When a patient has to come back to the hospital shortly after being discharged, it’s more than just an inconvenient statistic. It signals a breakdown somewhere in the care journey, a failure to set that person up for a successful recovery at home.
The goal isn't just to get readmission numbers down; it's to fix the gaps in care that cause patients to return in the first place. This means rethinking the entire process, from the moment a patient is admitted to long after they’ve gone home. It’s about building a system that’s proactive, not reactive, and truly supports patients through one of their most vulnerable times.
Why Reducing Hospital Readmission Rates Matters
A hospital readmission is a massive setback. For the patient, it's often a physically and emotionally draining experience that can kickstart a frustrating cycle of declining health. For the hospital system, high readmission rates are a financial black eye and a huge drain on already scarce resources like staff and beds.
This single metric tells a powerful story about the quality of care you provide. It reflects everything—the accuracy of the diagnosis, how well you educated the patient, and the strength of your follow-up process. Think of it as the ultimate test: did you just treat the immediate problem, or did you prepare the patient to thrive on their own?
The Human and Financial Cost of Readmissions
The stakes couldn't be higher. A patient who boomerangs back to the hospital is at a much greater risk for serious complications, or worse. The ripple effect hits everything from patient outcomes to your bottom line.
This isn't just an operational headache; it's a critical patient safety issue. A study looking at over 185,000 hospital admissions found some truly sobering numbers: patients who were readmitted had an in-hospital mortality rate of 20.6%. For those who weren't readmitted, that number was just 2.1%. You can discover more about the critical link between readmissions and patient outcomes in the full study.
Key Takeaway: A readmission isn't just a failed discharge. For many patients, it represents a life-threatening turn in their health journey, underscoring the urgent need for a better system.
Laying the Foundation for Success
You can't solve this problem with a piecemeal approach. Tackling readmissions requires a structured, comprehensive strategy built on a few core pillars that work in tandem to create a truly continuous care experience.
Below is a quick overview of these foundational components. Think of this as the blueprint for building a program that genuinely supports patients from admission through recovery.
Core Pillars of an Effective Readmission Reduction Strategy
This table summarizes the foundational components of a successful program to lower readmission rates, providing a quick-reference guide to the key areas of focus discussed in this article.
| Strategy Pillar | Objective | Key Activities |
|---|---|---|
| Proactive Planning | To prepare patients for a safe and successful transition home from the day they are admitted. | Initiate discharge planning upon admission, identify potential barriers (social, financial, logistical), and coordinate with post-acute care providers early. |
| Patient & Family Education | To empower patients and their caregivers with the knowledge and confidence to manage their condition at home. | Use teach-back methods, provide clear written instructions (in their preferred language), and confirm medication understanding before discharge. |
| Coordinated Transitional Care | To ensure a seamless handover of care from the hospital to primary care and other community-based services. | Schedule follow-up appointments before the patient leaves, conduct post-discharge follow-up calls within 48-72 hours, and reconcile medications. |
| Technology Integration | To identify at-risk patients early and provide continuous support after they leave the hospital. | Implement remote patient monitoring for high-risk conditions, use predictive analytics to flag patients likely to be readmitted, and offer telehealth options. |
By building your strategy around these core elements, you create a supportive framework that not only prevents readmissions but also drives real, lasting improvements in the quality of care. It’s about empowering patients, connecting the dots between providers, and making sure no one falls through the cracks.
Pinpointing the Real Reasons for Readmission
If you really want to reduce hospital readmissions, you have to stop guessing. It’s all too easy to point the finger at clinical complications, but the truth is, the reasons patients bounce back are often hiding in plain sight. They’re usually tangled up in things like communication breakdowns, social barriers, or clunky system processes.
Looking at your top-line readmission number won't tell you much. Real change starts when you commit to an honest investigation into why specific patients are returning. It means putting on your detective hat and digging into the data, ready to uncover patterns that might even challenge what you think you know.
Assembling Your Investigation Team
A solid root-cause analysis is never a one-person job. The best insights come from bringing together a multidisciplinary team because everyone sees the patient's journey through a different lens. A physician is focused on clinical stability, but a case manager is thinking about whether the patient has a ride to their follow-up appointment.
To get the full picture, you need a diverse crew. Make sure your team includes:
- Clinical Staff: The nurses, physicians, and specialists who live and breathe the medical complexities.
- Case Managers & Social Workers: These are your experts on the ground, spotting social determinants of health (SDOH) like unstable housing or a lack of caregiver support.
- Pharmacists: They can instantly identify medication-related traps, from overly complex regimens to affordability issues.
- Data Analysts: The people who can slice and dice the numbers to find statistical trends you’d otherwise miss.
- Quality Improvement Leaders: They can steer the analysis and help turn your team's findings into an actual plan.
This kind of collaboration breaks down the silos that so often get in the way. The goal is to build a complete, 360-degree view of every factor that could be pushing patients back through your doors.
Digging Deeper with Data Segmentation
With your team in place, the real work begins. The trick is to stop looking at broad, hospital-wide statistics—they’re just too vague to act on. You need to slice your readmission data into smaller, meaningful segments.
For instance, your cardiology unit might find that readmissions for congestive heart failure (CHF) spike among patients over 75 who live alone. That’s not a clinical failure; it's a social support problem. Or maybe a surgical unit discovers readmissions are highest for patients discharged on a Friday, which points to a gap in weekend support.
Crucial Insight: Don't just analyze what is happening; investigate who it is happening to. Segmenting data by condition, demographics, discharge day, and SDOH reveals the hidden stories behind the numbers.
This is where you find your true leverage points for change.
Using Practical Tools for Analysis
To give your investigation some structure, a few practical tools can make a world of difference. The fishbone diagram (also called an Ishikawa diagram) is a fantastic way to visualize complex problems and guide your team’s discussion.
The tool helps your team brainstorm potential causes by sorting them into clear categories. You start with a central "bone" representing the problem—let's say, "High CHF Readmission Rate." Then, you add smaller bones branching off for different categories:
- People: Was the patient education rushed? Did the caregiver actually understand the instructions?
- Process: Are follow-up appointments scheduled before the patient walks out the door? Is the discharge process chaotic?
- Technology: Did the EHR flag the patient's low health literacy score?
- Environment: Does the patient have transportation? Is their home actually safe for recovery?
This method keeps you from jumping to the first, most obvious conclusion and pushes for a more thorough look at all the moving parts. It shifts the conversation from blaming people to fixing systems.
Despite years of national effort, the average 30-day readmission rate in the U.S. has remained stubbornly around 14%. The constant pressure for shorter hospital stays, partly driven by a relatively low number of hospital beds, can sometimes lead to patients being discharged too soon, bumping up that risk. You can explore the full research on readmission trends to see how these dynamics play out.
By pinpointing the precise failure points, you can finally design interventions that address the actual root causes and start moving the needle on this persistent challenge.
Building a Proactive Discharge Planning Process
A successful discharge isn’t just a single event; it's a process. It has to start the moment a patient is admitted. Simply handing someone a stack of papers on their way out the door is a classic recipe for readmission. What works is a proactive approach—one that anticipates needs, tackles potential roadblocks, and truly empowers patients for a safe transition back home.
This shift in thinking is fundamental to lowering readmission rates. It moves your team from putting out fires to preventing them in the first place, creating a safety net that extends far beyond your hospital's walls. The aim here is to build a clear, actionable plan that patients and their families can actually follow.
Start Planning from Day One
The best discharge plans are never rushed together in the last few hours of a hospital stay. They’re built thoughtfully, right from the very beginning. This means weaving key assessments into the admission process itself to get a full, 360-degree view of the patient’s life outside the hospital.
From day one, your team needs to be digging into the practical realities:
- Health Literacy: Can the patient actually understand complex medical information? Do they need materials in another language, or maybe just larger print?
- Social Support: Who’s at home? Is there a reliable caregiver in the picture, or are they going home to an empty house?
- Home Environment: Is their home even safe for recovery? Are there stairs they can't climb or rugs that are major tripping hazards?
- Access to Care: How will they get to follow-up appointments? Can they actually afford the new prescriptions?
Getting answers to these questions early gives you the runway to solve problems before they become crises. For example, flagging a transportation issue on day one gives a social worker a few days to arrange for medical transport. That's a world away from finding out a week later when a critical follow-up appointment has already been missed.
The Power of Patient-Centered Education
If there's a weak link in the discharge chain, it's often patient education. We know that patients who genuinely understand their after-care instructions are over 30% less likely to be readmitted. Yet, so many leave feeling completely overwhelmed, clutching papers they can’t make sense of.
A fantastic way to fix this is the teach-back method. It’s so simple, but incredibly effective for confirming comprehension. Instead of just asking, "Do you have any questions?" (which almost always gets a "no"), you ask the patient to explain the plan back to you in their own words.
Here’s how that sounds in a real room:
A nurse might say, "We’ve gone over your new heart medication. To make sure I did a good job explaining it, can you tell me how many pills you need to take each morning and what you should do if you happen to forget a dose?"
That one exchange instantly highlights any confusion, letting you clarify on the spot. It turns a one-way lecture into a real conversation and helps critical information actually stick.
This infographic lays out the core flow of a proactive discharge process, showing how it all connects.
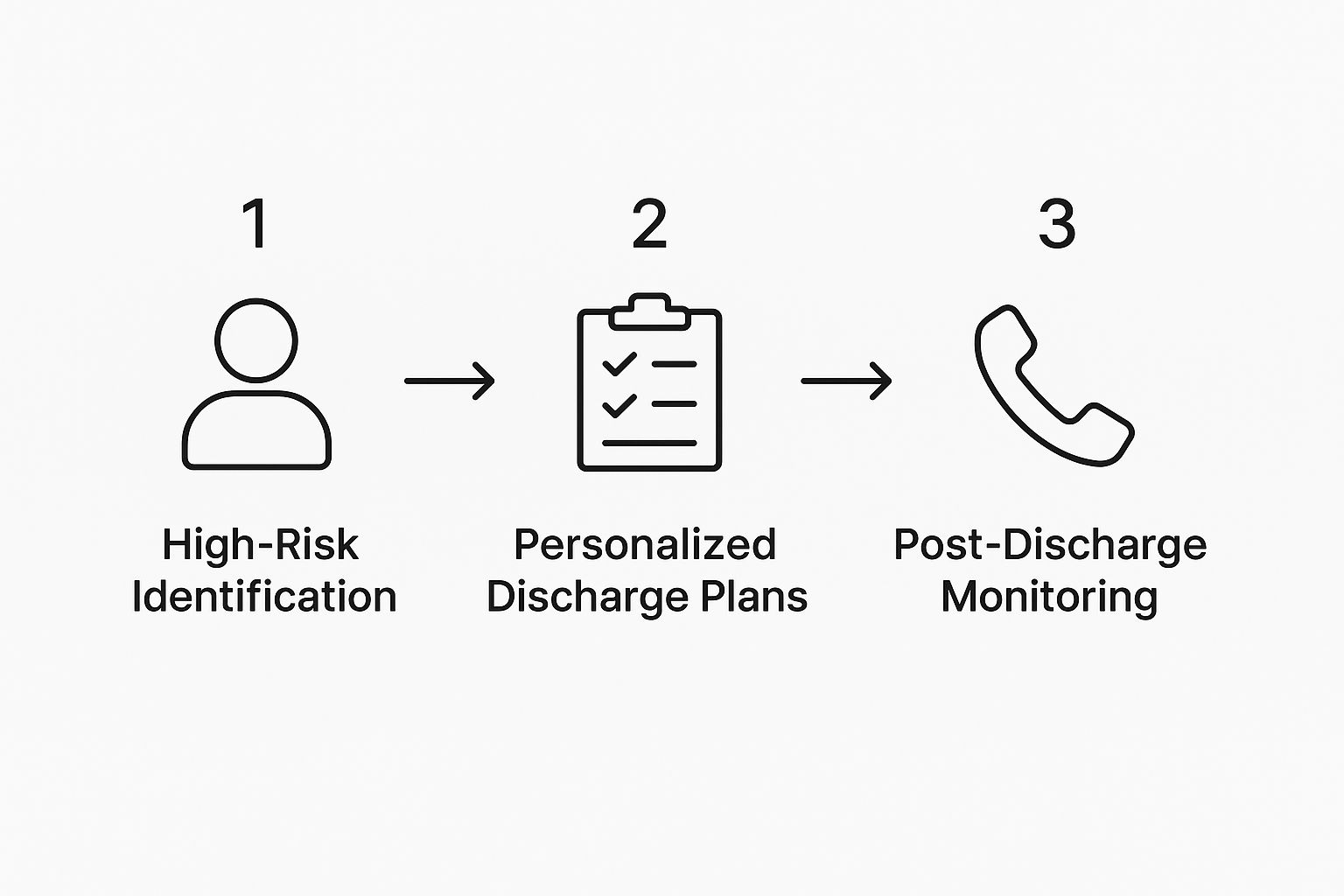
As you can see, a successful transition hinges on a continuous loop of assessing, planning, and following up—it's not a one-and-done event.
Creating Actionable Discharge Packets
Let's be honest: those generic, multi-page discharge summaries often go straight into the trash. An effective discharge packet needs to be customized, crystal-clear, and easy to navigate. Think of it less as a dense medical document and more like a user-friendly guide to getting better.
Here’s what a great one includes:
- A Clear Medication List: This should spell out each medication, its purpose, the dosage, and specific times to take it. Use a large font and plain language.
- Upcoming Appointments: List every scheduled follow-up, complete with the doctor's name, address, and phone number. A map is a great touch.
- Key Contacts: Create a simple list of who to call for what—the primary doctor for general questions, the specialist for specific concerns, and the hospital's nurse line for anything urgent.
- Warning Signs: I love a simple "red, yellow, green" format here. Explain which symptoms are normal (green), which mean they need to call a doctor (yellow), and which demand an immediate trip back to the ER (red).
This kind of structure cuts through the noise and gives patients a clear roadmap. For patients with more complex needs or very little support at home, bringing in specialized hospital discharge services can also be a game-changer, bridging the gap between hospital and home.
The Role of the Care Coordinator
A dedicated care coordinator or transition coach is the glue that holds this whole process together. This person acts as the central point of contact, making sure nothing falls through the cracks. They are the communication hub, connecting the hospital team, the patient and their family, and all the outpatient providers.
Think of them as the quarterback for the entire transition. They’re the ones confirming prescriptions were filled, making sure the patient has a ride to their first follow-up, and just being a reassuring voice on the phone. That human touch provides an incredible sense of security and ensures the plan you worked so hard to create is actually put into motion.
Bolstering Post-Discharge and Transitional Care
A patient’s journey to recovery doesn't stop at the hospital exit. In many ways, it's just beginning. Those first 30 days after discharge are a fragile, high-stakes window where a solid care plan can either hold firm or completely fall apart. This is why strengthening transitional care is so non-negotiable—it's the critical bridge between the controlled hospital environment and the unpredictable reality of being back home.
Think of this phase as building a safety net to catch patients before they stumble. It’s all about turning a potentially chaotic transition into a well-managed, supported continuation of care. A crucial part of this is providing patients and their families with the right resources. A well-structured guide to safe recovery at home for preventing hospital readmissions can be an invaluable tool for everyone involved.
The Make-or-Break First 72 Hours
The first few days at home are packed with risk. This is precisely when confusion over new medications creeps in, unexpected symptoms pop up, and questions that seemed clear in the hospital suddenly become urgent. One of the most powerful, low-cost interventions you can implement is a simple, structured follow-up call within 48 to 72 hours.
This isn't just a courtesy check-in; it's a clinical checkpoint. The goal is to get straight to the point:
- Medication Check: "Did you get your new prescriptions filled? Let's quickly go over which pills you take in the morning versus at night."
- Symptom Review: "We talked about a few warning signs to watch for. Have you experienced any of them since you've been home?"
- Appointment Logistics: "I see your follow-up with Dr. Smith is next Tuesday. Do you have a ride lined up?"
These direct questions uncover red flags early. You can then jump in immediately—clarifying a dosage with the pharmacy or urging a call to their PCP—before a small problem snowballs into a full-blown crisis that lands them right back in the hospital.
High-Impact Home Visits for High-Risk Patients
While phone calls are a great start, some patients need a more hands-on approach. For those you've identified as high-risk—maybe they're juggling multiple chronic conditions, a complex medication schedule, or have little social support—a targeted home visit can be a game-changer. These visits offer a level of insight you simply can't get over the phone or in a clinic.
When a visiting nurse or community health worker steps into a patient's home, they get a real-world assessment. They can see with their own eyes if the patient can navigate their space safely, check if the fridge is stocked with appropriate food, and even watch them sort their pillbox.
A home visit gives you an unfiltered look into the patient's daily reality. It's where you discover the "easy-open" prescription bottle is impossible for arthritic hands, or that the patient's idea of a low-sodium diet is still eating canned soup every day.
This direct observation allows for on-the-spot problem-solving and personalized education that actually sticks because it's tied to their lived experience. It moves care from abstract instructions to practical, real-world support.
Comparing Post-Discharge Support Models
Choosing the right post-discharge strategy depends on your patient population, available resources, and specific goals. Not every patient needs the same level of intervention. Here's a look at how different support models stack up, helping you decide where to invest your efforts.
| Model | Description | Best For | Resource Intensity |
|---|---|---|---|
| Phone-Based Follow-up | Structured calls made within 72 hours of discharge to check on medications, symptoms, and appointments. | Low-to-moderate risk patients; broad population coverage. | Low |
| In-Person Home Visits | Targeted visits by nurses or community health workers to assess the home environment and provide hands-on support. | High-risk patients with complex needs, mobility issues, or low health literacy. | High |
| Telehealth & RPM | Virtual check-ins and remote monitoring of vitals (e.g., blood pressure, weight) using connected devices. | Patients with chronic conditions like CHF or COPD; those in rural areas. | Moderate |
| Transitional Care Clinics | Dedicated outpatient clinics for post-discharge follow-up within 7-14 days, staffed by a multidisciplinary team. | Patients needing comprehensive clinical review post-hospitalization. | Moderate-High |
Ultimately, many organizations find success with a hybrid approach, using low-cost calls for everyone and reserving more intensive models like home visits or remote monitoring for those who need them most.
Telehealth as a Post-Discharge Lifeline
For many people, especially those in rural areas or with limited mobility, telehealth isn't just a convenience—it's a lifeline. It effectively closes the gap between the care team and the patient, ensuring continuous support without the burden of travel.
During the transitional period, telehealth can be used in a few powerful ways:
- Virtual Check-ins: A quick video call lets a nurse visually assess a patient's condition, check on wound healing, or simply offer reassurance face-to-face.
- Remote Patient Monitoring (RPM): For conditions like congestive heart failure or COPD, tools that track daily weight, blood pressure, and oxygen levels are invaluable. They provide real-time data that allows your clinical team to step in at the first sign of trouble.
This kind of proactive monitoring helps you catch physiological changes long before a patient even feels symptoms, turning what would have become a reactive ER visit into a simple, proactive medication adjustment.
Federal initiatives also recognize how crucial these efforts are. The Hospital Readmissions Reduction Program (HRRP) from CMS financially penalizes hospitals for excessive readmissions. For fiscal year 2025, only 7% of hospitals received penalties of 1% or more, the third straight year that number has dropped. It's clear that focused strategies are paying off. You can discover more about these penalty trends and hospital performance to see how healthcare systems are successfully adapting.
Using Technology and AI for Predictive Prevention

The old model of simply reacting to readmissions is quickly becoming obsolete. We now have the tools to get ahead of the problem, using data to see potential issues long before they become emergencies. By weaving smart technology into our daily workflows, we can build a system that flags high-risk patients from the start and keeps a close watch on them after they've gone home.
This isn’t about adding more tasks to a nurse’s already packed schedule. It's about working smarter. The right tech automates the grunt work—the endless data collection and analysis—so your clinical staff can dedicate their time to what they do best: patient care. The aim is to fundamentally change how we manage patient transitions, making them safer, more efficient, and far better at keeping people out of the hospital.
Harnessing Real-Time Data with Remote Patient Monitoring
One of the biggest black holes in post-discharge care has always been a lack of visibility. The moment a patient walks out the door, we lose access to the daily data points that tell us how they're really doing. Remote Patient Monitoring (RPM) completely changes that. It gives us a direct line of sight into a patient’s recovery right in their own home.
RPM tools are simple, connected devices patients use every day to track vital signs. Common examples I've seen work wonders include:
- Smart Scales: Essential for congestive heart failure (CHF) patients. A sudden weight gain can be the first sign of fluid retention, and catching it early is critical.
- Blood Pressure Cuffs: Perfect for monitoring hypertension and making sure medications are dialed in correctly.
- Pulse Oximeters: A lifeline for patients with COPD, allowing us to track their oxygen saturation levels from afar.
This data flows directly to a central dashboard where your care team can see it in real-time. It creates a continuous stream of objective health information. A nurse can spot a subtle, concerning trend—like a slow but steady weight increase over three days—and immediately intervene with a phone call or a telehealth visit. That simple, proactive check-in can stop a minor issue from spiraling into a full-blown emergency.
Unlocking Predictive Insights with AI and Machine Learning
While RPM gives us a real-time view, Artificial Intelligence (AI) and machine learning help us look into the future. They do this by finding hidden patterns in the data we already have. Your Electronic Health Record (EHR) is a goldmine of information just waiting to be analyzed to predict who is most likely to be readmitted—often before they've even left their hospital bed.
Machine learning models can sift through thousands of data points at once, looking at things like:
- A patient's medical history and existing comorbidities
- Lab results and vital signs from their current stay
- The total length of their hospitalization
- Demographic details and even social determinants of health
These algorithms spot complex correlations a person might easily miss, generating a "readmission risk score" for every single patient at discharge. This allows your team to channel high-touch resources—like home visits or specialized transition coaches—to the people who truly need them the most.
Real-World Application: I've seen systems that flag a patient with diabetes who also has a history of missed appointments and lives in a "pharmacy desert." The AI triggers an automatic alert for a pharmacist to conduct a one-on-one medication counseling session before discharge, making sure the patient not only has their prescriptions but also a concrete plan to manage them.
This predictive power is the cornerstone of any modern strategy to reduce hospital readmission rates. It moves us away from a one-size-fits-all approach and toward care that is deeply personalized and risk-adjusted.
Integrating Technology into Clinical Workflows
Let’s be honest: the most powerful technology is worthless if it's a pain for your staff to use. Success hinges on seamless integration. The insights from AI and RPM tools can't live on some separate platform that clinicians have to remember to log into. That’s a recipe for failure.
Instead, the information needs to be pushed directly into the EHR where your teams already live and breathe. A high-risk alert from an AI model should pop up as an unmissable banner on the patient's chart. An abnormal RPM reading should automatically generate a task in a nurse's daily work queue.
When you set it up this way, technology becomes a helpful assistant, not another administrative headache. When insights land in the right place at the right time, your staff can act on them quickly and confidently, turning powerful data into life-saving interventions.
Common Questions About Reducing Hospital Readmissions
When you're trying to build a solid program to lower hospital readmissions, a lot of practical questions come up. It's easy to get bogged down in the details, so let's clear the air and tackle some of the most common questions I hear from healthcare leaders. Getting these answers straight can give your team the confidence to move forward.
What Is the Single Most Effective Strategy?
Everyone's looking for that one magic bullet, but the truth is, it doesn't exist. The closest thing we have is a multi-faceted strategy that revolves around comprehensive, individualized discharge planning—and it has to start the moment a patient is admitted. This isn't just about handing over a packet of papers at the door; it's an active process of spotting and removing roadblocks to a safe recovery at home.
So, what does that actually look like?
- Real Patient Education: You have to move beyond just talking at patients. Using proven methods like "teach-back" ensures they and their families actually understand the condition, what each medication is for, and the early warning signs that mean "call the doctor."
- Proactive Appointment Scheduling: Don't leave it to the patient. A major hurdle is simply getting that first follow-up appointment scheduled. Make sure it's booked before they walk out the door.
- A Timely Follow-Up Call: This is non-negotiable. A structured call from a nurse or care manager within 48-72 hours of discharge is your first line of defense. It’s a chance to catch medication confusion or early symptoms before they spiral into a full-blown emergency.
Think of these elements as building a bridge from the highly controlled hospital setting to the often-chaotic reality of a patient's home life. It’s this bridge that prevents people from falling through the cracks.
How Can Smaller Hospitals Implement These Changes?
If you're at a smaller hospital, the idea of a massive overhaul can feel overwhelming. The key is not to do everything at once. Be surgical. Focus on high-impact, low-cost initiatives first.
Start by picking one specific, high-readmission group—say, patients with heart failure—and do a deep dive into why they're coming back. This tight focus channels your limited resources where they'll make the biggest difference.
Smart Starting Points for Smaller Facilities:
Focus on standardizing your discharge checklists. It costs nothing but ensures every patient gets the same high-quality send-off. You can also rework your patient education handouts to use simpler language and more visuals. Another game-changer? Tasking existing nurses or social workers with making those crucial post-discharge calls. You don't always need a new hire to make a huge impact.
Look outside your own walls, too. Partnering with local home health agencies or community groups can extend your reach without adding to your payroll. The goal is to start small, prove what works with your own data, and then build from there.
How Long Until We See a Reduction in Readmissions?
This is the big question, and the answer depends on where you're starting from and how aggressive your plan is. But with a focused, consistent effort, most hospitals begin to see a positive downward trend within six to nine months.
Those initial gains usually come from the "quick wins," like getting a solid post-discharge call process in place. The deeper, more sustainable reductions—the kind that really change your numbers—often take 12 to 18 months. That’s the time it takes for new workflows to become second nature for your staff and for the insights from your data to inform bigger, system-wide improvements. Patience and persistence are key.
What Role Do Social Determinants of Health Play?
Social determinants of health (SDOH) aren't just a side issue; they are often the main reason patients get readmitted. Think about it: a patient could have the best clinical care in the world, but it all falls apart if they can't get a ride to their follow-up appointment, can't afford their medications, or don't have stable housing.
A truly effective readmission reduction program has to screen for these real-world challenges. It means asking the tough questions and being ready to connect patients with help.
This might look like:
- Building a relationship with the local food bank.
- Having a list of medical transportation services on hand.
- Bringing in a social worker to help a patient navigate housing or financial aid applications.
Ignoring SDOH is like sending a patient home with a perfect recipe but an empty pantry. To help people stay healthy and out of the hospital, you have to address the life that happens outside your doors.
At PYCAD, we specialize in developing AI solutions that enhance medical imaging diagnostics and operational efficiency. Discover how our expertise in AI and computer vision can help your organization unlock predictive insights and build a more proactive approach to patient care. Learn more about our AI services for medical imaging at PYCAD.