At its core, Clinical Decision Support (CDSS) is health technology that gives clinicians the right information, for the right patient, at the right time. It's not about replacing a doctor's judgment. Think of it as an incredibly smart assistant, whispering evidence-based suggestions and critical patient data directly into a physician's workflow. The whole point is to improve patient safety and raise the standard of care.
Understanding Clinical Decision Support

Picture a physician trying to piece together a complex case. They're juggling lab results, known allergies, past procedures, and current prescriptions—a mountain of data. A Clinical Decision Support System acts like a guide, working silently in the background within the electronic health record (EHR). It constantly analyzes this information and offers timely, relevant advice when it matters most.
This isn't about the system making the decisions. Far from it. Instead, it’s a critical safety net. The system's main job is to blend the latest medical knowledge with a patient's specific data, flagging things that a busy clinician might otherwise miss.
A Co-Pilot for Better Outcomes
So, what does this look like in the real world? CDSS isn't a single piece of software but a wide range of tools, each serving a different purpose. They all share the same goal: helping clinicians make better, safer choices.
Here are just a few examples of what these systems can do:
- Flagging Potential Risks: A doctor prescribes a new medication, and the system immediately sends an alert about a potential adverse interaction with another drug the patient is taking.
- Suggesting Best Practices: For a patient with a specific diagnosis, the system can pull up the most current, evidence-based treatment guidelines.
- Providing Dosing Guidance: It can automatically calculate the precise medication dosage based on a patient’s weight, age, and kidney function, reducing the chance of human error.
- Enhancing Diagnostic Accuracy: Based on a patient's symptoms and initial lab results, the system might present a list of differential diagnoses for the clinician to consider.
To put it simply, clinical decision support is the bridge between observation and knowledge. It's what turns a sea of raw data into clear, actionable insights that lead to better health outcomes.
For a quick overview, this table breaks down the essentials of what a CDSS does.
Clinical Decision Support At a Glance
| Core Function | Primary Goal | How It Works | Key Benefit |
|---|---|---|---|
| Presenting timely, relevant clinical knowledge. | Improve patient safety and quality of care. | Integrates with EHRs to analyze patient data in real-time. | Reduces medical errors and adverse events. |
| Offering evidence-based recommendations. | Ensure adherence to best practice guidelines. | Matches patient-specific info against established protocols. | Standardizes care and improves patient outcomes. |
| Providing alerts and reminders. | Prevent oversights and mistakes. | Flags potential issues like drug interactions or allergies. | Enhances clinician awareness at the point of care. |
Ultimately, these systems act as a powerful layer of support, helping clinicians navigate the complexities of modern medicine with more confidence.
The demand for these systems is surging, thanks to the widespread adoption of EHRs and huge leaps in artificial intelligence. This trend underscores a clear commitment across healthcare to use technology for safer, more efficient patient care. You can explore the data behind this growth by reviewing the expanding CDSS market trends and forecasts at Precedence Research.
Breaking Down a CDSS Framework
So, what's really going on under the hood of a clinical decision support system? It's easy to think of it as a single piece of tech, but it’s more like a three-part harmony. Each component has a distinct job, but they all work together to turn raw patient data into a genuinely helpful insight for a doctor or nurse.
1. The Knowledge Base: The System’s Library
Everything starts with the knowledge base. Picture a massive, constantly evolving digital medical library. This is where the system stores all the clinical information it needs to make smart recommendations.
But this isn't just a dusty old bookshelf. The knowledge base is a highly structured collection of rules, clinical guidelines, and evidence-based protocols. For example, it might contain information on thousands of drug-to-drug interactions, best-practice care plans for diabetes, or standard formulas for medication dosing.
2. The Inference Engine: The System’s Brain
Next up is the inference engine. If the knowledge base is the library, the inference engine is the brilliant librarian who connects all the dots. This is the processor that does the actual "thinking."
When a clinician enters new information into a patient’s electronic health record (EHR)—say, a new diagnosis or a prescription—the inference engine immediately gets to work. It takes that new piece of data and runs it against the entire knowledge base, looking for connections. Using a series of "if-then" rules, it figures out if the new information triggers a specific warning, protocol, or suggestion. This is what gives the system its intelligence, letting it analyze a patient's specific situation on the fly.
3. The Communication Mechanism: The Messenger
Finally, you have the communication mechanism. This is how the system actually gets the insight back to the clinician. After all, a brilliant deduction from the inference engine is completely useless if no one sees it.
This part is critical. One study found that clinicians ignore safety alerts between 49% and 96% of the time, largely due to "alert fatigue." A poorly designed interface can render an otherwise powerful CDSS ineffective.
This is why the delivery method has to be just right for the situation. It can show up in a few different ways:
- Active Alerts: Urgent pop-up notifications that demand immediate attention, like a warning about a potentially fatal drug allergy.
- Passive Reminders: A more subtle flag or icon, maybe next to a lab value that's slightly out of the normal range. It provides context without disrupting the clinician's workflow.
- Data Visualizations: Instead of just spitting out numbers, the system might display patient data in a graph to make it easier to see trends over time.
- Order Sets: When a common diagnosis is made, the system can suggest a pre-built list of standard tests, medications, and consults to consider.
This infographic breaks down how this well-oiled framework leads to tangible benefits.
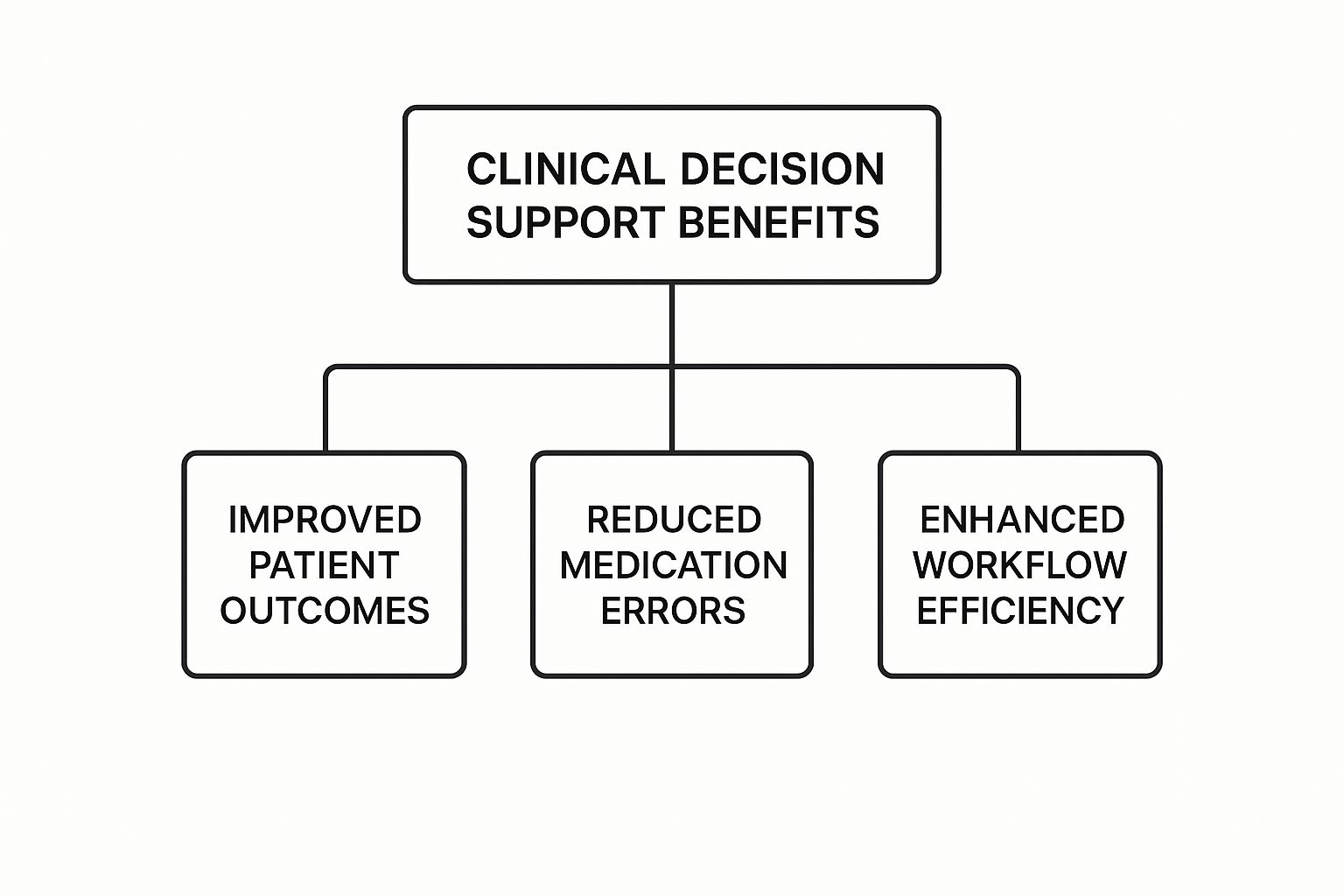
As the diagram shows, these components work together to improve patient outcomes, make medication management safer, and streamline day-to-day clinical work. It’s a powerful feedback loop: data becomes knowledge, knowledge prompts action, and that action leads directly to better patient care.
Seeing Clinical Decision Support in Action
Theory is one thing, but how does a clinical decision support system actually perform when the stakes are high in a real medical setting? Let's walk through a common scenario to see this technology at work.
Picture this: a physician is with a patient who has a complicated medical history—we're talking multiple chronic conditions and a list of ongoing prescriptions.
The doctor decides to prescribe a new medication to address a new symptom. As they type the prescription into the patient's Electronic Health Record (EHR), the CDS system is already working behind the scenes. In an instant, it cross-references the new drug against the patient's entire profile, including every known allergy, current medication, and recent lab result.
From Data to Intervention
In mere seconds, the system’s inference engine flags a potentially dangerous interaction between the new drug and one the patient is already taking. This isn't just a generic warning. The system recognizes that this specific combination could trigger severe side effects for this particular patient.
This is where the communication component kicks in. Instead of letting the order go through, the system generates a clear, non-intrusive alert on the physician's screen.
A well-designed alert is crucial. It has to provide enough context to be helpful without becoming just another annoying popup. This helps clinicians avoid "alert fatigue," a very real problem where people start ignoring excessive notifications.
The alert doesn't just flash a red "Warning" sign. It delivers actionable intelligence, like:
- Specific Interaction: It clearly names the two drugs that could interact negatively.
- Potential Outcome: It briefly explains the risk—for example, an increased chance of kidney damage.
- Alternative Suggestions: It might even suggest safer alternative medications, pulling recommendations from established clinical guidelines.
This immediate feedback loop turns the CDS from a passive data repository into an active safety net. It doesn't make the decision for the doctor. Instead, it gives them the critical information they need to pause, reconsider, and ultimately choose a safer, more effective treatment path for their patient.
The real power of CDS is its ability to weave evidence-based knowledge directly into the day-to-day clinical workflow, improving both patient outcomes and efficiency. These systems play a huge role in cutting down on medical errors, especially adverse drug events, which is a direct win for patient safety and the quality of care. To get a better sense of the broader impact, you can read the full research on how CDSS improves healthcare quality on marketsandmarkets.com.
The Real-World Benefits of Implementing CDSS
It’s easy to get lost in the technical details, but the real magic of clinical decision support happens at the bedside. Its impact isn't just about better data; it's measured in lives improved, errors caught, and efficiencies found. When a CDSS is implemented well, it sends positive ripples through the entire healthcare ecosystem, benefiting patients, clinicians, and the organization itself.
A Safety Net for Patients
For patients, the biggest win is safety. Think of a well-integrated CDSS as a tireless digital guardian, constantly watching for potential problems. This is especially true when it comes to medications, where the risk of error is high.
A huge portion of preventable medical harm comes from adverse drug events. A CDSS can instantly flag a dangerous drug-drug interaction, an incorrect dosage, or a patient's known allergy right at the point of prescribing. It's a simple intervention that makes care profoundly safer.
This safety net goes beyond just prescriptions. By making sure treatment plans follow the latest evidence-based guidelines, these systems help ensure every patient gets the best possible care for their condition. The result is better, more predictable outcomes.
Empowering Clinicians, Not Replacing Them
For doctors and nurses on the front lines, a CDSS provides a much-needed layer of confidence. In a chaotic emergency room or a busy clinic, having immediate access to best practices or diagnostic prompts can make a world of difference. It’s not about taking over their job; it's about giving them powerful, data-driven insights to augment their own expertise.
This support shows up in very practical ways that improve daily workflows:
- Catching Diagnostic Errors: By suggesting a list of possible diagnoses based on a patient's symptoms and lab results, a CDSS can help a doctor consider an uncommon condition they might have otherwise missed.
- Sticking to the Standard of Care: The system gently nudges clinicians to follow established protocols, which is key for maintaining high-quality care and meeting regulatory requirements.
- Making Work Flow Smoother: Instead of building an order set from scratch for a common diagnosis like pneumonia, a clinician can use a pre-built template. This saves precious minutes that can be better spent with the patient.
Building a Stronger Healthcare Organization
From a hospital or clinic administrator's perspective, the benefits are just as clear. By standardizing care and cutting down on expensive medical errors, these systems directly help manage costs while elevating the quality of care.
Better adherence to clinical guidelines also translates to stronger performance on key quality metrics and, in turn, higher patient satisfaction scores. Ultimately, a CDSS helps build a culture of safety and continuous learning—an essential foundation for any modern healthcare organization. It makes the entire system more efficient, reliable, and effective for everyone involved.
Exploring the Different Flavors of CDSS

When we talk about clinical decision support, it’s not a one-size-fits-all concept. The tools out there are incredibly diverse, running the gamut from basic calculators that double-check a medication dose to sophisticated platforms that can suggest a list of possible diagnoses.
Grasping these differences is crucial. It helps us see how each tool is built to solve a specific problem, whether that's a routine safety check or a complex diagnostic mystery.
Broadly speaking, CDSS tools can be sorted into two main buckets based on how they process information: knowledge-based systems and non-knowledge-based systems. Each has its own way of arriving at the guidance clinicians see on their screens.
Knowledge-Based Systems: The Rule-Followers
The classic, and still most common, type of CDSS is knowledge-based. You can think of these systems as a massive, digital library of medical rules. They work on a straightforward "if-then" logic that human experts have carefully coded into them.
A perfect example is a simple drug allergy rule: IF a patient's record shows a penicillin allergy, THEN trigger an alert when a doctor tries to prescribe amoxicillin.
These systems are reliable and easy to understand. You can always trace their recommendations back to a specific, pre-written rule. That makes them fantastic for tasks like flagging drug-drug interactions, sending reminders for routine screenings, or making sure care follows established guidelines.
Non-Knowledge-Based Systems: The Pattern-Detectives
On the other end of the spectrum are the non-knowledge-based systems, which are often driven by artificial intelligence and machine learning. Instead of following a pre-written rulebook, these systems learn by digging through enormous piles of clinical data to find hidden patterns.
They analyze millions of anonymized patient records, lab values, and doctor's notes, looking for subtle connections that would be nearly impossible for a human to spot. A non-knowledge-based system, for example, might discover that a specific combination of symptoms and lab results points to a high risk for a rare disease.
This data-first approach means the system can adapt and get smarter over time. The more data it sees, the better it gets at making accurate predictions and offering subtle recommendations that go far beyond simple alerts.
The real distinction is in how they come up with their advice. One follows explicit commands, while the other uncovers insights from the data itself. To make this clearer, let's break down the core differences.
Comparing Types of Clinical Decision Support Systems
The table below offers a side-by-side look at how these two approaches stack up in the real world.
| CDSS Type | How It Works | Common Use Case | Level of Interaction |
|---|---|---|---|
| Knowledge-Based | Uses pre-programmed "if-then" rules defined by experts. | Allergy alerts, drug interaction warnings, guideline reminders. | Often passive, providing clear alerts based on set criteria. |
| Non-Knowledge-Based | Uses AI to find patterns and correlations in large datasets. | Predicting disease risk, suggesting differential diagnoses, analyzing medical images. | Can be more interactive, offering probabilistic insights and complex data analysis. |
At the end of the day, the healthcare world needs both. Knowledge-based tools act as a dependable safety net for everyday clinical practice. Meanwhile, non-knowledge-based systems are out on the frontier, showing us what's next for diagnostics and truly personalized medicine.
How AI Is Shaping the Future of CDSS
The next chapter for clinical decision support is already being written, and it’s fueled by Artificial Intelligence (AI) and Machine Learning (ML). We're seeing these systems move beyond the simple, rule-based alerts of the past and into a world of predictive insights. This is a fundamental shift from reactive warnings to proactive, intelligent guidance.
Think about a system that’s constantly monitoring the tiny, almost imperceptible changes in a patient's vitals. Instead of just flagging a high heart rate, it spots a complex pattern that predicts the onset of sepsis hours before it becomes a full-blown crisis. That's the real power of AI in CDSS—it finds the faint signals hidden in mountains of data that are often invisible to the human eye.
Augmented Intelligence in Medical Imaging
Nowhere is this shift more obvious than in medical imaging. AI algorithms are being trained on massive libraries of scans—X-rays, CTs, and MRIs—learning to pick up the earliest signs of diseases like cancer or diabetic retinopathy.
The goal isn't to replace radiologists. It's to give them a form of augmented intelligence. An AI can meticulously screen thousands of images, flagging suspicious areas that need a closer look from a human expert. This kind of collaboration boosts both speed and diagnostic accuracy.
This approach creates a powerful partnership between the clinician and the machine. The AI does the heavy lifting of pattern recognition, which frees up physicians to concentrate on the complex work of diagnosis, treatment planning, and actually talking to their patients.
These tools are giving clinicians the ability to see more, understand more, and act faster than ever before. The influence of AI isn't just limited to direct clinical guidance, either. It's also boosting productivity in other areas, with tools like AI-powered writing assistants showing how this technology can help with healthcare documentation and communication. This is what the future of clinical decision support looks like: a truly intelligent partner helping deliver exceptional care.
Got Questions About CDSS? We've Got Answers.
Jumping into the world of clinical decision support can feel complex, and it's natural to have a few questions. Let's break down some of the most common ones with straightforward, practical answers.
How Does a CDSS Actually Talk to an EHR?
Think of it like two people who speak different languages needing a translator. A CDSS connects with an Electronic Health Record (EHR) system using interoperability standards like HL7 and FHIR. These standards act as the universal translator, allowing the two separate systems to share information smoothly and securely.
This connection is everything. It lets the CDSS pull patient data from the EHR in real time, analyze it, and then push relevant alerts or guidance right back into the clinician's existing workflow. No toggling between screens, just smart support exactly when it's needed.
Is the Goal for CDSS to Replace Doctors?
Not a chance. A CDSS is a co-pilot, not the pilot. It’s a powerful tool designed to augment a clinician’s expertise by providing data-backed insights, flagging potential safety issues, and highlighting best practices.
The final medical decision always rests with the healthcare professional. They bring something a system can't: the full context of a patient's life, their personal wishes, and the nuanced details of their situation. A CDSS offers valuable information, but the doctor's judgment and experience make the final call.
What Are the Biggest Hurdles to Getting a CDSS Running?
Implementing a CDSS isn't just a plug-and-play situation. There are a few common bumps in the road that every organization needs to navigate. The most notorious one is "alert fatigue." If clinicians are bombarded with too many low-priority notifications, they'll inevitably start tuning them all out—even the critical ones.
Beyond that, other key challenges include:
- Keeping the Knowledge Base Fresh: Medical science doesn't stand still. The system's rules and guidelines need constant updates to reflect the latest evidence.
- The Upfront Cost: There’s no getting around it—the initial investment in software, integration work, and training can be significant.
- Getting Staff Onboard: Proper training is crucial. Clinicians need to understand how the tool works and, more importantly, trust the guidance it provides.
At PYCAD, we focus on building smarter AI that cuts through these challenges, especially in medical imaging. We help enhance diagnostic accuracy without adding to the noise. See how our custom solutions can upgrade your medical devices by visiting us at https://pycad.co.






