Imagine a surgeon getting ready for a difficult operation. Instead of just looking at flat, black-and-white X-ray films, they're holding and rotating a precise, digital 3D model of their patient's actual anatomy. This is exactly what 3D reconstruction CT makes possible—a process that turns standard, cross-sectional CT scan slices into fully interactive, three-dimensional models.
Seeing Anatomy in a New Dimension
This guide is your deep dive into this essential medical imaging process, covering everything from its core principles to its life-saving applications. We'll break down how simple 2D images are stacked and rendered into detailed 3D visualizations. But more importantly, we'll see how doctors are using these models to improve patient outcomes every single day.
Consider this your definitive guide to understanding one of modern medicine's most vital tools.

Why 3D Models Matter in Medicine
A standard computed tomography (CT) scan gives a radiologist a series of individual, flat images. You can think of them like digital slices of bread from a loaf. While incredibly useful, these 2D views force a physician to mentally piece the slices together to figure out the complex spatial relationships between organs, blood vessels, and things like tumors.
The 3D reconstruction CT process completely removes that guesswork. It takes the raw data from the scan and uses powerful software to build a complete, interactive model. This gives medical professionals a clear, intuitive view of the patient’s internal structures that feels more like holding the real thing.
A 3D model lets a surgical team see not just where a tumor is, but exactly how it’s tangled up with nearby critical blood vessels and healthy tissue. This enables a level of pre-operative planning that was simply impossible before.
This leap from 2D interpretation to 3D interaction is a massive step forward in personalized medicine. It allows for a much deeper understanding of each patient's unique anatomical landscape.
The Core Benefits of 3D Visualization
The value of creating a three-dimensional view from CT data is felt across many medical fields, from oncology to orthopedics. The main advantages are clear:
- Improved Surgical Planning: Surgeons can essentially rehearse complex procedures, spot potential challenges, and map out the safest, most effective path for an operation. In liver cancer surgery, for example, a 3D model can calculate the exact remaining liver volume after a tumor is resected, which is critical for the patient's safety.
- Enhanced Diagnostic Accuracy: Seeing structures in 3D often reveals subtle details that are easy to miss on flat images alone. This leads to more accurate diagnoses for complex fractures, vascular conditions, and other tricky pathologies.
- Better Patient Communication: It’s one thing to describe a condition, but it's another to show it. Doctors can use these intuitive models to walk patients through their diagnosis or surgical plan, improving their understanding and helping them feel more involved in their own care.
- Custom Medical Device Design: The data from a 3D reconstruction CT is the blueprint for creating patient-specific implants, like custom cranial plates for skull reconstruction or joint replacements that are a perfect fit.
As we move forward, we'll explore how artificial intelligence is making this entire process faster and more precise, continuing to shape the future of medical imaging and patient care.
From Paper Tape to Pixel-Perfect Models

Before we can really grasp just how incredible today's instant, high-definition 3D visualizations are, we have to go back in time. Picture the early 1970s. The idea of peering inside the human body in three dimensions felt like pure science fiction, but the pioneers of computed tomography were determined to make it a clinical reality. They were working against unbelievable technical odds, yet their foundational efforts gave us the 3d reconstruction ct tools we rely on today.
Their early attempts were slow, clunky, and produced images that look almost primitive by modern standards. But that work was what started everything.
The Dawn of Digital Imaging
The story of 3d reconstruction ct really kicks off in the late 1960s and early 1970s. The very first CT image of a live patient was taken in 1971, the result of a project with a tiny budget of just £69,000 over three years—a shoestring amount for such a revolutionary breakthrough. The first scanners were painfully slow. A single scan took nine full days to capture, and then a computer needed 2.5 hours to crunch the numbers and produce just one image. You can explore a more detailed account of these early days and their challenges on the PMC website.
The images themselves were incredibly rough, initially displayed as a mere 32×32 pixel matrix. Even as technology improved to an 80×80 resolution, the quality was nothing like what a doctor would accept today. Making that jump required shifting the complex calculations from prototype machines to much more powerful mainframe computers, showing how tightly linked imaging and computing power have been from the start.
A World of Tapes and Oscilloscopes
It's hard to imagine now, but in the 1970s, there were no hard drives or cloud servers for patient data. The storage "medium" for one of those grainy 80×80 pixel images was a physical roll of paper tape that stretched 90 meters long. Just managing and accessing patient scans was a massive physical chore.
Visualizing the images was just as cumbersome. Technicians didn't have high-res monitors; they peered at oscilloscope displays. To get a permanent copy, they would take a Polaroid picture of the screen, a process that sometimes required an exposure of up to 60 minutes.
Think about this: adjusting the brightness or contrast wasn't a quick mouse click. It meant physically rewinding that enormous paper tape and reprocessing all the data from scratch. The whole procedure could take hours.
This look back really puts today's technology into perspective. We’ve come a long way from storing a single, low-res image on a roll of paper to generating a fully interactive 3D model in just a few minutes.
From Obstacles to Opportunities
The limitations of early CT were huge, but they didn't stop the forward march of progress. In fact, they did the opposite. Every roadblock—from slow scan times to clunky data storage—became a new problem that brilliant minds were eager to solve.
The evolution from those first fuzzy pictures to the crystal-clear models used in operating rooms is a powerful story of persistence. Those early struggles directly paved the way for:
- Faster Acquisition: Scan times plummeted from days to seconds.
- Higher Resolution: Image quality shot up exponentially, revealing incredibly fine anatomical details.
- Efficient Workflows: All those tedious, manual steps were eventually replaced with smart, automated software.
Understanding this history gives you a real appreciation for the sophisticated 3d reconstruction ct tools that clinicians now use to plan complex surgeries, diagnose diseases with pinpoint accuracy, and ultimately, save lives.
How 2D Slices Become a 3D Model
So, how do we get from a stack of flat, black-and-white CT images to a dynamic 3D model we can spin around on a screen? It's not magic, but a sophisticated process that turns raw scan data into an incredibly powerful clinical tool.
Think of it like this: a CT scanner gives you hundreds of individual, transparent slides, each with a thin cross-section of an image drawn on it. By stacking them perfectly, the full, solid object suddenly takes shape. This is the core idea behind 3D CT reconstruction. Let’s walk through the three key stages of this journey.
Stage 1: Data Acquisition
Everything begins inside the CT scanner. As the gantry rotates, it captures a series of cross-sectional images—often hundreds or even thousands of them. Each image is a thin "slice" of the patient's anatomy, stored in the universal DICOM (Digital Imaging and Communications in Medicine) format.
The quality of the final 3D model hinges on this first step. The thinner the slices and the smaller the gap between them, the more detailed the final reconstruction will be. It's like sculpting with very fine layers of clay versus thick, chunky blocks; the finer layers allow for much more intricate and accurate detail.
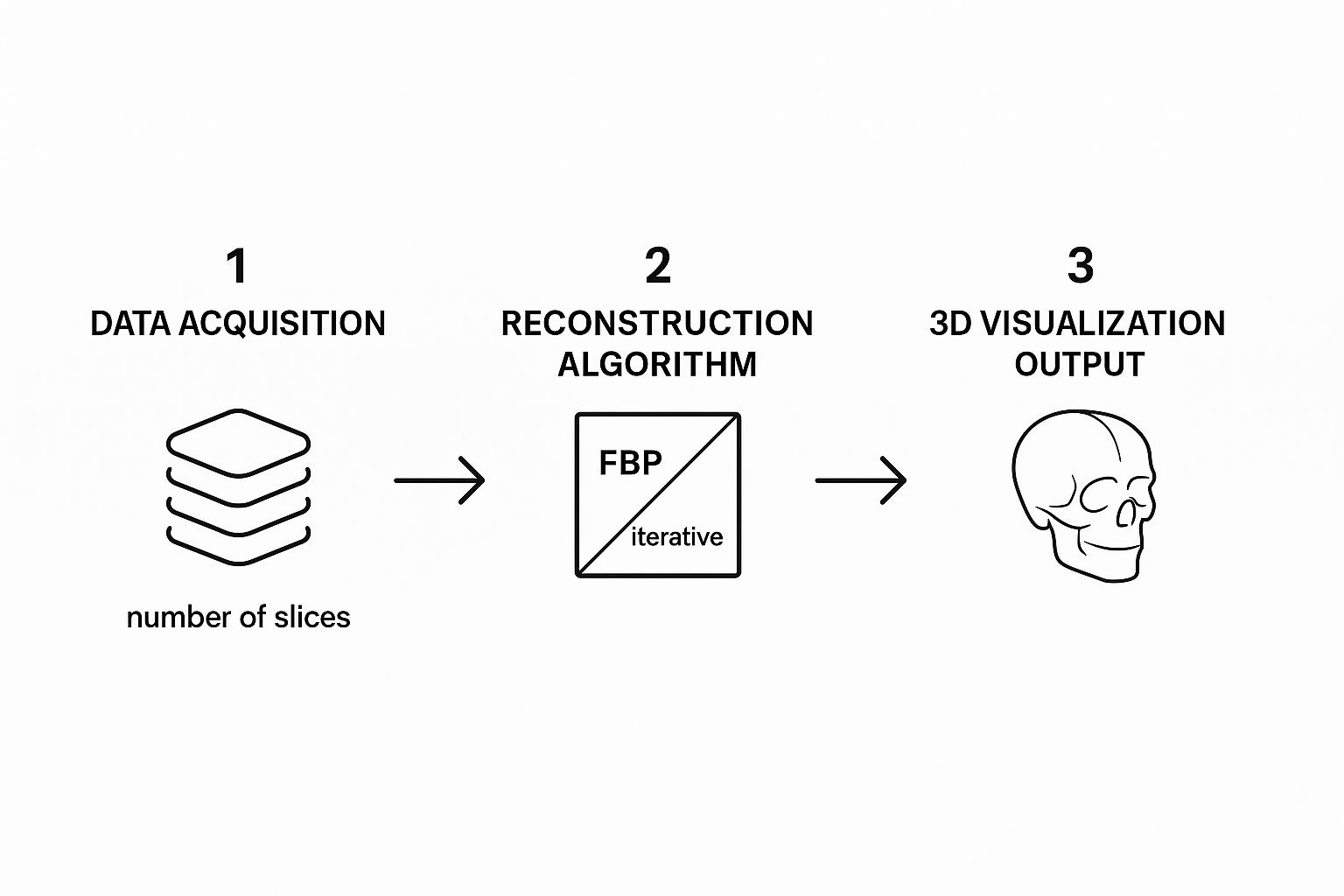
As you can see, the path from raw data to a useful 3D model involves a critical choice of reconstruction technique. This decision directly shapes the clarity and utility of the final visualization.
Stage 2: Segmentation
With the 2D slices ready, the next phase is segmentation. This is where we tell the software which pixels belong to which anatomical structure. It’s like a high-stakes digital coloring book, where a specialist—or increasingly, an AI— meticulously outlines specific tissues in each slice.
CT scans show different tissues based on their density. Bone is bright white, air is black, and soft tissues fill the gray spectrum. Segmentation is the process of defining these areas, telling the software, "All these bright white pixels are bone," or "This specific cluster of gray pixels is the kidney."
Segmentation is often the most demanding and time-consuming part of the workflow. The accuracy of the final 3D model is entirely dependent on how well each structure is isolated.
Without this step, you’d just have a block of undifferentiated data. By carefully segmenting bones, organs, and blood vessels, we can view them individually or see exactly how they relate to one another in 3D space.
Stage 3: Rendering and Visualization
The final step is rendering, where the software takes all the segmented 2D slices and builds them into a cohesive 3D object. It stacks the "colored-in" layers and uses powerful algorithms to generate a model you can interact with. The two main approaches for this are Surface Rendering and Volume Rendering.
Here’s a look at how these fundamental 3D CT reconstruction techniques work and where they shine.
Core Techniques in 3D CT Reconstruction
A comparison of the primary methods used to generate 3D models from CT scan data, outlining their processes and best-use cases.
| Technique | How It Works | Best For Visualizing |
|---|---|---|
| Surface Rendering | Identifies the outer boundary of a segmented structure and builds a solid-looking 3D shell. | The shape and surface details of individual structures, like bones for fracture planning or the exterior of an organ. |
| Volume Rendering | Assigns color and transparency values to all the data points (voxels), creating a semi-transparent model. | Complex relationships, like seeing a tumor inside an organ or tracing blood vessels through surrounding tissue. |
Essentially, Surface Rendering gives you a solid-looking object, perfect for examining the shape of a bone for a complex fracture repair. Volume Rendering, on the other hand, provides incredible depth. It allows a surgeon to see a tumor inside the liver while simultaneously visualizing the delicate network of blood vessels running through it.
These three steps—acquisition, segmentation, and rendering—work together to convert a flood of 2D data into a clear, interactive anatomical map. This map gives medical teams the insight they need to plan safer procedures, make more confident diagnoses, and ultimately improve patient care.
Clinical Applications That Save Lives
The real magic of 3D reconstruction CT isn't in the technology itself, but in how it profoundly changes patient outcomes. We're moving far beyond theory here. These detailed 3D models have become essential tools in operating rooms and clinics everywhere, turning complex medical puzzles into solvable problems. They give medical teams a clear, intuitive roadmap of a patient's internal anatomy, boosting safety and precision in ways we once could only imagine.

The clinical potential was obvious from the very beginning. The first patient CT scan back in October 1971 took a full five minutes for just one 180-degree rotation. From that humble start, the field grew at a dizzying speed. By 1980, the U.S. alone was performing about 3 million CT exams a year, a testament to how quickly it was adopted.
Precision Planning in Oncology
Picture a surgeon preparing to remove a cancerous tumor from a patient's liver. The challenge is twofold: get all of the cancer out, but leave behind as much healthy liver as possible. The amount of remaining functional liver is a critical factor for the patient's survival. On flat, 2D scans, it’s incredibly difficult to see the tumor's exact relationship with major blood vessels or to accurately calculate the future liver remnant.
This is where a 3D reconstruction CT model becomes a game-changer. Take a recent case of a 60-year-old woman with recurrent liver cancer. Her surgical team used a 3D model to precisely map out the liver volumes. The model confirmed that 61.9% of her liver would remain after surgery—a number that gave them the confidence to proceed safely.
The 3D model didn't just show the tumor; it mapped its exact position relative to critical blood vessels. This gave the surgical team a clear guide for a precise removal, directly contributing to a better outcome by minimizing risks.
This is a perfect illustration of how 3D visualization arms surgeons with the clarity they need to tackle incredibly complex procedures.
Revolutionizing Orthopedic and Cranial Surgery
The benefits of 3D reconstruction CT don't stop with soft tissue. In the worlds of orthopedics and maxillofacial surgery, these models are the foundation for creating custom-fit solutions that match a patient's unique anatomy perfectly.
Imagine a patient who has suffered a traumatic skull injury. A neurosurgeon can use a 3D model of the skull to design a patient-specific cranial implant that fits flawlessly into the damaged area. This completely sidesteps the old method of trying to manually shape a generic implant during surgery, saving precious time in the OR and leading to a much better cosmetic result.
The same principle is making a huge difference in other areas:
- Joint Replacements: Orthopedic surgeons can map out complex hip or knee replacements with incredible accuracy, ensuring the implant size and placement are absolutely optimal.
- Complex Fractures: When a bone is shattered into multiple pieces, a 3D model lets surgeons see exactly how the fragments fit together—like assembling a difficult puzzle—before they even make an incision.
- Jaw Reconstruction: After removing part of a patient's jaw due to cancer, surgeons can use 3D models to plan the reconstruction using bone from another part of the body, ensuring a perfect functional and aesthetic fit.
These detailed 3D models are now vital not just for diagnosis, but for creating patient-specific implants and surgical guides. You can explore a variety of additive manufacturing solutions for the medical market to see how this technology is being applied.
Guiding Interventional Radiology
Interventional radiologists do incredible work, navigating tiny catheters and wires through a patient's blood vessels to perform minimally invasive procedures. This demands an exceptional understanding of vascular anatomy.
A 3D reconstruction CT gives them a detailed vascular map, essentially a "GPS" for the human circulatory system. It allows radiologists to chart the safest and most efficient path to treat conditions like aneurysms or blockages. This guidance not only reduces the time a procedure takes but also significantly lowers the risk of complications, making treatments safer and more effective for the patient.
How AI Is Supercharging 3D Reconstruction
The next big jump in 3D reconstruction CT isn't coming from the scanner hardware. It’s happening in the software that brings the images to life. Artificial intelligence, and deep learning in particular, is tackling the single biggest headache in the entire process: segmentation. What used to be a long, tedious manual task is quickly becoming automated and incredibly fast.
Think of an AI model as a highly specialized assistant that has studied millions of CT images. It’s been trained to instantly recognize specific anatomical parts—bones, organs, blood vessels, even tumors—with remarkable accuracy. This brings a speed and consistency to the process that's tough for even the most experienced human to match, especially on complex scans.
Automating the Toughest Part of the Job
Segmentation has always been the bottleneck. This is the part where someone has to manually trace the outlines of structures on slice after slice of a CT scan. For a complex organ or vascular system, this could easily eat up hours of a skilled professional's day.
An AI model? It can often get the same job done in minutes.
This isn't just about moving faster. Automating this step with AI delivers some major wins:
- Unwavering Consistency: When done by hand, segmentation can differ slightly from one person to another, or even from the same person on a different day. AI follows the exact same rules every single time, creating models that are far more standardized and reproducible.
- Higher Case Throughput: When you slash the time it takes to create a 3D reconstruction CT, you can naturally handle more cases. This makes powerful 3D visualizations available to a much wider range of patients.
- A Shift to Higher-Value Work: By taking over the repetitive tracing, AI frees up highly trained technologists and radiologists. They can now spend their valuable time on what really matters: analyzing the finished models, planning surgeries with doctors, and interpreting the most challenging cases.
A Smart Assistant for the Radiologist
AI's contribution goes well beyond just automating tedious tasks. Deep learning models are becoming a powerful second set of eyes, helping radiologists catch subtle details that might otherwise be missed. These systems are masters of pattern recognition at a scale humans simply can't match.
AI can analyze minute changes in tissue density or texture across hundreds of CT slices at once, flagging suspicious spots that could be early signs of disease. It doesn't replace the expert's decision, but it points them in the right direction, saying, "You might want to take a closer look right here."
This partnership is pushing the limits of what a 3D reconstruction CT can do. For instance, some AI algorithms can now analyze the 3D shape and texture of a tumor to help estimate how it might grow or respond to treatment. We're moving from just seeing what is to helping clinicians predict what might happen.
Ultimately, bringing AI into the workflow is about building a smarter, more efficient system. It boosts the abilities of medical experts, reduces the chance of human error on repetitive work, and squeezes a whole new level of insight out of the data that was already there. It's this blend of human experience and machine precision that is shaping the future of medical imaging.
The Future of Medical Imaging
The world of 3D reconstruction CT is anything but static. With computational power exploding and imaging hardware constantly evolving, we're right on the edge of the next big breakthrough. The innovations coming down the pipeline are set to deliver medical images that are not just more detailed, but far more dynamic and interactive than anything we have today. This is steering us toward a future of predictive diagnostics and truly personalized medicine.
Of course, the progress we're seeing now is built on the shoulders of giants—decades of dedicated research and development. But turning these future concepts into clinical reality requires sustained investment. That's why recent developments like funding cuts to biomedical research send a ripple of concern through the entire medical technology community. Without that financial fuel, the engine of innovation can stall.
Seeing More with Photon Counting CT
One of the most exciting advancements on the horizon is photon-counting CT. To understand the leap, think of today's CT scanners as using buckets to catch rain—they tell you the total volume, but nothing about the individual drops. Photon-counting detectors are a whole different game. They measure the energy of every single X-ray photon, essentially counting and sizing each raindrop as it falls.
This fundamental change brings a massive improvement in image quality. Here’s what it means in practice:
- Unprecedented Detail: These scanners can generate images with dramatically higher spatial resolution, allowing us to see tiny anatomical structures that are completely invisible on current scans.
- Reduced Radiation Dose: Because photon-counting detectors are so efficient, they can create these superior images with significantly less radiation. That's a huge win for patient safety.
- Better Material Differentiation: By analyzing photon energies, the scanner can easily tell different materials apart, like distinguishing soft plaque from hardened, calcified plaque within an artery.
Adding the Fourth Dimension: Time
Once you have a perfect 3D model, the next logical step is to see it move. That's where 4D reconstruction comes in, adding the dimension of time to the mix. The technique works by capturing multiple 3D scans in quick succession, creating a short video loop of anatomy in motion. It's no longer just a static picture.
Imagine a cardiologist watching a detailed 3D model of a patient's heart actually beating, allowing them to see precisely how the valves are functioning or how blood flows through the chambers in real time.
The potential here is incredible for understanding dynamic processes in the body. We could analyze how a joint moves under load, watch how the lungs function during a full breath, or track a contrast agent as it flows through the bloodstream. This transforms 3D reconstruction CT from a simple anatomical map into a living, breathing representation of the human body.
Surgery with Augmented Reality Guidance
Peering even further into the future, we'll see the digital models from CT scans merge seamlessly with the physical world through augmented reality (AR). Surgeons, equipped with AR headsets, will be able to project a patient's 3D digital model directly onto their body during an operation. This would give them a kind of real-time, X-ray vision, guiding their instruments with a level of precision and confidence that was once the stuff of science fiction.
Your Questions About 3D CT, Answered
As 3D reconstruction CT becomes a more familiar part of modern medicine, it's natural to have questions. Getting clear, straightforward answers can make a world of difference in how you feel about your own care. Here, we'll walk through some of the most common questions people have about this incredible imaging technology.
Our goal is simply to demystify the process, so you feel informed and confident about the tools being used to help you.
How Is a 3D CT Different From a Standard 2D Scan?
Imagine a standard 2D CT scan as a single photograph of a slice of bread. To understand the whole loaf, a doctor has to look at dozens of these individual pictures and mentally stack them together. A 3D reconstruction CT, on the other hand, uses powerful software to assemble all those flat "slices" into a complete, interactive 3D model of the loaf itself.
This gives your medical team a much more intuitive and complete picture. They can rotate the model, view it from any angle, and truly grasp the spatial relationships between bones, organs, and blood vessels in a way that flat images just can't show.
Will I Get More Radiation to Create the 3D Model?
This is a great question, and the answer is a reassuring one: no, extra radiation is not needed. The 3D model is built using the exact same data collected during your standard CT scan.
The magic happens on a computer after your scan is over. The "reconstruction" is a digital process where software takes the original 2D images and builds the 3D view. You aren't involved in this step and are not exposed to any additional radiation.
Who Actually Builds the 3D Reconstruction?
Putting together a detailed 3D model is a specialized skill. It's usually handled by a CT technologist or a radiologist who has specific training in using advanced 3D imaging software. They are the experts who perform the delicate process of segmentation—digitally separating the specific anatomical structures needed for the model.
It's a team effort. The technologist or specialist prepares the model, which is then used by the radiologist and your primary doctor (like a surgeon or cancer specialist) to analyze your anatomy, plan a procedure, or make a diagnosis.
Can Any CT Scan Be Turned Into a 3D Model?
Technically, many can, but the results won't always be useful. The quality of a 3D reconstruction CT is directly tied to how the initial scan was performed. To create a high-quality 3D model, the original scan needs to be captured using very thin image "slices" with almost no gaps between them.
A CT scan done for a quick 2D check-up might use thicker slices. But when a 3D model is the goal from the start, the CT machine is set to a specific protocol designed to capture the fine details needed for an accurate and clinically valuable reconstruction.
At PYCAD, we build the AI-powered software that makes this kind of advanced 3D reconstruction quicker and more accurate. Our tools help medical professionals by automating the time-consuming segmentation work and improving their diagnostic capabilities. See how we're helping to shape the future of medical imaging.