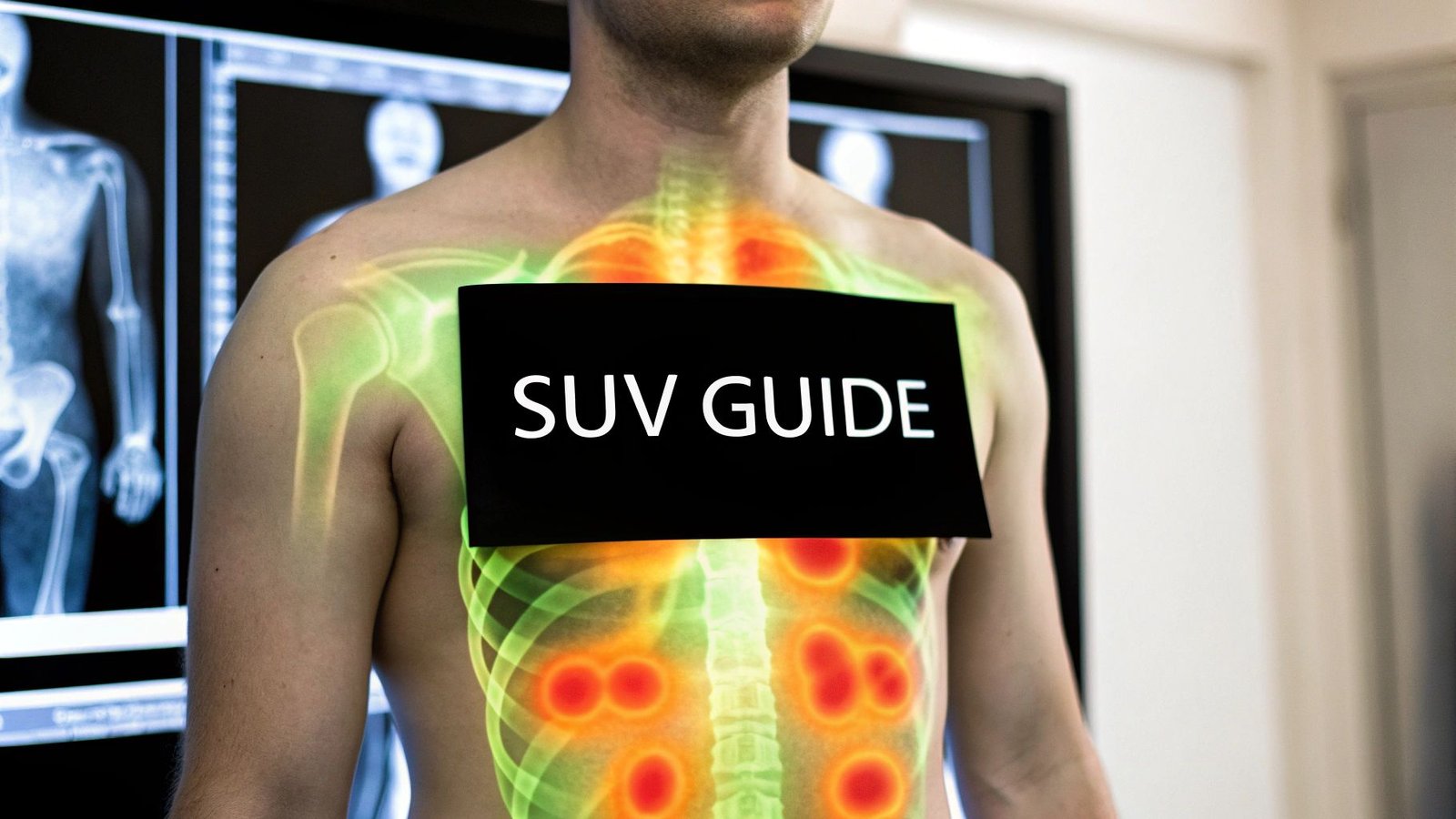
Standard Uptake Values (SUVs) are a cornerstone of modern PET scans, essentially acting as a biological heat map for cellular activity. This single number helps doctors pinpoint areas in the body where cells are burning through energy at an unusually high rate—a potential red flag for conditions like cancer. Getting a handle on what this value means is the first real step to understanding a PET scan report.
Decoding the Numbers on Your PET Scan Report

Think of your body as a bustling city and sugar as the electricity powering it. Most neighborhoods have a predictable, steady energy draw. But what if one block is suddenly pulling a massive amount of power? A Positron Emission Tomography (PET) scan is like the city's power grid monitor—it's designed to find those energy-guzzling hotspots.
To make this happen, a patient is given an injection of a radioactive tracer, usually a type of sugar called fluorodeoxyglucose (18F-FDG). The logic here is simple: cells that are growing and dividing rapidly, like cancer cells, are incredibly hungry. They devour this sugar tracer far more aggressively than healthy, normal tissue.
Measuring Cellular Activity
The PET scanner doesn't see the cells themselves; it detects the tiny radioactive signals coming from where the tracer has accumulated. It then builds a 3D map showing where all that sugar went. The Standard Uptake Value (SUV) is what gives this map a legend—it's the specific number that quantifies just how much tracer has piled up in any given spot.
A higher SUV is a clear signal of higher metabolic activity. It means more of the sugar tracer was gobbled up by the cells in that area. This beautifully simple concept is what makes PET imaging such a powerful tool in medicine today.
Technically, the SUV is a ratio. It compares the concentration of the tracer in a specific tissue to the total dose injected, all normalized for the patient's body weight. This standardization is key, as it allows doctors to compare results more reliably. For context, the blood pool in a healthy person typically has an SUV between 1.5 and 1.9, and the liver usually sits around 2.3 to 2.8. These benchmarks are crucial reference points for interpreting scans, a practice detailed in resources on clinical PET scan interpretation worldwide.
For a quick reference, here’s a breakdown of what the SUV represents in PET imaging.
Key Aspects of Standard Uptake Values at a Glance
| Concept | Simple Explanation | Primary Use in Medicine |
|---|---|---|
| PET Scan Tracer | A radioactive sugar (like 18F-FDG) injected into the body. | Makes metabolically active cells "light up" on a scan. |
| Metabolic Activity | The rate at which cells use energy (sugar) to live and grow. | Cancer cells have very high metabolic activity. |
| Standard Uptake Value (SUV) | A number that measures the concentration of the tracer in a specific area. | To quantify how "hot" or active a spot is. |
| High vs. Low SUV | A high SUV means high energy use; a low SUV means normal or low energy use. | Helps differentiate cancerous tissue from healthy tissue. |
This table provides a snapshot, but the real-world impact of the SUV is where its importance truly shines.
Why Standard Uptake Values Matter
This single number is incredibly influential throughout a patient's cancer care journey. It gives clinicians the data they need to:
- Diagnose Disease: A suspicious lesion with a significantly high SUV is more likely to be malignant (cancerous) than a spot with a low SUV, helping guide decisions like whether a biopsy is needed.
- Monitor Treatment: Oncologists use SUVs to see if a treatment is working. A dramatic drop in a tumor's SUV after a round of chemotherapy is a fantastic sign that the cancer cells are dying off.
- Detect Recurrence: After a patient is in remission, a follow-up PET scan might reveal a new area with a high SUV. This can be the earliest sign that cancer has returned, often long before other imaging methods would catch it.
In essence, the SUV translates a complex biological process into a straightforward, actionable number. It helps transform a colorful PET image into a quantitative tool that guides critical medical decisions.
How Doctors Figure Out a Standard Uptake Value
Calculating a Standard Uptake Value isn't as intimidating as it sounds. The whole process is actually quite logical, and it all starts with a special radioactive sugar called a radiotracer. The one you'll hear about most often is 18F-FDG (fluorodeoxyglucose), which is the key to seeing what’s happening inside the body on a metabolic level.
After it’s injected, the 18F-FDG hitches a ride through the bloodstream. Here’s the clever part: cancer cells are notorious energy hogs. They gobble up this sugary tracer much faster and in greater amounts than healthy, normal tissue. This difference in appetite is what makes tumors and other metabolically active spots "light up" on a PET scan. The scanner picks up the faint radioactive signals from the tracer, building a map of where all that sugar went.
The SUV Formula in a Nutshell
At its core, the math behind a Standard Uptake Value is just a ratio. It’s designed to create a standardized number that allows for fair comparisons between different people, regardless of their size.
The formula essentially looks at how much radiotracer is concentrated in a specific spot and compares that to the total dose injected, all while adjusting for the patient's body weight.
SUV = (Tracer Activity in Tissue) / (Injected Dose / Body Weight)
Why the adjustment for body weight? It’s critical for consistency. A larger person will naturally have the tracer more diluted throughout their body than a smaller person, even if they both receive the exact same dose. By factoring in weight, we get a reliable, relative number that can be compared from one scan to the next.
This image breaks down how the raw data from the scanner gets turned into that single, powerful number.
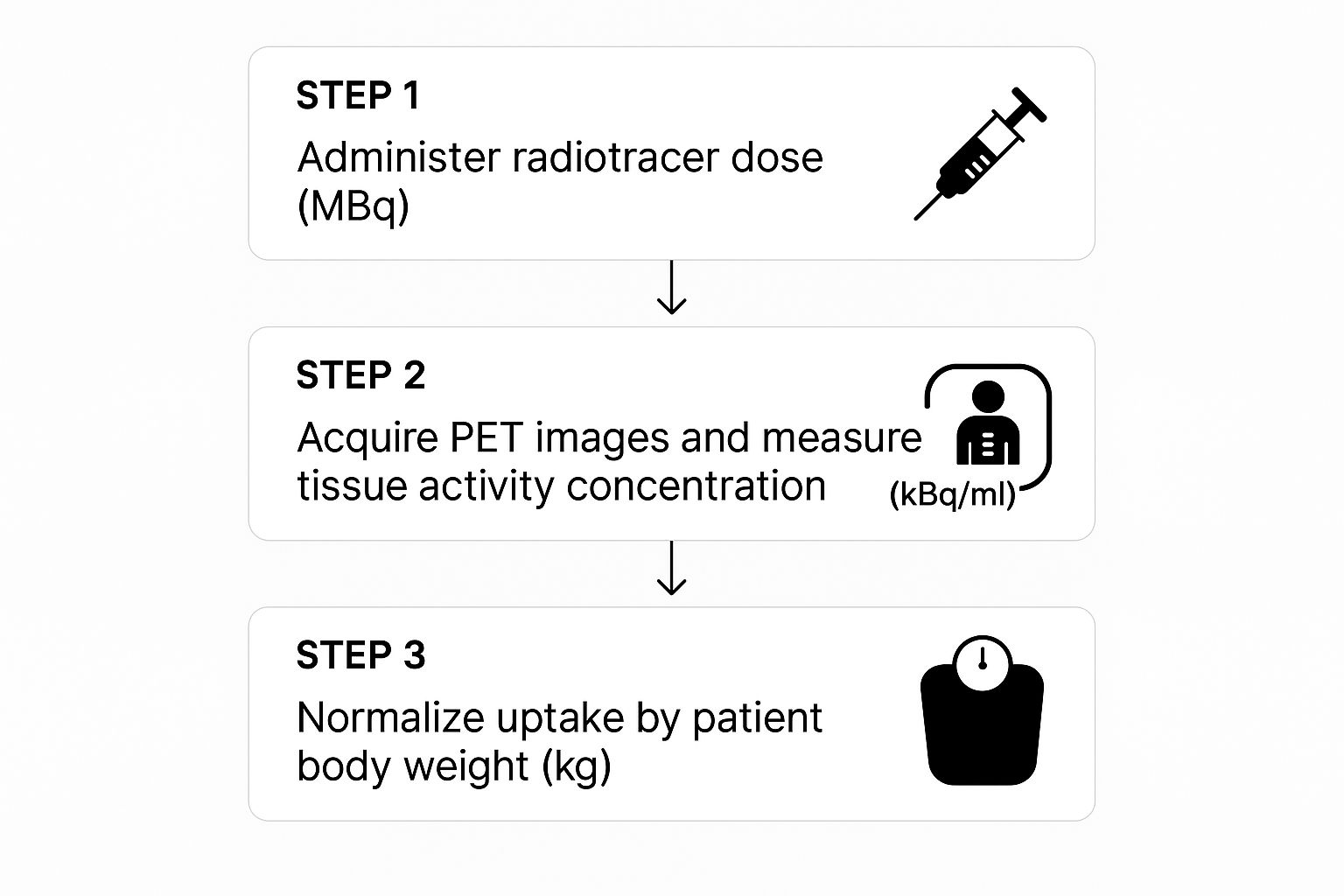
It's all about transforming complex scan data into a straightforward metric that helps guide clinical decisions.
Not All SUVs Are Created Equal
When you look at a radiology report, you’ll probably see an SUV followed by a little subscript, like "max" or "mean." These aren't just details—each one tells a slightly different story and gives clinicians a more complete picture of what they’re seeing.
There are three main types of SUV measurements that doctors look at:
- SUVmax (Maximum SUV): This is the one you’ll see most often. It’s simply the value of the single brightest, or "hottest," pixel within the area of concern. It’s popular because it’s easy to measure and highly repeatable, making it a great benchmark for the most aggressive part of a tumor.
- SUVmean (Mean SUV): This metric gives you the average SUV value across the entire 3D area of the lesion. It provides a better sense of the overall metabolic activity, but there’s a catch. Its accuracy depends on how carefully the radiologist draws the boundary. If a little healthy tissue gets included, it can pull the average down.
- SUVpeak (Peak SUV): Think of this as a more refined version of SUVmax. Instead of relying on a single pixel, which can be thrown off by random signal noise, it averages the values from a small, fixed-size cluster of the hottest pixels. This makes it a more stable and reliable measurement.
So, which one is best? It really depends on the situation. For tracking how well a tumor is responding to treatment, SUVmax is often the go-to for its straightforwardness. But in the world of clinical trials, SUVpeak is becoming more common because it’s less prone to statistical hiccups.
A Real-World Patient Example
Let’s put this into practice. Imagine a patient comes in for a PET scan to investigate a suspicious nodule in their lung. The radiologist finds the spot on the scan and uses their software to draw a "region of interest" around it.
- The software instantly finds the single pixel with the highest tracer uptake and spits out a number: SUVmax = 8.5. This high number is an immediate red flag, suggesting the nodule is highly metabolic and likely cancerous.
- Next, the system calculates the average uptake across the entire nodule, giving an SUVmean = 5.2.
- It might also calculate an SUVpeak = 7.9 by averaging the values from the most active little neighborhood of pixels.
The oncologist then compares these numbers to the patient's healthy tissues. The normal lung tissue might have an SUV around 0.8, and the liver (a metabolically active organ) might be around 2.5. The stark difference between the nodule's high SUVs and these normal background values provides clear, quantitative proof of its aggressive nature. This information is invaluable for deciding the next step, which would likely be a biopsy.
Critical Factors That Influence SUV Measurements
A Standard Uptake Value might look like a simple, concrete number, but it’s anything but. It’s far more like a blood pressure reading—influenced by a dozen different variables at any given moment—than a fixed measurement like your height. For an SUV to be a reliable guidepost in a patient's journey, especially when tracking how well a treatment is working, clinicians have to account for these variables.
These influences generally fall into two buckets: technical factors tied to the PET scanner and the imaging procedure, and biological factors unique to the patient. Understanding both is non-negotiable for interpreting standard uptake values accurately. Without that context, comparing a scan from May to one from September would be like comparing lap times from two completely different race tracks.
Technical Variables in PET Imaging
The nuts and bolts of the PET scan itself—the machine, the software, the timing—play a huge role in the final SUV. Just as two photographers using different cameras and settings will get slightly different pictures of the same scene, different PET scanners can produce varying results.
This is why consistency is everything. While standard uptake values have become incredibly popular for their convenience, their reproducibility can be a real challenge. Things like the scanner model, the image reconstruction settings, and the precise timing of the scan after the tracer is injected can all nudge the final numbers. To get around this, strict adherence to standardized protocols is absolutely essential, particularly when monitoring a patient’s response to therapy over time. It’s the only way to ensure that a change in SUV reflects a genuine biological response, not just technical noise. For a closer look at managing these issues, a review in the American Journal of Roentgenology offers detailed insights on PET/CT imaging standards.
Some of the most critical technical factors include:
- Scanner Calibration: Every PET scanner needs to be meticulously calibrated to ensure its measurements are true. A machine that’s even slightly off can skew the results, making them unreliable.
- Reconstruction Algorithms: The software that turns raw scanner data into a 3D image is incredibly complex. Different algorithms or even different settings on the same software can alter the final SUV.
- Uptake Time: This is the window between injecting the radiotracer and starting the scan. The standard is usually 60 minutes, but even a few minutes' deviation can change how much tracer has settled into a lesion, directly impacting the SUV.
- Dose Administration: The exact amount of radiotracer given to the patient and the precision of that injection are vital. Any small error here throws off the entire calculation, which depends on knowing the precise starting dose.
The goal is to make the technology as invisible as possible. By standardizing every technical detail, clinicians can be more confident that a change in a patient’s SUV is due to a change in their disease, not a change in the machine.
Patient-Specific Biological Factors
You can control technology, but the human body is another story. Several biological factors unique to each patient can have a massive impact on the accuracy and meaning of standard uptake values. This is why patients receive very specific pre-scan instructions.
If you ignore these biological variables, the results can be dangerously misleading. A benign patch of inflammation might light up like an aggressive tumor, or worse, a real tumor might appear deceptively quiet.
Key Biological Influences on SUV
Here are some of the most important patient-related factors that can throw off SUV measurements:
- Blood Glucose Levels: This is the big one. Because the 18F-FDG tracer is a stand-in for sugar, high blood sugar (hyperglycemia) creates a traffic jam. The body's cells, both healthy and cancerous, have more real glucose to feed on, so they take up less of the radioactive tracer. The result? An artificially low and misleading SUV.
- Patient Diet and Fasting: This is why patients are told to fast for at least 4-6 hours before a scan. Eating, especially carbs, spikes insulin and blood glucose, directly interfering with how the tracer is absorbed.
- Recent Physical Activity: A tough workout before a scan can cause major muscle uptake of the FDG tracer. This not only creates "hot spots" in muscles that could be mistaken for disease but also diverts the tracer away from a potential tumor, falsely lowering its SUV.
- Body Composition: The original SUV formula uses total body weight. The problem is, fat tissue barely uses any glucose and doesn't absorb much tracer. For patients with a high body mass index, normalizing the value to their lean body mass (a metric called SUL) often gives a much more accurate picture.
Putting SUV Numbers to Work: What Do They Mean for Patients?
Once a PET scan spits out the numbers, the real detective work starts. A Standard Uptake Value isn't just a piece of data. In the hands of an experienced oncologist or radiologist, it tells a story about what’s happening deep inside a patient's body. These specialists are trained to translate the raw figures into insights that guide some of the most critical decisions in cancer care.
It's easy to get fixated on finding a single, magic number—a clear line in the sand that screams "cancer." But interpreting standard uptake values is far more of an art than a simple calculation. There’s no universal "cancer number." For instance, an SUV of 4.0 might be a major red flag in the lung, but it could be completely normal in the bladder, where the tracer naturally accumulates before being flushed out.
Context is everything. An oncologist never looks at an SUV in a vacuum. Instead, they’re constantly comparing the value to the metabolic activity in nearby healthy tissues. The liver is often used as an internal measuring stick because its metabolic rate is fairly consistent. A lesion is usually only considered suspicious if its SUV is significantly higher than this background hum of normal activity.
The Three Main Jobs of an SUV in Cancer Care
In the clinic, standard uptake values are used to answer three fundamental questions. Each one corresponds to a critical point in a patient's cancer journey, from the first diagnosis to monitoring their health for years to come.
These core applications are:
- Diagnosis and Staging: Helping to figure out if a growth is benign or malignant.
- Monitoring Treatment Response: Seeing if chemotherapy or radiation is actually killing cancer cells.
- Detecting Recurrence: Spotting the earliest signs of cancer coming back after remission.
Let's break down what each of these looks like in the real world.
Diagnosing and Staging Cancer
One of the first hurdles in oncology is figuring out if a suspicious spot found on a CT or X-ray is something to worry about. This is where standard uptake values can bring incredible clarity. A mass that is metabolically "cold"—meaning it has a very low SUV—is often benign, which could save a patient from the stress and risk of an unnecessary biopsy.
On the flip side, a "hot" lesion with a high SUV immediately raises suspicion. A lung nodule with an SUVmax of 7.5, for example, is far more likely to be cancerous than one with an SUVmax of 1.5. This kind of quantitative data helps doctors stage the disease by showing if the cancer has spread to lymph nodes or other organs, which would also light up as areas of high uptake.
An SUV doesn't give a definitive diagnosis by itself—that still requires a tissue sample from a biopsy. Think of it more as a highly accurate map, pointing doctors exactly where they need to look and helping them prioritize the most aggressive-looking areas.
Monitoring How Well a Treatment is Working
Perhaps the most powerful use of standard uptake values is tracking a tumor's response to treatment. Before a patient starts therapy, a baseline PET scan is done to measure the tumor's initial metabolic activity. Then, after a few cycles of chemotherapy or radiation, they'll get another scan.
A sharp drop in the tumor's SUV is fantastic news—it's a strong sign the treatment is working. Imagine a lymphoma patient whose tumor starts with an SUVmax of 12.0. If that number falls to 2.5 after two rounds of chemo, the oncologist can be confident the cancer cells are dying. This gives them near-real-time feedback, allowing them to switch gears if a treatment isn't effective and sparing patients the side effects of a therapy that isn't helping.
Catching Cancer If It Comes Back
For a patient in remission, the fear of recurrence is always there. PET scans and their standard uptake values act as a vigilant surveillance tool. During a routine follow-up, a scan might pick up a new, small area of high metabolic activity.
This could be the very first sign of cancer returning, often long before the patient feels any symptoms or the spot is big enough to see on other types of scans. An isolated hot spot with a rising SUV gives doctors a chance to jump in and act quickly, when the recurrent disease is small and at its most treatable. This early-detection capability is a cornerstone of modern cancer survivorship.
The power of these measurements to predict outcomes is well-established. In fact, the clinical relevance of SUV is so significant that it's a standard tool in major cancer centers for guiding therapy. Higher standard uptake values often correlate with a tougher fight ahead, a finding that helps oncologists fine-tune the intensity of treatment to match the aggressiveness of the tumor. You can read more on how SUV informs patient outcomes at the National Center for Biotechnology Information.
Common Misconceptions About Standard Uptake Values

The Standard Uptake Value is an incredibly useful number in PET imaging, but its very simplicity can open the door to some major misunderstandings. Perhaps the most common—and most dangerous—myth is that a high SUV automatically equals cancer.
Seeing a bright, "hot" spot on a PET scan can be terrifying for patients and families. It's only natural. But it’s critical to remember what this number actually measures: metabolic activity, not cancer itself.
A high SUV simply tells us that cells in a particular spot are gobbling up sugar-based radiotracer at a high rate. While it’s true that aggressive cancer cells are notorious energy hogs, they aren't the only cells in the body with a big appetite. This is why a standard uptake value is never interpreted in a vacuum. It’s just one piece of a much larger diagnostic puzzle.
When High SUVs Are Not Cancer
Many non-cancerous conditions can kick cellular metabolism into high gear, leading to an elevated SUV that can mimic a tumor. Think about your body's own defense and repair crews—they need a ton of energy to do their jobs. When your immune system rushes to fight an infection or heal an injury, those cells become highly active and absorb the FDG tracer just as intensely as a malignant lesion would.
Some of the most common culprits behind a "false positive" high SUV include:
- Infections: An area with a bacterial infection, like pneumonia, or a deep tissue abscess will light up brilliantly on a PET scan.
- Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis, or even just the body’s healing response after surgery can create intense hot spots.
- Benign Growths: Some non-cancerous tumors, known as adenomas, can also be metabolically active and show a high SUV.
The following table gives a clearer picture of just how many non-cancerous conditions can cause an elevated SUV.
Causes of Elevated SUV Besides Malignancy
| Condition Category | Specific Examples | Why It Causes High SUV |
|---|---|---|
| Inflammatory Processes | Arthritis, Sarcoidosis, Post-surgical changes | Immune cells (macrophages, neutrophils) are highly metabolic as they work to repair tissue. |
| Infectious Diseases | Pneumonia, Tuberculosis, Abscesses | Bacteria and the body's immune response both consume large amounts of glucose. |
| Recent Injury | Healing fractures, Bruises, Biopsy sites | The cellular repair process requires significant energy, causing high tracer uptake. |
| Physiological Activity | Brown fat activation, Muscle strain | Active tissues, like muscles after exercise or brown fat responding to cold, burn sugar. |
Recognizing these potential mimics is a core part of a radiologist's expertise in interpreting PET scans.
The Other Side of the Coin: False Negatives
Just as a high SUV isn't a guaranteed sign of cancer, a low SUV doesn't always mean everything is fine. This scenario, known as a "false negative," can happen for a few key reasons. Some cancers are just naturally slow-growing or have a lower metabolic rate, so they don't absorb enough of the sugary tracer to stand out from the normal background activity.
For instance, certain well-known cancers can produce deceptively low standard uptake values:
- Prostate Cancer: Often grows very slowly and may not be particularly FDG-avid.
- Certain Lung Cancers: Well-differentiated adenocarcinomas, for example, can have low uptake.
- Some Kidney Cancers: Renal cell carcinomas are another type that can be tricky to spot with FDG-PET.
The Standard Uptake Value is a guide, not a verdict. It is a powerful tool for flagging areas of concern, but a definitive diagnosis of cancer almost always requires a biopsy—a physical tissue sample examined under a microscope.
At the end of the day, the SUV is a crucial piece of evidence, not the final judgment. It helps point doctors in the right direction, but it’s the combination of this metabolic data with anatomical imaging (like CT or MRI) and a pathologist's expert analysis that ultimately provides a conclusive answer.
What's Next for Quantitative PET Imaging?
The Standard Uptake Value has been a cornerstone of PET imaging for years, but the field is always pushing forward. The big goal now is to make these quantitative measurements even more accurate and universally consistent. Imagine a future where an SUV reading from a scanner in one city is perfectly identical to a reading from another scanner halfway across the world.
That's where major standardization efforts come in. Initiatives like the EARL (EANM Research Ltd) accreditation are leading the charge to harmonize how PET scanners are calibrated and how scans are performed. This isn't just about technical tidiness; it's absolutely crucial for large-scale clinical trials that rely on consistent data from many different hospitals to develop and approve new treatments. By getting every machine to speak the same quantitative language, these programs make the standard uptake value a much more powerful and reliable tool.
AI and Smarter Tracers on the Horizon
The next leap forward is all about artificial intelligence and machine learning. New AI algorithms can now analyze PET scans in ways that were impossible just a few years ago. Instead of just looking at a single SUVmax number, these tools can dig into the subtle patterns and textures within a tumor—a field called radiomics. These features, often invisible to the human eye, can give us incredible new insights into how aggressive a tumor is and how it might respond to a particular drug.
We're shifting from simply asking "how hot is the tumor?" to understanding why it's hot. This is a massive step toward truly personalized medicine.
At the same time, we're moving beyond the trusty 18F-FDG tracer. While FDG is fantastic for tracking glucose metabolism, scientists are developing a whole new generation of radiotracers that target other specific biological pathways.
- Amino Acid Tracers: These are a game-changer for certain brain tumors, which don't always light up brightly with FDG. By tracking protein synthesis instead, we get a much clearer picture.
- Hypoxia Agents: Some parts of a tumor have very low oxygen levels, making them notoriously resistant to radiation. These tracers can pinpoint those stubborn areas so we can adjust treatment accordingly.
- Immune Cell Tracers: This is incredibly exciting stuff. These revolutionary tracers allow us to watch a patient's own immune system in action, showing us if an immunotherapy treatment is successfully rallying the troops to attack the cancer.
These incredible advances aren't making the SUV obsolete. Far from it. The simple, elegant concept of the standard uptake value—quantifying what's happening inside the body—laid the groundwork for all of these next-generation tools. It’s the foundation upon which a future of clearer, more precise diagnostic imaging is being built.
Common Questions About Standard Uptake Values
Even with a good grasp of the science, it's completely normal to have practical questions about what standard uptake values really mean for a patient. Let's walk through some of the most common things people ask after getting their PET scan results.
Does a High SUV Always Mean Cancer?
Not at all. A high SUV is simply a flag for high metabolic activity—it tells us that cells in a particular area are burning through a lot of energy. While it's true that many cancers are energy-hungry, they're not the only culprits.
Think of it this way: your body’s own defense and repair systems can also light up a PET scan. A few common examples include:
- Infections: The body sends a rush of cells to fight off things like an abscess or pneumonia, and that activity shows up as a hot spot.
- Inflammation: Healing from a recent injury, surgery, or even a chronic condition like arthritis can cause a spike in metabolic activity.
- Benign Tumors: Some non-cancerous growths are also metabolically active and can absorb the tracer.
This is why a radiologist never looks at the SUV in a vacuum. They interpret it alongside your medical history, the exact location of the uptake, and findings from other scans. Often, a biopsy is the only way to know for sure.
What’s Considered a Normal or Low SUV?
There’s no universal "normal" number for an SUV because it’s all about context. The value is always relative to the tissue being scanned. To get their bearings, clinicians use healthy organs as an internal benchmark.
For example, a healthy liver typically shows an SUV between 2.0 and 3.0. The background activity in the blood is usually below 2.0. A reading only becomes suspicious when it's significantly higher than the tissue surrounding it.
On the other end of the spectrum, a very low SUV (think under 1.0) points to minimal metabolic activity. This is typical for areas filled with fluid, like simple cysts, or regions where tissue has died (necrosis).
Why Do I Need a Special Diet Before a PET Scan?
Following those pre-scan instructions, like fasting and avoiding sugar, is absolutely critical for getting a clear and accurate result. The tracer used in most PET scans, 18F-FDG, is essentially a radioactive sugar molecule. Your cells—both healthy and cancerous—use sugar for fuel.
If you eat or drink something sugary before your scan, your blood sugar spikes. This makes your healthy cells, especially in your brain and muscles, gobble up the sugary tracer. This can either hide the activity in a potential tumor or create misleading "hot spots" that confuse the reading.
By fasting, you lower your blood sugar and ensure that the most metabolically ravenous cells—the ones doctors are looking for—take up the lion's share of the tracer. This makes them stand out brightly on the scan, leading to a much more accurate standard uptake value.
At PYCAD, we're focused on bringing the power of artificial intelligence to medical imaging, helping to improve diagnostic accuracy and streamline workflows. See how our AI tools are making a difference in healthcare by exploring our work at PYCAD.