Demystifying the Medical Device Validation Process
Medical device validation is essential for a successful product launch. It's the foundation of ensuring a device consistently performs its intended function and meets user needs, ultimately contributing to patient safety and positive health outcomes. Validation differs from verification. Verification confirms the device is built correctly according to specifications, while validation focuses on whether you’re building the right device to address real user needs. This is a critical distinction impacting both patient well-being and a company’s bottom line.
Understanding the Stages of Validation
The medical device validation process involves several key stages. Design validation ensures the device's design effectively addresses the clinical need and intended use. This often involves testing prototypes with intended users in simulated or real-world environments.
Process validation confirms that the manufacturing process consistently produces devices meeting pre-defined specifications. Factors like materials, equipment, and environmental conditions are carefully examined.
Finally, product verification checks that the finished product meets all design outputs and specifications.
These stages are interconnected and build upon each other. A robust design validation process, for example, can streamline process validation by minimizing design flaws that might impact manufacturing consistency. This interconnectedness highlights the importance of a holistic approach to the entire validation process.
Why Validation Matters
Effective validation is crucial for several reasons. Primarily, it ensures patient safety by minimizing the risk of device malfunction or unintended consequences. A well-validated device performs reliably and predictably, building confidence in both healthcare professionals and patients.
Validation also minimizes the potential for costly remediation or product recalls. Addressing potential issues early in development significantly reduces the financial and reputational damage that can result from post-market problems.
Finally, successful validation can accelerate time-to-market. Demonstrating regulatory compliance and proving device efficacy allows companies to expedite the approval process and launch their products sooner. The medical device validation process encompasses design validation, process validation, and product verification. In North America, these processes are heavily regulated, with the FDA playing a critical role in ensuring adherence to stringent standards.
The use of risk-based approaches and statistical methods in process validation is becoming increasingly common, as emphasized by FDA guidelines, which provide helpful frameworks for planning and documenting validation processes. This helps address the complexities of medical device manufacturing, such as variable production volumes and destructive testing, ensuring that devices meet high safety and quality benchmarks. Explore this topic further: Learn more about medical device validation process
Real-World Validation Strategies
Leading medical device companies employ various strategies to optimize their validation processes. Risk-based validation focuses resources on the areas of highest risk. By prioritizing potential hazards and vulnerabilities, companies allocate validation efforts more effectively, maximizing efficiency without compromising safety.
Close collaboration between validation teams and regulatory bodies is also crucial. Early and frequent communication with regulators can identify potential compliance issues early, minimizing delays and rework during the approval process.
Effective documentation is also essential. Clear, concise, and traceable documentation provides evidence of compliance, supports audits, and facilitates knowledge transfer within the organization. This documentation should be seen not just as a regulatory requirement, but as a valuable tool for continuous improvement and process optimization. By adopting these strategies, companies can navigate the medical device validation process more confidently and efficiently.
Navigating the Regulatory Maze With Confidence

The regulatory landscape for medical devices is complex and constantly changing. Successfully navigating this requires a deep understanding of applicable frameworks, from the FDA in the United States to the MDR/IVDR in Europe, as well as other global regulations. This section explores key elements of these frameworks, offering practical advice from regulatory affairs experts experienced in bringing medical devices to market.
Understanding the Core Requirements
One of the most critical aspects of regulatory compliance is understanding what reviewers prioritize. Many companies get caught up in "documentation theater," creating excessive paperwork that doesn't enhance the validation process. Instead, focus on demonstrating that your medical device validation addresses safety and efficacy. Clear, concise documentation directly linking design inputs to validation results is more valuable than lengthy, jargon-filled reports.
Device classification also significantly impacts your validation strategy. Higher-risk devices demand more rigorous testing and documentation. Understanding these classifications and their requirements is crucial for efficient resource allocation. This involves knowing not only what to test, but how to test, ensuring alignment with regulatory expectations.
Harmonization and Streamlined Approaches
While regulatory frameworks differ across regions, harmonization efforts are underway. This means certain aspects of medical device validation can be streamlined for multiple markets, potentially reducing development time and costs. However, carefully analyze each target market's specific requirements to ensure compliance, even within harmonized areas.
The global medical device validation market is experiencing substantial growth. Reaching USD 1.04 billion in 2023, it's projected to reach USD 1.13 billion by 2024. This growth stems from increasingly stringent regulatory standards, technological advancements, and the need to demonstrate robust safety and efficacy. The implementation of MDR and IVDR in Europe since 2021 and 2022, respectively, are key drivers, emphasizing the importance of validation for market access. Europe, particularly Germany with its strong Notified Body infrastructure, plays a significant role. Discover more insights about the medical device validation market
Building Relationships With Regulators
Building productive relationships with regulatory bodies is invaluable. Early, open communication can prevent misunderstandings and proactively address potential issues. This collaborative approach helps avoid costly delays caused by deficiency letters, which can significantly set back product launches. Proactive engagement allows companies to anticipate regulatory concerns and adapt validation strategies accordingly.
By understanding core requirements, leveraging harmonization, and fostering strong relationships with regulators, manufacturers can navigate the regulatory maze with confidence, ensuring both compliance and efficient time-to-market.
Practical Advice for Validation Success
Here are some practical tips for a robust validation process:
- Define clear objectives: Begin with a well-defined validation master plan outlining scope, objectives, and acceptance criteria.
- Risk-based approach: Prioritize validation activities based on the device's risk profile, with higher-risk features requiring more rigorous testing.
- Thorough documentation: Maintain meticulous records of all activities, including test protocols, results, and deviations.
- Traceability: Establish clear traceability between user needs, design inputs, and validation results.
- Regular communication: Engage with regulatory bodies throughout the process to address questions and concerns proactively.
By focusing on these strategies, manufacturers can build a robust validation process that meets regulatory requirements and supports a successful product launch.
To further understand the varying requirements across the globe, the following table provides a comparison:
A brief explanation about this table – It summarizes key validation requirements and expectations across major regulatory jurisdictions. It highlights critical differences and similarities to aid in understanding the global regulatory landscape.
| Global Regulatory Requirements for Medical Device Validation |
|---|
| Regulatory Body/Region |
| — |
| US FDA |
| European Union |
| Japan PMDA |
| Health Canada |
Key insights from the table above: Regulations vary significantly across regions, emphasizing the importance of tailoring validation strategies to each target market. While harmonization efforts are ongoing, specific requirements and documentation expectations remain distinct. Staying updated on recent changes is crucial for maintaining compliance.
Mastering the Validation Journey: From IQ to PQ
The medical device validation process is a structured, multi-phased journey. It ensures a device consistently performs as intended. This rigorous process is crucial for both patient safety and regulatory compliance. It goes beyond simple checklists; it's about building confidence in the device's real-world performance. This section explores the key phases: Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ). We’ll also examine how successful companies approach each stage.
Installation Qualification (IQ)
The IQ phase confirms the device is correctly installed according to the manufacturer's specifications. This includes verifying all components are present and the installation environment meets requirements. It also ensures the device is configured correctly. Think of it like assembling furniture: all parts must be present and assembled correctly before use. This fundamental step lays the groundwork for subsequent validation phases.
Operational Qualification (OQ)
Once installed, the OQ phase assesses the device’s operational capabilities. This demonstrates the device functions according to its operational specifications within the intended operating range. For example, if the device is a ventilator, OQ verifies its ability to deliver the correct air volumes and pressures. This stage ensures reliable operation before real-world usage testing.
Performance Qualification (PQ)
PQ, the final stage, confirms the device performs as expected under real-world conditions. This involves testing with representative user profiles and simulated usage scenarios. Continuing the ventilator example, PQ might involve testing with simulated patients mimicking different respiratory conditions. Regulatory requirements often drive validation efforts. To navigate these effectively, consider established automation testing best practices. This final step connects all previous phases, proving the device’s effectiveness and safety.
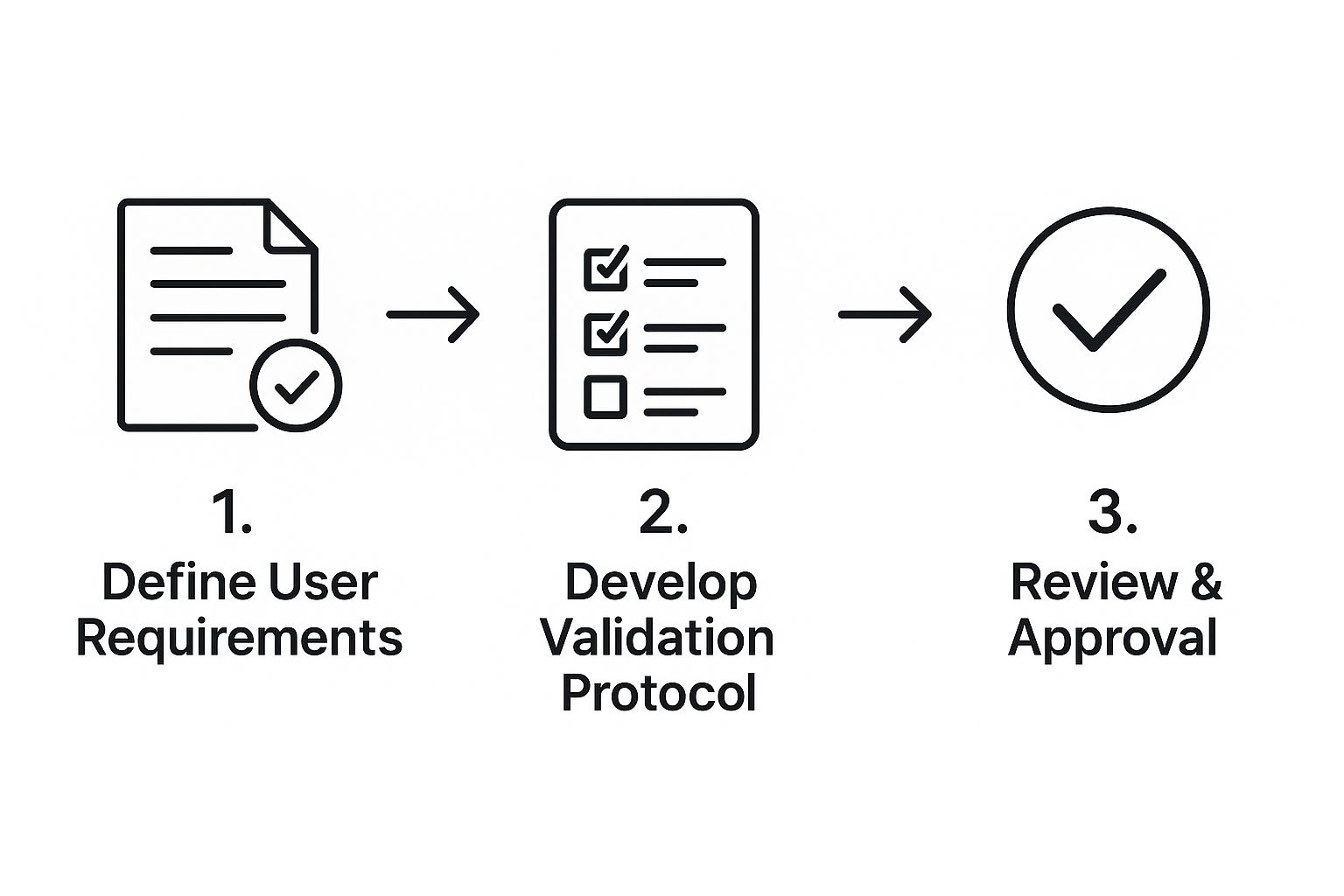
The infographic above visualizes the medical device validation process. It begins with defining user requirements and culminates in reviewing and approving the validation protocol. This highlights the iterative nature of the process, ensuring user needs drive development and thorough protocol review.
Building Bulletproof Validation Protocols
Effective validation hinges on well-designed protocols reflecting real-world use. Leading validation teams establish meaningful acceptance criteria. These are pre-defined standards determining whether a device passes or fails a test. These criteria must balance statistical rigor with practical considerations. Determining appropriate sample sizes is also crucial. Over-testing increases costs and timelines, while under-testing jeopardizes the validity of the results.
Managing validation across distributed teams adds complexity. Clear communication, well-defined roles, and centralized documentation systems are essential for consistency and efficiency. Software validation presents unique challenges in today’s medical device industry. The increasing reliance on software makes software validation a critical area. Robust testing methodologies, meticulous documentation, and a thorough understanding of software development lifecycles are critical for success. Incorporating these strategies allows companies to develop a strong validation process that minimizes risks and maximizes efficiency.
To better understand the validation phases, let's examine the following table:
Validation Phases and Key Activities
Overview of major validation stages with corresponding activities, deliverables, and common challenges
| Validation Phase | Key Activities | Required Documentation | Common Challenges | Best Practices |
|---|---|---|---|---|
| Installation Qualification (IQ) | Verify components, environment, and configuration | Installation checklist, manufacturer specifications | Missing components, unsuitable environment | Pre-installation checks, clear documentation |
| Operational Qualification (OQ) | Test device functions within operating range | Test protocols, operational specifications | Device malfunction, deviations from specifications | Calibrated equipment, standardized procedures |
| Performance Qualification (PQ) | Test device under real-world conditions | Test reports, user profiles, simulated usage scenarios | Unrealistic scenarios, insufficient sample size | Representative user profiles, statistically sound sample sizes |
This table summarizes the key activities, required documentation, common challenges, and best practices for each validation phase. By understanding these elements, organizations can develop more robust and efficient validation processes. This contributes to the overall safety and efficacy of medical devices, ultimately benefiting both patients and healthcare providers.
Risk-Based Validation: Smarter Approach, Better Results
Validating every single part of a medical device with the same level of scrutiny isn't the most efficient or effective way. A risk-based validation strategy concentrates resources where they have the biggest impact, aligning validation efforts with the potential effects on patient safety and how well the device works. This approach not only uses resources better but also makes the entire medical device validation process more streamlined.
Assessing Risk: The Foundation of a Smarter Strategy
The first step in risk-based validation is a thorough risk assessment. This means identifying potential hazards associated with the device and analyzing how likely they are to occur and how serious the harm could be. This isn't just a theoretical exercise; it's a practical look at how the device could fail and what would happen if it did. This assessment, often following the guidelines of ISO 14971, provides a structured way to understand and reduce risks.
This means that higher-risk device aspects, such as those directly affecting patient safety or critical functions, get more rigorous validation. Lower-risk elements can be validated with less intensive methods, saving time and resources. For example, a software algorithm controlling drug delivery would require far more validation than a cosmetic aspect of the device's user interface.
Implementing Risk-Based Validation: Practical Techniques
Figuring out the right level of validation for each part of the device is crucial. This requires careful thought about the risk assessment findings and their potential impact on patient safety. A common approach is to create a risk matrix that connects the likelihood and severity of harm to specific validation activities. This creates a visual representation of the risks and guides the creation of specific validation plans.
This lets companies prioritize validation efforts, ensuring critical device aspects receive the attention they need while avoiding unnecessary testing on lower-risk elements. The global medical device validation and verification market is expected to reach USD 2059.7 billion by 2034, growing at a CAGR of 11.5%. This highlights the increasing importance of efficient validation strategies. Find more detailed statistics here.
Documentation: Demonstrating Due Diligence
Documenting your risk-based decisions is essential for showing regulatory bodies that you've done your homework. This documentation needs to clearly connect the risk assessment findings to the chosen validation activities, creating a clear and auditable record. Regulators can then easily see the reasoning behind your validation strategy and confirm that you've taken the right steps to address potential risks. For example, documenting the risk analysis of a new device provides valuable information for validation and testing.
This not only satisfies regulatory requirements but also provides valuable internal records. It allows for continuous improvement of the validation process by recording what you've learned and providing a structure for future validations. This transparent documentation approach supports organizational learning and ensures validation efforts consistently align with risk.
Overcoming Challenges: Embracing Change
Shifting to a risk-based approach can sometimes encounter resistance within an organization. Some teams may be used to traditional, "validate everything" methods. This means education and communication are vital for getting everyone on board and making sure they understand the advantages of risk-based validation. This requires open communication, clearly explaining the reasons behind the approach, and demonstrating its effectiveness.
However, the benefits of risk-based validation are clear: increased efficiency, lower costs, and a more targeted approach to ensuring patient safety. By proactively addressing potential challenges and promoting a culture of continuous improvement, companies can successfully implement risk-based validation and achieve its full potential. This move towards a more strategic and efficient validation approach is essential for staying competitive in the medical device field.
Documentation That Works: Beyond Regulatory Theater
Medical device validation documentation can sometimes feel like a chore, a performance put on for auditors. But effective documentation is much more than a regulatory requirement. It's a powerful tool for ensuring product quality and streamlining the entire validation process. This section explores practical ways to create documentation that serves both purposes.
Validation Master Plans: Your Roadmap to Success
A Validation Master Plan (VMP) is the cornerstone of your validation efforts. It's not a static document, but a dynamic roadmap that guides all validation activities. A well-structured VMP outlines the overall validation strategy, including the devices covered, the phases of validation, and the responsibilities of each team member.
This shared understanding keeps everyone aligned and working towards a common goal. For instance, a VMP could specify the necessary testing for each device component, guaranteeing comprehensive coverage and leaving no room for uncertainty.
Protocols That Work: Balancing Thoroughness and Usability
Validation protocols require a delicate balance. They must be thorough enough to ensure consistent execution, yet clear and concise enough to be easily followed. Think of them as detailed recipes: all ingredients and steps must be listed, but the instructions shouldn't be overly complicated.
This balance ensures the validation process is both rigorous and efficient. For example, including step-by-step instructions with clear diagrams within a protocol can guide testers effectively, minimize ambiguity, and promote consistent execution.
Traceability Matrices: Connecting the Dots
Traceability matrices are essential for demonstrating the relationships between user needs, design inputs, and validation results. They provide evidence that your device fulfills its intended purpose and meets regulatory requirements. Visualizing these connections helps simplify complex relationships and track the entire validation process.
A good traceability matrix acts like a detective's board, linking all the pieces together. It also highlights any gaps in the documentation, ensuring comprehensive coverage and minimizing the risk of oversight.
The Power of Electronic Systems
Electronic systems offer significant advantages for managing validation documentation. Electronic document management systems can streamline workflows, improve data integrity, and simplify version control, reducing the risk of errors and lost information.
Imagine a centralized, searchable database replacing mountains of paperwork. This system, accessible to authorized personnel from anywhere, allows for real-time collaboration, streamlined reviews, and enhanced efficiency.
Preparing for Regulatory Inspections
Effective documentation is crucial for successful regulatory inspections. By clearly demonstrating compliance with all applicable regulations, you build trust with regulators and minimize potential delays. This means preparing documentation that is complete, accurate, and easily accessible.
Think of it as preparing for an exam: having all the answers at your fingertips demonstrates mastery of the subject matter. This proactive approach not only streamlines the inspection process, but also reinforces a culture of quality within your organization.
Practical Techniques for Documentation Excellence
Maintaining excellent documentation requires a proactive approach. Regular reviews help identify and address any missing information or inconsistencies. A robust version control system is also critical, especially when collaborating with multiple teams, preventing confusion and ensuring everyone uses the latest documents.
Finally, explore how technology can reduce documentation burden. Electronic signatures, automated report generation, and other tools can streamline the process without compromising compliance. These practical techniques ensure your documentation truly supports product quality and regulatory success.
Manufacturing Excellence: Process Validation That Delivers
The most innovative medical device is useless without consistent manufacturability. This section explores process validation, a crucial part of medical device validation, ensuring reliable and repeatable manufacturing that meets pre-defined specifications. We’ll examine practical strategies from experienced manufacturing engineers, focusing on the three stages defined by FDA guidance: process design, process qualification, and continued process verification.
Process Design: Building a Solid Foundation
Process design creates the foundation for successful manufacturing. This stage centers on identifying critical process parameters (CPPs). These parameters, such as temperature, pressure, or time, significantly influence the final product’s quality. Think of baking a cake: oven temperature and baking time are CPPs directly affecting the final product. Carefully defining these CPPs and their acceptable ranges establishes the basis for a robust and repeatable process.
This also includes selecting appropriate materials and equipment. Material variations can affect final product performance, requiring careful selection and quality control. Equipment characteristics also play a vital role. Ensuring equipment operates within specified parameters is essential for consistent results.
Process Qualification: Proving the Process
Process qualification confirms the manufacturing process consistently creates devices that meet specifications. This stage involves rigorous testing and data analysis, demonstrating that the chosen CPPs, materials, and equipment reliably produce acceptable devices.
This stage often comprises three sub-stages: Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ). IQ confirms equipment is installed and functions according to specifications. OQ verifies the process operates within defined parameters. PQ proves the process consistently delivers devices meeting all quality and performance criteria. Choosing appropriate sample sizes for these tests is critical, balancing statistical validity and cost-effectiveness.
Continued Process Verification: Maintaining Control
Maintaining a validated state demands ongoing attention. Continued process verification ensures the manufacturing process remains in control over time. This involves regularly monitoring CPPs and product quality attributes. Consider this routine maintenance: consistent monitoring helps manufacturers identify and address potential problems early.
This also includes using effective change management processes. Any manufacturing process changes, like new equipment or modified parameters, require careful evaluation and re-validation to prevent negative impacts on product quality or regulatory compliance. For more detailed information, refer to this Documentation about managing documentation for regulatory needs.
Statistical Techniques for Process Validation
Statistical techniques are essential for process validation. Techniques like process capability analysis help determine the process’s capacity to consistently meet specifications, providing a quantitative measure of the process’s consistency and predictability.
Analyzing validation data requires statistical methods. These methods provide valuable insights, identify trends, and highlight potential problems. This data-driven strategy allows manufacturers to make informed decisions, continuously improve the process, and maintain consistent product quality. By integrating robust process design, comprehensive qualification, and vigilant monitoring, manufacturers establish and maintain control, consistently producing high-quality medical devices meeting stringent regulatory standards.
Future-Proofing Your Validation Strategy
The medical device validation process isn't a fixed target. It's a constantly shifting landscape shaped by technological advancements and evolving regulatory expectations. This section explores emerging validation challenges and how forward-thinking organizations are preparing for the future of medical device validation.
Validating Emerging Technologies: AI, Connectivity, and Combination Products
New technologies like Artificial Intelligence (AI), connected healthcare devices, and combination products present unique validation challenges. AI-enabled devices, for example, require validation of their algorithms and machine learning models, ensuring they perform reliably and consistently across diverse datasets. This adds a layer of complexity to the traditional medical device validation process.
Artificial Intelligence (AI) in healthcare has introduced new considerations for validation, particularly regarding algorithm reliability and consistency.
Connected healthcare technologies raise cybersecurity concerns. Validation must address data integrity, privacy, and protection against unauthorized access. This means incorporating cybersecurity testing and risk assessments into the validation strategy. Additionally, combination products, which combine drugs, devices, and/or biological products, require validation that considers the interactions between these components, further complicating the process.
Adapting to Regulatory Changes
Regulatory bodies are constantly adapting their expectations for these innovative technologies. Staying informed about these changes is critical for maintaining compliance. This means actively monitoring regulatory updates, participating in industry discussions, and engaging with regulatory bodies to understand their evolving requirements. For example, the FDA's guidance on AI in medical devices is constantly being updated, requiring companies to adapt their validation strategies accordingly.
Regular communication with regulatory bodies and active participation in industry discussions are crucial for staying ahead of regulatory changes.
Building Adaptable Validation Capabilities
Leading companies are building adaptable validation capabilities that can flex with changing requirements. This involves implementing modular validation processes, leveraging automation, and adopting a risk-based approach. Modular processes allow for easy modification and adaptation to new technologies or regulations.
Automation streamlines repetitive tasks, improving efficiency and reducing errors. A risk-based approach focuses resources on the areas of highest risk, maximizing impact while minimizing unnecessary testing. Investing in validation infrastructure and training, building internal expertise, and establishing robust quality management systems are all key elements of this approach. By building these adaptable capabilities, companies can stay ahead of the curve, ensuring their validation strategies remain effective and compliant in a constantly evolving landscape. This proactive approach enables them to embrace new technologies and market opportunities while maintaining the highest standards of safety and quality.
Practical Recommendations for Staying Ahead
Here are some practical recommendations for future-proofing your medical device validation process:
- Embrace a continuous learning culture: Stay up-to-date with the latest regulatory guidance and technological advancements.
- Invest in validation automation tools and technologies: Streamline processes and improve efficiency.
- Develop robust risk management strategies: Prioritize validation efforts based on risk levels.
- Build strong relationships with regulatory bodies: Facilitate communication and address potential concerns proactively.
- Foster cross-functional collaboration: Ensure alignment between validation, engineering, and other relevant teams.
By implementing these strategies, medical device companies can confidently navigate the evolving validation landscape, ensuring both compliance and efficiency in their product development processes.
Ready to streamline and enhance your medical device validation process? PYCAD, a leading provider of AI-powered solutions for medical imaging, offers comprehensive support for data handling, model training, and deployment. From data annotation and anonymization to deploying trained models and creating MVP UIs, PYCAD empowers medical device manufacturers to optimize their validation strategies and achieve regulatory compliance. Learn more about how PYCAD can help you navigate the complexities of medical device validation and accelerate your time-to-market at https://pycad.co.






