Imagine trying to understand a complex, multi-layered cake just by looking at the outside. It’s impossible, right? You’d need to cut a slice to see what’s really going on inside. Cross section analysis in medicine works on the same principle, letting doctors see detailed 'slices' of the human body without ever making an incision.
Unveiling the Inner Body Through Digital Slices
At its heart, cross section analysis is a non-invasive way to look deep inside the body. Technologies like Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are the workhorses here. They capture a series of 2D images, with each one representing a very thin slice of a specific body part.
When you stack these individual slices together in order, they create a complete and incredibly detailed picture. This process gives clinicians a clear view of organs, bones, blood vessels, and soft tissues, letting them find problems with stunning accuracy. It's really the idea that modern diagnostics is built on.
Why Are These Slices So Important?
The real magic of cross section analysis is its ability to isolate and examine structures that would otherwise be hidden. Think about a standard X-ray. It gives you a flat image where bones and organs are layered on top of each other, which can sometimes make it tough to see what’s truly going on.
Cross-sectional views get rid of that overlap. They provide a clean, unobstructed perspective of each layer. This level of clarity is critical for a whole host of medical tasks:
- Pinpointing a Diagnosis: It helps identify the exact location, size, and shape of tumors, injuries, or other abnormalities.
- Planning Treatment: Surgeons can map out a complex procedure beforehand, and radiation oncologists can precisely target cancer cells while avoiding healthy tissue.
- Monitoring Health: Doctors can track how a condition is progressing or see how well a patient is responding to a new treatment.
This method essentially turns a confusing diagnostic puzzle into a manageable, layer-by-layer investigation.
By translating complex anatomy into a series of clear, digestible images, cross section analysis provides the crucial insights needed for confident clinical decision-making.
From 2D Slices to 3D Understanding
While each 2D slice is valuable on its own, their true power comes when they're combined. Using sophisticated software, these individual images can be digitally stitched back together to create a full, three-dimensional model of the scanned area.
This reconstructed 3D view isn't static. A doctor can rotate it, zoom in, and even virtually dissect it. This gives them a complete spatial understanding of the patient’s unique anatomy. It’s not just about seeing inside the body anymore; it's about understanding it in a way that leads to effective, and often life-saving, treatment.
How Medical Imaging Tech Slices Through the Body

To really get a feel for what cross-section analysis can do, you have to understand how these incredible images are made in the first place. Each imaging technology—or modality, as we call it in the field—has a unique way of peering inside the body. Think of it like a specialist's toolkit; you wouldn't use a hammer to turn a screw, and you wouldn't use the same imaging for bone as you would for brain tissue.
These machines don't just snap a single photo. They collect massive streams of data that a computer then meticulously rebuilds into the anatomical "slices" doctors examine. This method of capturing a single moment in time to compare different variables is a powerful concept used well beyond medicine. Market researchers, for example, use it to get an immediate snapshot of consumer habits across different groups.
Computed Tomography: The High-Speed Architect
When speed and detail are critical, especially in an emergency, Computed Tomography (CT) is the go-to. Picture a camera on a circular track, spinning around you and taking hundreds of pictures from every angle in just seconds. That's essentially what a CT scanner does.
The machine uses a rotating X-ray beam and a series of detectors to capture these "snapshots" as the patient moves through the machine's opening. A powerful computer then stitches all those individual angles together to create those detailed cross-sectional images.
Because CT is based on X-rays, it’s brilliant at picking up differences in tissue density. This makes it the undisputed gold standard for:
- Bone Fractures: Showing even the most complex breaks with incredible clarity.
- Internal Bleeding: Quickly spotting life-threatening bleeds in the brain or abdomen after an accident.
- Cancer Detection: Pinpointing and measuring tumors in organs like the lungs and liver.
The sheer speed and precision of CT give doctors the immediate answers they need to save lives.
Magnetic Resonance Imaging: The Soft Tissue Expert
If CT is the architect of the body’s hard structures, then Magnetic Resonance Imaging (MRI) is the master painter of its soft tissues. Instead of radiation, MRI uses a massive magnet and radio waves to generate its images. The process works by getting the hydrogen atoms in your body—which are abundant in water and fat—all riled up.
Once the radio waves stop, these atoms relax and send out energy signals that the MRI scanner picks up. Different tissues contain different amounts of water, so they release unique signals. The scanner translates this symphony of signals into images with breathtaking contrast and detail.
MRI gives us a view of the body's soft tissues that is simply in a class of its own, revealing subtle problems that other imaging techniques would completely miss.
This unique ability makes MRI essential for looking at:
- The Brain and Spinal Cord: Finding tumors, signs of multiple sclerosis, or herniated discs.
- Joints and Ligaments: Visualizing tears in cartilage, tendons, or ligaments with pinpoint accuracy.
- Muscles and Organs: Checking for damage or disease in places like the heart and liver.
An MRI scan takes a bit longer than a CT, but for soft tissue analysis, the level of detail it provides is second to none.
Comparing Core Cross-Sectional Imaging Modalities
To make sense of when to use which technology, it helps to see them side-by-side. Each modality has its own strengths, making it the right tool for a specific job.
| Modality | Imaging Principle | Best For Visualizing | Key Advantage |
|---|---|---|---|
| CT | Uses X-rays from multiple angles to create detailed slices. | Dense structures like bone, internal organs, and blood vessels. | Speed and precision, ideal for trauma and emergencies. |
| MRI | Uses magnetic fields and radio waves to map hydrogen atoms. | Soft tissues like the brain, muscles, ligaments, and tendons. | Exceptional soft tissue contrast without using radiation. |
| PET | Injects a radioactive tracer to detect metabolic activity. | Functional processes, especially cancer cell activity. | Shows biological function, not just anatomy. |
| Ultrasound | Uses high-frequency sound waves that bounce off tissues. | Organs in motion, fluid-filled structures, and fetal development. | Real-time imaging, non-invasive, and no radiation. |
This comparison highlights why having a range of imaging tools is so crucial for modern diagnostics. It allows clinicians to tailor the exam to the specific clinical question at hand.
Other Key Imaging Players
Beyond CT and MRI, a few other technologies play huge roles. Positron Emission Tomography (PET) gives us a completely different kind of picture—one of function, not just form. By using a radioactive tracer, it lights up areas with high metabolic activity, which is a game-changer for finding aggressive cancer cells.
Ultrasound, on the other hand, uses sound waves to create live images. It’s safe, portable, and perfect for looking at organs in motion, guiding needles for biopsies, or checking on a developing baby. And the innovation doesn't stop; exciting new breakthroughs in imaging are constantly emerging from fields like military medical photonics research and development, promising to give us even more powerful tools in the future.
Each of these technologies adds a unique piece to the diagnostic puzzle, empowering clinicians to pick the perfect tool for the job. This ensures that every cross-section analysis delivers the most accurate and relevant information possible for patient care.
A Patient's Journey Through a Cross-Sectional Scan
Stepping into a hospital for a CT or MRI can be a bit daunting. The big machines and clinical setting can feel overwhelming, but knowing what to expect can make the whole experience feel much more manageable. The journey through a cross section analysis is a carefully choreographed process, fine-tuned for accuracy and patient safety, that takes you from initial prep all the way to a final diagnostic report.
It actually starts well before you even see the scanner. Your doctor will provide you with a specific set of instructions based on the type of scan you're having.
Preparing for a Clearer Picture
For some scans, you might need to fast for a few hours. This is pretty standard for abdominal imaging because an empty digestive system reduces visual "noise" and helps create a much sharper picture of your organs.
In many situations, a contrast agent is used to make specific tissues or blood vessels pop. This is a special dye you might drink or have injected into a vein. For instance, a contrast-enhanced CT of the chest can light up the pulmonary arteries, making it much easier for a radiologist to spot something like a blood clot. It’s a crucial step for adding an extra layer of detail and clarity.
Inside the Scanning Room
Once you're prepped, a technologist will bring you into the scanning room and help you get comfortable on a motorized table. This table will then gently slide into the center of the scanner—that big, doughnut-shaped machine. The technologist runs everything from an adjoining room, but they can see you and talk to you through an intercom the entire time.
The most important thing during the scan is to stay as still as you can. Think of it like taking a photograph with a slow shutter speed; even tiny movements can blur the final images. The tech might ask you to hold your breath for a few seconds at a time, especially for chest or abdomen scans, to get the absolute crispest pictures. You’ll hear some whirring and clicking as the machine works its magic, capturing hundreds or even thousands of individual image slices.
The entire scan is a partnership between you and the technology. Your stillness is what provides the clean, high-quality data that forms the very foundation of an accurate diagnosis.
From Slices to a 3D Model
After the scan is over, your part is finished, but for the imaging team, the real work is just getting started. The raw data from the scanner is basically a huge stack of 2D cross-sectional "slices." This is where some serious computing power comes into play.
This graphic gives a great overview of the workflow, from capturing the raw data to the final interpretation.
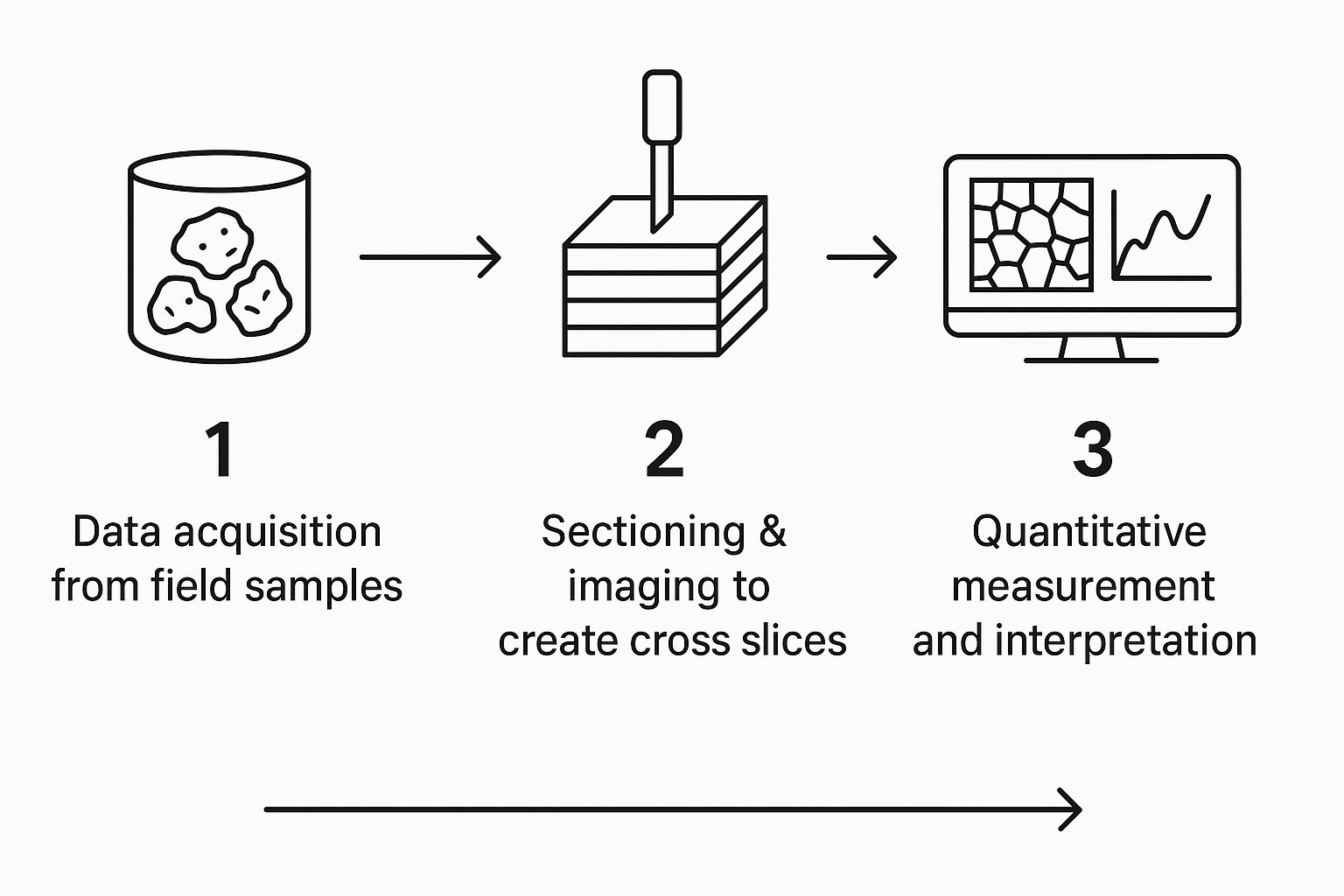
As you can see, the process flows from data acquisition to imaging and, finally, to measurement—turning a stream of information into medical insight.
Sophisticated software gets to work on what's called image reconstruction. It digitally stacks all those 2D slices in the exact right order, almost like putting a loaf of bread back together slice by slice. The software then intelligently fills in the gaps between each one to build a seamless and incredibly detailed 3D model of your anatomy.
This 3D model is a game-changer. A surgeon can rotate it to map out the best way to perform a procedure, or a radiologist can zoom in to measure the precise dimensions of a tumor. This ability to go from flat pictures to a dynamic digital model is at the heart of modern cross section analysis.
The final piece of the puzzle is the radiologist—a doctor who specializes in interpreting medical images. They meticulously examine every slice and the 3D model before writing a detailed report for your doctor. And with that, your journey from scan to diagnosis is complete.
How AI Is Supercharging Cross Section Analysis
Artificial intelligence is stepping in as a powerful collaborator in medical imaging, turning the meticulous process of cross section analysis into a faster, smarter, and more insightful diagnostic tool. Think of a radiologist as a highly skilled detective, carefully piecing together clues from hundreds of image slices. AI is like their brilliant new assistant, one that can instantly sift through mountains of data and point out the most suspicious evidence.
This isn't about replacing the expert in the room. It’s about augmenting their skills, helping clinicians manage overwhelming workloads and focus their attention where it's truly needed. We train machine learning algorithms on vast, anonymized libraries of CT and MRI scans, teaching them to recognize the subtle patterns, textures, and anomalies that hint at potential health problems.
Automating the Grind and Boosting Efficiency
One of the most immediate benefits of AI is how it handles the time-consuming, repetitive parts of the job. For instance, an AI model can precisely segment and measure a tumor's volume across dozens of cross-sectional slices in mere seconds. That’s a task that could easily take a human expert a significant amount of time.
This speed isn't just a matter of convenience; it’s a critical factor in patient outcomes. Faster analysis leads to quicker diagnoses, which means treatment can start sooner. By taking over the laborious aspects of image analysis, AI frees up radiologists to concentrate on complex case interpretation, collaborating with other physicians, and consulting directly with patients.
By taking on the heavy lifting of measurement and segmentation, AI acts as a powerful efficiency multiplier, allowing medical experts to work at the top of their license and deliver more focused, high-value care.
Uncovering What the Human Eye Might Miss
Beyond just doing things faster, AI brings a new level of analytical depth to the table. Machine learning models can detect incredibly subtle patterns in image data that are often invisible, or at least not obvious, to the human eye. This is a game-changer for early disease detection, where the first signs of a condition can be minuscule.
Here are a few real-world examples of this in action:
- Early Cancer Detection: An AI algorithm analyzing a chest CT scan can flag a tiny, suspicious lung nodule that might have been missed during a routine review.
- Cardiovascular Risk Assessment: From a cardiac scan, AI can automatically calculate the exact volume of plaque buildup in coronary arteries, giving a precise, quantitative measure of a patient's risk for heart disease.
- Neurological Analysis: In brain imaging, AI helps quantify changes in brain volume over time, offering critical data for tracking the progression of diseases like Alzheimer's.
This ability to quantify and track changes with superhuman precision empowers a much more proactive and personalized approach to medicine.
It All Comes Down to the Data
The power of any AI in medical imaging comes down to the quality and quantity of the data it's trained on. This principle isn’t unique to healthcare, of course. Cross-sectional data is also invaluable in fields like econometrics for evaluating relationships between variables at a single point in time, which influences everything from public health policy to market research. Economists, for example, use these datasets to measure income inequality across thousands of households, while health officials analyze them to get an efficient snapshot of a population's health. You can learn more about these broader applications from resources like Econometrics Tutor.
In much the same way, a robust medical AI is built on a diverse foundation of images from patients with different conditions, ages, and backgrounds. This comprehensive training allows the algorithm to learn the full spectrum of what "normal" looks like and, more importantly, what deviates from it. The result is an analytical tool that is both powerful and reliable.
As AI models continue to learn from ever-expanding datasets, their accuracy and usefulness in cross section analysis will only get better. The goal is a future where AI and human experts work in a seamless partnership, blending computational power with clinical wisdom to deliver the best possible diagnosis for every single patient.
Cross Section Analysis in Everyday Clinical Practice
The real magic of cross section analysis isn't in the technology itself, but in how it touches individual lives. In hospitals and clinics everywhere, these detailed peeks inside the human body are far more than just diagnostic images; they're the bedrock of modern medical decisions. They give doctors the clarity they need to pick the right treatment, a choice that can completely change a patient's outcome.
From a chaotic emergency room to a quiet oncology ward, cross-sectional imaging tells a story. It might be the story of a life saved from a sudden crisis, a complex injury being put back together, or a chronic disease managed with pinpoint accuracy.
Let's look at how this plays out in a few key medical specialties.
Oncology: Precision Cancer Staging and Treatment
For any oncologist, knowing the exact stage of a cancer is everything. It dictates the entire treatment plan and helps set realistic expectations for the patient. This is where cross section analysis is absolutely essential.
Think about a patient who just found out they have lung cancer. A simple chest X-ray might have shown a suspicious spot, but it can't tell the whole story. That's when a PET/CT scan comes in, providing a series of detailed slices that reveal a massive amount of information. The CT part maps out the tumor's exact size and location, while the PET scan lights up areas of high metabolic activity—showing where the cancer is most aggressive.
By poring over these slices, an oncologist can answer critical questions:
- Tumor Size and Invasion: Is the tumor pushing into the chest wall or wrapping around major blood vessels?
- Lymph Node Involvement: Has the cancer spread into the nearby lymph nodes?
- Metastasis: Are there any signs of cancer in distant organs, like the liver or bones?
This level of detail allows the medical team to design a highly specific treatment plan, whether it's targeted radiation, surgery, or chemotherapy. The same analysis is then repeated over time to see exactly how well the tumor is responding.
Neurology: Diagnosing a Stroke in Minutes
When someone comes into the ER with stroke symptoms, every single second is critical. The brain isn't getting oxygen, and the faster doctors can restore blood flow, the better the chances of avoiding permanent damage. In this high-pressure situation, the speed and clarity of cross section analysis can be the difference between life and death.
A non-contrast CT scan of the head is always the first, most crucial step. It takes just a few minutes to get a series of axial "slices" of the brain, and its primary job is to determine what kind of stroke it is.
In the high-stakes environment of stroke care, a CT scan provides the definitive fork in the road, instantly guiding clinicians toward the right treatment path and preventing catastrophic errors.
A radiologist looking at the cross-sectional images can see immediately if there's any bleeding in the brain (a hemorrhagic stroke). If there's no blood, it's almost certainly an ischemic stroke, which is caused by a clot. This distinction is vital because the treatments are complete opposites. Giving a clot-busting drug to someone with a brain bleed would be fatal. Thanks to this quick analysis, the right treatment can start right away, preserving brain function and saving lives.
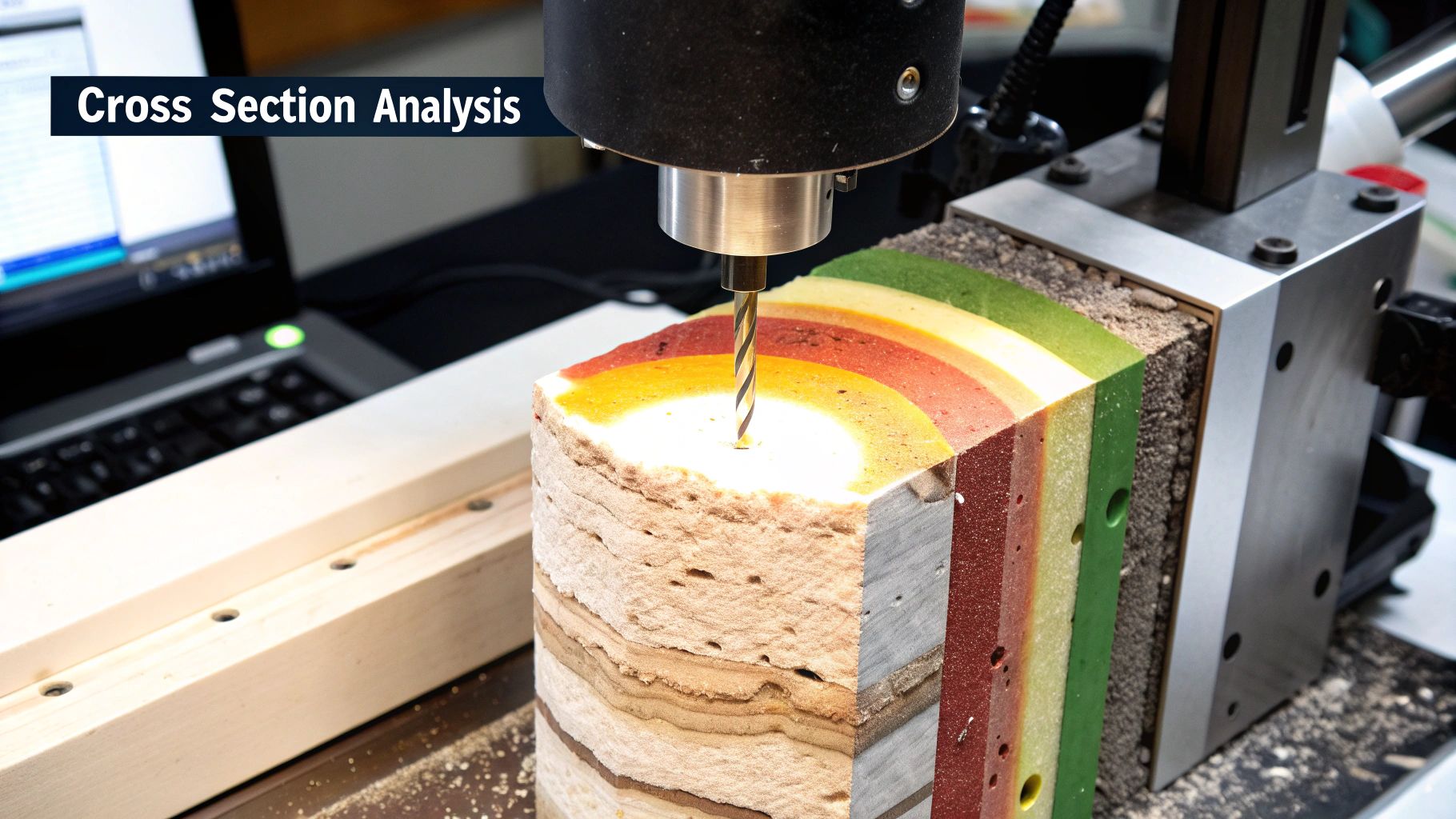
Orthopedics: Creating a Surgical Roadmap
For an orthopedic surgeon, fixing a badly broken bone is like putting together a complex 3D puzzle. A flat, two-dimensional X-ray just doesn't provide enough detail to understand how all the fragments are positioned, especially in tricky joints like the wrist or ankle. A CT scan, on the other hand, gives them the three-dimensional view they need.
Imagine a patient who shattered their ankle in a bad fall. The CT scanner produces hundreds of thin, cross-sectional images of the joint. Special software then stitches these slices together into a detailed 3D model that the surgeon can spin around and inspect from every possible angle. This virtual roadmap allows the surgeon to:
- See the precise number and location of every single bone fragment.
- Check for damage to the joint surface, which could cause arthritis down the line.
- Plan the exact placement for plates and screws long before the patient is even in the operating room.
This kind of detailed pre-operative planning, all made possible by cross section analysis, results in more accurate repairs, shorter surgeries, and much better long-term outcomes for the patient.
Interestingly, while medical imaging looks at physical structures, the principles of cross-sectional data are used in other fields to understand complex systems, like how investor behavior shapes global markets. One study found that the proportion of a country's stock market held by US investors could explain about 40% of the variation in its return correlations with the US market. It’s a great example of how cross-sectional data reveals hidden connections. You can learn more about this financial research from the University of Cambridge.
Common Questions About Cross-Sectional Imaging
Even with a good handle on the basics, some practical questions always pop up about cross-sectional imaging and its role in medicine. It's a field full of nuances, so let's clear up a few of the most common points of confusion.
We'll tackle the key differences between analysis types, talk candidly about safety, and demystify how those stunning 3D models come to life from a series of flat images.
Cross-Sectional Versus Longitudinal Analysis
One of the first things people ask is, "What's the real difference between cross-sectional and longitudinal analysis?" It all comes down to one simple concept: time.
Think of a cross-sectional analysis as a high-resolution photograph. It captures a detailed snapshot of a patient’s anatomy at one specific moment. For example, a radiologist uses a CT scan to measure a tumor's exact size and shape on a Tuesday morning. This gives them a complete picture of the situation right now.
Longitudinal analysis, on the other hand, is more like a movie. It’s about tracking the same patient over a period of time, collecting images at different points to see how things change. That same tumor might be scanned again in three months, and then again six months later. By comparing these sequential images, the doctor is performing a longitudinal analysis to see if the tumor is growing, shrinking, or just staying put.
Cross-sectional gives you the "what is," a deep dive into a single point in time. Longitudinal tells you "what's happening," revealing the story of change over weeks, months, or years.
Both are absolutely vital. An initial diagnosis often leans heavily on that first, precise cross-sectional view. But long-term treatment and management depend on the story that a longitudinal perspective tells.
Understanding the Risks of Imaging Scans
Patient safety is paramount, so it's only natural to have questions about the risks involved with medical scans. The answer really depends on the specific technology being used.
Some technologies, like CT and PET scans, use ionizing radiation. This comes with a very small, cumulative risk of increasing cancer likelihood over a lifetime. The risk from a single scan is minimal, but it can add up. That's why clinicians are so strict about the ALARA (As Low As Reasonably Achievable) principle—they always use the lowest possible radiation dose to get the job done and only order these scans when the medical benefit is crystal clear.
Contrast agents, which are sometimes injected to make certain tissues pop on the scan, are another consideration. They are generally very safe but can cause allergic reactions in a small number of patients or pose a risk for those with kidney issues.
Then you have modalities like MRI and Ultrasound, which don't use ionizing radiation at all and are considered extremely safe.
- MRI's main safety concerns stem from its powerful magnetic field. It's crucial for patients to report any metal in their body, like pacemakers or aneurysm clips, because the magnet can interfere with them.
- Ultrasound uses simple sound waves and has no known long-term risks. This makes it the go-to for sensitive situations, like monitoring a baby's development during pregnancy.
Rest assured, your doctor always weighs the pros and cons carefully before ever recommending a scan.
Building 3D Models from 2D Slices
So, how does a stack of flat, 2D images magically turn into a dynamic 3D model that a surgeon can spin around on a screen? It's a brilliant bit of digital engineering. The easiest way to picture it is by thinking of a deck of cards.
Each individual image from a CT or MRI is like a single playing card—a thin, two-dimensional slice. Medical imaging software takes this whole stack of hundreds, sometimes thousands, of digital "cards" and arranges them in their exact order.
But the software does more than just stack them up. Its powerful algorithms interpolate the data between each slice, essentially filling in the gaps to create a smooth, continuous volume. Every single pixel in those 2D slices contains crucial information about tissue density and location, which is exactly what the software uses to build the complete 3D structure.
This final model is so much more than a cool visual. It's an interactive digital twin of the patient's anatomy. A surgeon can use it to plan a complex operation, virtually dissecting the model, measuring distances with sub-millimeter accuracy, and mapping out every step before making the first incision. This digital roadmap has become a cornerstone of modern surgery, dramatically improving both safety and precision.
At PYCAD, we specialize in bringing the power of artificial intelligence to this intricate process. Our advanced AI solutions are designed to enhance diagnostic accuracy and streamline the analysis of medical images, helping clinicians turn complex data into life-saving decisions. Discover how we can advance your medical imaging capabilities at https://pycad.co.