Think of medical imaging software as a high-tech digital darkroom for the human body. It takes the raw, complex data captured by scanners—like MRIs, CTs, and X-rays—and develops it into crystal-clear images. These images are what doctors rely on to diagnose diseases, map out treatments, and track a patient's progress with incredible accuracy.
The Digital Bridge Between Scanners and Diagnoses

Imagine a state-of-the-art MRI or CT scanner as a camera taking millions of pictures inside the body. By itself, that information is just a jumble of numbers and signals, completely unreadable to us. This is where medical imaging software steps in, acting as the essential bridge between the scanner's raw data and a doctor's life-saving diagnosis.
The software crunches all that raw output and reconstructs it into detailed anatomical images. It gives clinicians a non-invasive window to peer inside the body, letting them examine organs, bones, and soft tissues with a level of detail that was once unimaginable. Without this crucial software, the full potential of modern scanning technology would be completely wasted.
Core Purpose and Functionality
At its core, the software is built to do a few things really well, all of which are vital for patient care. It gives medical professionals the power to see internal structures with stunning clarity—something that used to require invasive surgery.
But it’s not just about looking at a static picture. The software comes packed with tools that let doctors interact with and analyze the images on a much deeper level.
Here’s a quick rundown of what it enables:
- Diagnosing Conditions: Spotting everything from simple bone fractures to complex tumors and blockages in blood vessels.
- Planning Treatments: Giving surgeons the ability to create 3D models of a patient's anatomy to meticulously plan out a complex procedure before ever making an incision.
- Monitoring Progress: Tracking how well a treatment is working over time, like watching a tumor shrink in response to chemotherapy.
- Screening for Prevention: Catching diseases like breast or lung cancer in their earliest, most treatable stages.
The need for these precise diagnostic tools is exploding. The global market for medical imaging software was valued at around USD 7.6 billion and is expected to climb to nearly USD 13.93 billion by 2033. That kind of growth tells you just how central these systems have become in healthcare today.
The Universal Language of Imaging
For all of this to work seamlessly, there needs to be a common language. How do you make sure an image from a GE scanner can be opened and read perfectly on a system built by Siemens? The industry solved this with a universal standard.
A cornerstone of all medical imaging software is its compliance with the DICOM standard for medical imaging. This ensures that images and data can be handled consistently and shared between different devices and hospital systems without a hitch.
This standardization is what makes modern radiology possible. It means an X-ray taken at a small-town clinic can be instantly sent to a specialist at a major research hospital hundreds of miles away for a second opinion. This ability to share and collaborate is absolutely critical for effective patient care.
Ultimately, these platforms are far more than just fancy image viewers. They are the diagnostic command centers of modern medicine.
Exploring Different Medical Imaging Tools
Not all medical imaging is created equal. The same goes for the medical imaging software that brings those pictures to life. Each method—whether it's a CT scan, an MRI, or a simple X-ray—tells a very different story about what's happening inside the human body. The software is the storyteller, translating raw data into a clear narrative a clinician can read and act on.
Think of it like a photographer choosing the right lens. You wouldn't use a wide-angle lens for a detailed portrait, and you wouldn't use a macro lens to capture a landscape. In the same way, a cardiologist needs a different "lens" than a neurologist, and their software is built for that specific job.
To really get a feel for how these tools differ, it helps to see them side-by-side. Each has a job it's uniquely suited for, along with its own set of trade-offs.
Comparison of Medical Imaging Modalities
| Modality | Primary Use Case | Key Advantage | Main Limitation |
|---|---|---|---|
| CT | Trauma, bone fractures, tumor location | Excellent for dense structures (bone, organs) | Higher radiation exposure |
| MRI | Brain, spinal cord, soft tissue injuries | Unmatched detail in soft tissues; no radiation | Slower, more expensive, not suitable for all patients |
| Ultrasound | Obstetrics, cardiology, real-time guidance | Real-time imaging, safe (no radiation), portable | Operator-dependent, limited by bone/gas |
| X-ray | Bone fractures, chest (pneumonia), dental | Fast, inexpensive, widely available | 2D view, poor soft tissue detail, radiation |
| PET | Cancer detection, metabolic studies | Shows biological function, not just structure | Requires radioactive tracer, lower-resolution images |
This table gives a quick snapshot, but the real magic is in the software that powers each of these modalities.
Computed Tomography (CT) Software
CT software is the architect of the imaging world. It takes a series of X-ray images from dozens of different angles and digitally stitches them together, creating detailed, cross-sectional "slices" of the body. From there, clinicians can build intricate 3D models of bones, organs, and blood vessels.
Its main strength is visualizing dense structures with incredible clarity. This makes it a lifesaver in emergency rooms for assessing trauma, where quickly spotting internal injuries or bone fractures is everything. It's also a go-to for oncologists who need to know the exact size and location of a tumor.
Magnetic Resonance Imaging (MRI) Software
If CT is the architect, then MRI software is the master painter, capturing the rich, subtle details of soft tissues. Instead of X-rays, MRI uses powerful magnets and radio waves to generate images. This technique gives doctors an unparalleled view of the brain, spinal cord, muscles, and ligaments.
Because of this, MRI software is a cornerstone of neurology, helping diagnose conditions like strokes or multiple sclerosis. It’s also crucial in oncology for staging cancers in soft tissues and in orthopedics for examining joint and muscle injuries without any radiation exposure.
Ultrasound and X-ray Software
Ultrasound and X-ray are two of the most familiar and accessible imaging tools, and their software reflects that.
- X-ray Software: This is the original. The software is generally straightforward, designed to create 2D images of bones and chest cavities. It’s fast, effective, and the perfect tool for diagnosing a broken bone, pneumonia, or dental problems.
- Ultrasound Software: This software uses high-frequency sound waves to create live, moving images of the body’s internal structures. Its ability to show movement makes it essential in cardiology for watching the heart beat and in obstetrics for monitoring a developing fetus.
Market data shows some interesting shifts here. Ultrasound has long been the market leader, but others are catching up. Projections indicate that while Ultrasound's market share may dip slightly from 31% to 29% by 2025, both CT and MRI are set to grow. CT is expected to rise from 15% to 16%, and MRI from 12% to 14%. You can dig deeper into these modality trends and software statistics for a fuller picture.
Positron Emission Tomography (PET) Software
PET scan software offers a view that other tools simply can't: it visualizes the body's metabolic processes right down to the cellular level. Before a scan, a patient gets a small injection of a radioactive tracer. This tracer naturally accumulates in areas with high metabolic activity—like cancer cells.
PET software then detects the energy given off by this tracer, creating images that make these "hot spots" light up. This makes it an incredibly powerful tool in oncology for finding cancer, checking if it has spread, and seeing if a treatment is actually working.
Each of these software platforms comes with its own set of capabilities and performance benchmarks.
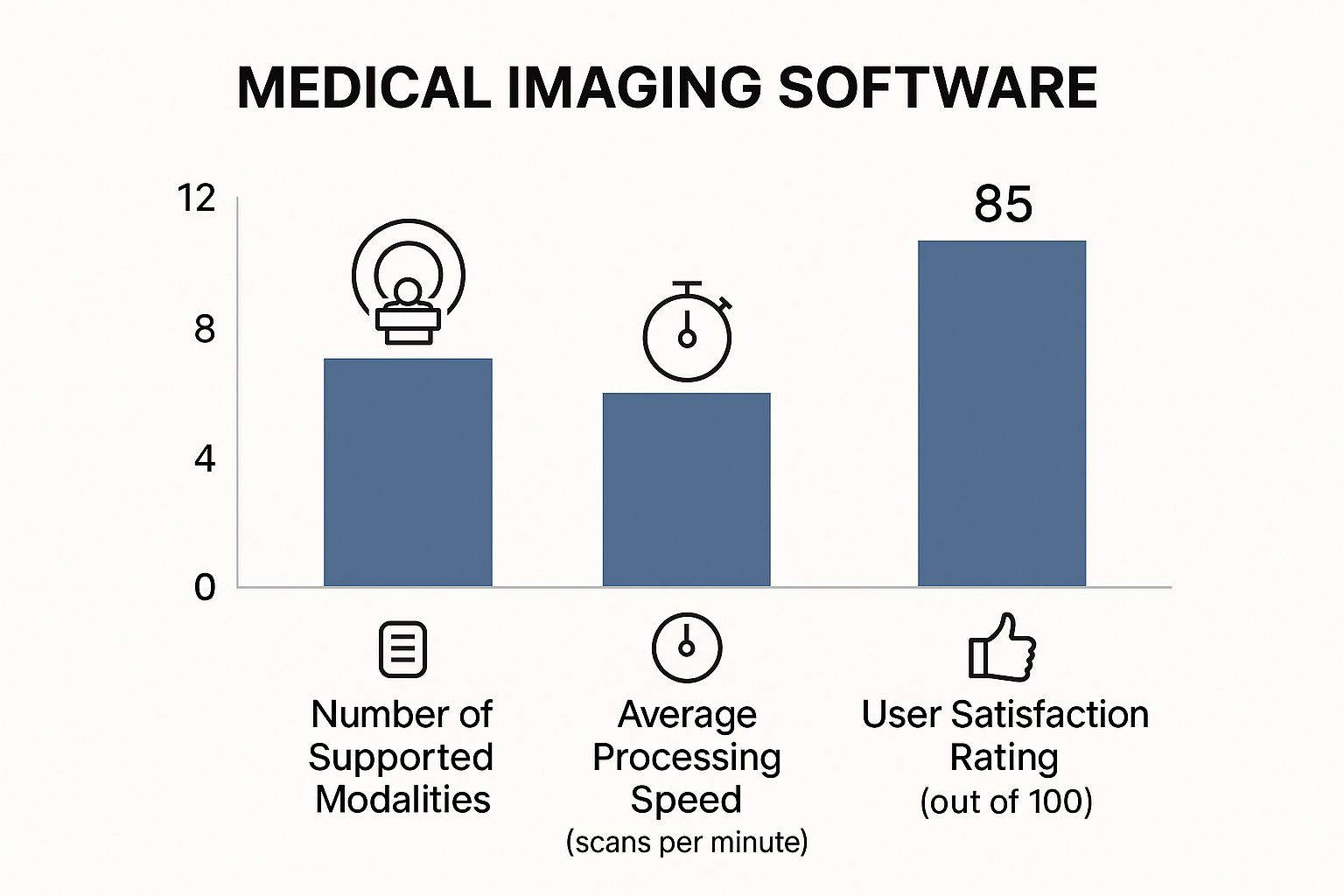
As the data shows, there's often a trade-off. Platforms that support more modalities might be a bit slower, while highly specialized software often leads the pack in speed and user satisfaction. It all comes down to finding the right tool for the job.
What Really Makes Modern Imaging Software Tick?

While the big scanners like CT and MRI often steal the spotlight, the real diagnostic magic happens inside the medical imaging software itself. It’s a mistake to think of this software as just a simple image viewer. A better analogy is a digital workbench, fully loaded with specialized tools that a clinician uses to transform flat, grayscale images into an interactive, detailed map of a patient's body.
Today's platforms are expected to do much more than just put a picture on a screen. They need to deliver a complete suite of functions for deep analysis, precise measurement, and easy collaboration. These features are the bedrock of a confident diagnosis, helping professionals get to the right answer faster and with greater accuracy.
Advanced Visualization and Manipulation
The most basic—and most essential—feature is the ability to truly see and interact with images from every possible angle. Simple 2D viewing is just the first step. The real value comes from the dynamic tools that bring the data to life.
- 2D Viewing: This is the classic slice-by-slice view you might imagine. It’s fundamental for an initial review and the standard way to interpret scans like X-rays or a series of CT images.
- Multi-Planar Reconstruction (MPR): This is a brilliant tool. It lets a clinician take a stack of 2D images, say from a CT scan, and instantly rebuild them into different anatomical views—coronal, sagittal, and axial. It’s like having the power to digitally re-slice the body from any direction you want, all without needing another scan.
- 3D Volume Rendering: This is where the software constructs a full three-dimensional model of an organ, bone structure, or vascular network. Surgeons lean on this heavily to plan out complex procedures, rotating the model to get a feel for spatial relationships long before they make the first incision.
These visualization tools aren't just for show. The ability to inspect a tumor from every conceivable angle or trace a complex fracture in 3D provides a level of insight a flat 2D image could never match. This comprehensive perspective is a game-changer for both diagnostic certainty and surgical planning.
Precision Measurement and Enhancement Tools
Looking at images is one thing; quantifying what you see is another. This is where measurement and enhancement tools become absolutely critical, adding a layer of objective data to what can be a subjective interpretation.
Image enhancement functions are like a digital magnifying glass. They let users fine-tune brightness, contrast, and sharpness to pull subtle details out of the shadows. This small adjustment could be the very thing that helps a radiologist spot a tiny nodule or a faint fracture line that might have otherwise gone unnoticed.
Measurement tools are just as important, especially for tracking how a disease is progressing over time. These can range from simple tools for measuring distance and angles to more complex calculations, like the volume of a lesion or the percentage of blockage in a blood vessel. Having consistent, accurate measurements is the only way to know for sure if a treatment is working.
The ability to precisely measure anatomical structures and abnormalities over time is non-negotiable. It transforms a qualitative observation ("the tumor looks smaller") into a quantitative fact ("the tumor has decreased in volume by 15%"), providing concrete evidence for clinical decisions.
Seamless Integration and Compliance
Even the most powerful imaging software is useless if it’s isolated. It has to talk to the rest of the hospital's technology ecosystem to make sure data gets from the scanner to the patient's record securely and without a hitch.
This is where two key standards come into play:
- PACS Integration: A hospital's Picture Archiving and Communication System (PACS) is its digital library for all medical images. The software must plug directly into the PACS, allowing doctors to pull up a patient's entire imaging history in seconds. This prevents delays and gives them the full story.
- DICOM Compliance: DICOM (Digital Imaging and Communications in Medicine) is the universal language for medical imaging. Being DICOM compliant ensures that images and data from any manufacturer's equipment can be opened and analyzed on any software that also follows the standard. This interoperability is the backbone of modern radiology, preventing departments from getting locked into one vendor and making it easier for different hospitals to share information.
Without these two foundational pieces, all the fancy visualization features in the world wouldn't matter. They are the connective tissue that holds the entire diagnostic workflow together, ensuring the right information gets to the right person, right when they need it.
How AI Is Changing the Game in Medical Imaging
https://www.youtube.com/embed/mbjXXvsa5I8
The biggest shift happening in medical imaging right now isn't a new kind of scanner—it's the quiet but powerful integration of Artificial Intelligence. This isn't some futuristic sci-fi concept; AI is a real tool working alongside clinicians today, fundamentally changing how they interpret diagnostic images. It's becoming an essential partner, making the entire process more accurate and efficient.
Imagine an AI algorithm as a radiologist who has already seen and flawlessly analyzed millions of scans. It has trained itself to spot the most subtle patterns and abnormalities that signal disease—some so faint that they could easily be missed by the human eye at the end of a long day. This digital assistant never gets tired or distracted. It just applies its massive "experience" to every image it sees.
Supercharging Diagnostic Accuracy
One of the most immediate benefits of AI is how it acts as a second set of eyes for the clinician. These systems are trained on enormous datasets of medical images, teaching them to pinpoint specific conditions with incredible precision. This is a huge deal, especially when it comes to catching diseases in their earliest stages when the signs are barely there.
For instance, an AI tool can automatically flag a tiny, suspicious lung nodule on a CT scan or highlight a subtle area of concern on a mammogram. The software isn't making the final call—that's still the doctor's job. Instead, it acts as a safety net, directing attention to spots that need a closer look and dramatically lowering the chance of a critical finding being missed.
AI isn't here to replace expert clinicians. It's here to augment them. By taking on the repetitive, data-heavy analysis, it frees up physicians to focus on complex patient cases, treatment planning, and the human side of medicine where their expertise is irreplaceable.
This partnership between human and machine is proving to be a powerful formula for better patient outcomes.
Making Workflows Smarter and Faster
AI isn't just about analyzing the pictures themselves; it's also about streamlining the entire diagnostic process. In a busy hospital's radiology department, there might be hundreds of scans in the queue. AI-powered medical imaging software can intelligently sort through this list, pushing the most critical cases right to the top.
An algorithm can instantly analyze a head CT from the emergency room, and if it detects signs of a potential brain bleed, it flags that scan for immediate review. This simple prioritization can shave minutes—or even hours—off the time it takes to get a diagnosis and start treatment, which can be the difference between life and death in acute situations.
This intelligent automation helps in other ways, too:
- Automated Measurements: AI can perform routine tasks like calculating a tumor's volume or a heart's ejection fraction with perfect consistency, saving valuable time.
- Report Generation: It can draft preliminary reports by summarizing key findings, giving the radiologist a solid starting point to review, edit, and finalize.
- Predictive Analytics: Some advanced AI models can even look at a single scan and help predict how a disease might progress, giving doctors incredible foresight.
The money and effort being poured into this technology show just how much potential it has. The global AI in medical imaging market, valued at USD 1.28 billion, is expected to hit USD 1.67 billion soon and is projected to skyrocket to around USD 14.46 billion by 2034. That’s a compound annual growth rate of roughly 27.10%, showing massive industry confidence.
On top of that, new tools like AI agents for medical research are now helping researchers analyze huge datasets, including information pulled from medical images. This rapid growth makes one thing clear: AI is here to stay, and it's making a real-world impact.
How to Choose the Right Medical Imaging Software

Picking the right medical imaging software isn't just a purchase; it's a major investment that will shape your clinical efficiency and patient care for years to come. Think of it less like buying an app and more like installing the central nervous system for your imaging department. Get it right, and you’ll create a seamless, connected workflow. Get it wrong, and you're looking at bottlenecks, frustrated staff, and a whole lot of operational headaches.
This decision demands a structured approach that goes way beyond a simple feature-for-feature comparison. Healthcare providers and IT teams need to look at the whole picture, from daily usability to how well the investment will hold up over time. Having a clear framework is the only way to cut through the noise in a crowded market and find the perfect fit for your specific clinical needs.
Start By Assessing Your Core Needs and Workflow
Before you even glance at a vendor’s website, the first step is to look inward. What specific problems are you actually trying to solve? The needs of a small orthopedic clinic are worlds apart from those of a large hospital's multi-specialty oncology department.
Begin by mapping out your current imaging workflow from start to finish. Where do things slow down? What tasks are eating up your staff's valuable time? Pinpointing your unique pain points helps build a concrete list of "must-have" features versus "nice-to-have" extras.
The goal is to find software that bends to your workflow, not the other way around. A platform that shines in a demo but forces you to overhaul proven processes will struggle with user adoption and never deliver its full value.
Here are a few key questions to ask your team:
- What imaging modalities do we use now, and what might we add in the next five years?
- How many people will need access, and what are their distinct roles (radiologist, technician, referring physician)?
- What are our absolute requirements for sharing images with specialists or facilities outside our network?
Prioritize Integration and Scalability
Modern healthcare is an ecosystem of interconnected systems. No piece of software can work in isolation. Your chosen medical imaging platform has to be a team player, capable of communicating perfectly with the other critical systems you rely on.
Integration with your Electronic Health Record (EHR) system is absolutely non-negotiable. A smooth connection ensures imaging studies are automatically tied to the correct patient file, building a complete, unified health history. This simple link eliminates tedious manual data entry, slashes the risk of errors, and gives clinicians immediate access to the full story.
Scalability is just as crucial. Your practice or hospital is going to grow and change, and your software must be ready to grow with it. A scalable solution can handle a rising volume of studies, support more users, and adapt to new imaging technologies without needing a complete and costly replacement. Thinking ahead prevents you from being trapped in a system that can't keep up just a few years down the road.
Evaluate User Experience and Vendor Support
The most powerful software on the planet is worthless if your staff finds it clunky or confusing. A clean, intuitive user interface is essential for getting your team on board quickly and maintaining efficiency for the long haul. When you're evaluating options, insist on hands-on demos for the clinicians, technicians, and administrators who will live in this system every single day.
Their feedback is gold. A system that feels logical to them will naturally lead to fewer mistakes and a smoother day.
Finally, look beyond the software and size up the vendor. You’re looking for a long-term partner, not just a seller. Dig into their training programs, check the responsiveness of their customer support, and review their history of providing timely updates and security patches. A strong support system is your safety net, ensuring any hiccup is resolved fast with minimal disruption to patient care.
Choosing the right software involves weighing many factors, from technical specifications to user-friendliness. This checklist can help you organize your evaluation process and make a more informed decision.
Software Selection Checklist
| Evaluation Criteria | Key Questions to Ask | Importance (High/Medium/Low) |
|---|---|---|
| Workflow & Needs Alignment | Does the software address our specific pain points (e.g., slow reporting, difficult image sharing)? Does it match our current and future workflow? | High |
| EHR/HIS Integration | Is there proven, seamless integration with our current EHR/HIS system? What is the integration process like? | High |
| Scalability | Can the system easily handle a 50% increase in study volume? Can we add new users, locations, or modalities without major upgrades? | High |
| User Experience (UX) | Is the interface intuitive for radiologists, technologists, and administrative staff? Can key tasks be completed in just a few clicks? | High |
| Vendor Support & Training | What are the support hours and guaranteed response times? Is the training comprehensive and offered on-site or online? | High |
| DICOM & HL7 Compliance | Is the software fully compliant with the latest DICOM and HL7 standards to ensure interoperability? | High |
| Security & Compliance | Does the platform meet all HIPAA requirements? What are the data encryption, backup, and disaster recovery protocols? | High |
| Advanced Features | Does it offer the specific tools we need (e.g., 3D reconstruction, AI-powered analysis, teleradiology features)? | Medium |
| Total Cost of Ownership | What is the complete cost, including licensing, implementation, training, support, and potential hardware upgrades? | Medium |
| Vendor Reputation | What do current customers say about the vendor? Can they provide references from similar-sized organizations? | Medium |
By systematically working through these criteria, you can move beyond the sales pitches and focus on what truly matters for your practice. This structured approach helps ensure your final choice is a strategic one that empowers your team and enhances patient outcomes.
Common Questions About Medical Imaging Software
Diving into the world of medical imaging software can feel overwhelming. The technology is complex, the acronyms are endless, and the stakes couldn't be higher. To cut through the noise, let's tackle some of the most common questions people have, breaking down the essentials in a straightforward way.
Getting a firm grasp on these details is vital for anyone involved in choosing, rolling out, or using these critical healthcare tools. From security protocols to the core differences between key systems, clarity here ensures you’re making smart decisions that help both your clinical team and your patients.
What Is the Difference Between PACS and RIS?
It's incredibly common to mix up PACS and RIS. They work hand-in-hand, but they have completely different jobs. Here’s a simple way to think about it: the PACS is the high-tech library where all the images are stored, while the RIS is the front desk that manages the whole patient journey.
-
A PACS (Picture Archiving and Communication System) is all about the pictures. Its main purpose is to store, retrieve, manage, and display the medical images themselves—the X-rays, CT scans, and MRIs. Think of it as the secure digital vault for all visual data.
-
A RIS (Radiology Information System) acts as the department's operational command center. It handles the administrative side of things, like scheduling patient appointments, managing billing, and generating the final radiology reports. It tracks the patient's entire workflow from check-in to follow-up.
So, while the RIS tells the story of the patient's visit, the PACS provides the visual evidence. They are two distinct systems, but for a radiology department to run smoothly, they have to communicate perfectly.
How Is Patient Data Kept Secure?
In the medical world, keeping patient data secure isn't just a good idea—it's a legal and ethical requirement, heavily enforced by regulations like HIPAA (Health Insurance Portability and Accountability Act). To protect this sensitive information, modern software systems build a digital fortress using multiple layers of defense.
The goal is to safeguard data at every single stage, from the moment it's created to when it's being stored or viewed. It’s never about just one password; it's about a whole system of technical checks and balances working together.
Security in medical imaging isn't a "set it and forget it" feature. It's an active, ongoing process that requires constant vigilance and layered defenses to ensure confidential patient health information stays exactly that—confidential.
Here are some of the key security measures you'll always find:
- Strong User Authentication: Verifies that only authorized staff can even get into the system.
- Role-Based Access Controls: This is a big one. It means users can only see and do what's necessary for their specific job. A technician might upload a scan, but only a radiologist can officially sign off on the report.
- End-to-End Data Encryption: This scrambles the information both when it's stored on a server (at rest) and when it's sent over a network (in transit). To an outsider, it's just unreadable code.
- Comprehensive Audit Trails: The system keeps a detailed log of every action taken. It records who accessed what data, and when, creating accountability and making it easy to spot unusual activity.
Are Cloud Solutions Better Than On-Premise Servers?
This is a classic "it depends" scenario. There’s no single right answer, because the best choice comes down to a facility's unique budget, IT capabilities, and workflow needs. Both on-premise servers and cloud solutions have clear pros and cons.
An on-premise server is just what it sounds like—the physical hardware lives inside your facility. This setup gives you total, hands-on control over your data and infrastructure. The downside? It demands a huge upfront investment in equipment and a dedicated, expert IT team to maintain it all.
A cloud-based solution, on the other hand, means you store your imaging data on secure, remote servers managed by a specialized company. This approach has a much lower initial cost, makes it easy to scale up as you grow, and offers the flexibility of remote access. The provider handles all the security updates and maintenance, but you’ll have ongoing subscription fees and need a rock-solid internet connection. Many organizations are even moving to a hybrid model to get the best of both worlds.
Why Is DICOM Compliance So Important?
DICOM (Digital Imaging and Communications in Medicine) is, quite simply, the universal language of medical imaging. It's the global standard that allows a CT scanner from one manufacturer to talk to a software viewer from a completely different one.
Without it, chaos would ensue. An image taken on a Siemens machine might be unreadable on a GE workstation. This would create massive data silos, cripple collaboration between hospitals, and lock institutions into a single vendor for all their equipment.
DICOM compliance is the solution. It guarantees interoperability, which means medical images and all their related data can be shared, viewed, and analyzed correctly on any system that follows the standard, anywhere on the planet. This is non-negotiable for modern healthcare, as it enables critical tasks like:
- Sending a complex case to a specialist at another hospital for a second opinion.
- Integrating a new, state-of-the-art MRI machine without having to rip out your entire software system.
- Ensuring that patient imaging histories remain accessible and readable for decades, no matter how technology evolves.
DICOM is the foundational glue that holds the entire digital imaging ecosystem together.
At PYCAD, we build the specialized AI that powers the next generation of medical imaging software. We partner with medical device companies to sharpen diagnostic accuracy and streamline workflows through our expertise in data handling, model training, and deployment. Learn how our customized AI services can elevate your technology.






