Understanding Medical Image Registration Fundamentals
Medical image registration is a crucial process in modern medical imaging. It involves aligning two or more images of the same patient, which may be taken at different times, from different angles, or even using different imaging methods (like a CT scan and an MRI). This alignment allows doctors to compare and combine information from these various sources for more accurate diagnoses and treatment plans. Think of it like trying to compare two slightly offset photos of the same landscape – image registration digitally shifts one image to perfectly overlay the other, revealing subtle changes or hidden details.
Core Principles of Image Registration
Medical image registration algorithms work by identifying matching anatomical features or patterns across the multiple images. This identification process relies on complex mathematical transformations. These transformations manipulate one image to align it with another, similar to adjusting the position and orientation of a puzzle piece to fit correctly. The accuracy of this alignment is critical for patient care, ensuring doctors have the clearest possible understanding of a patient's condition. For instance, accurate registration is essential for tracking tumor growth over time or for planning complex surgical procedures.
Transformation Models and Similarity Metrics
There are various types of transformations, each suited to different clinical situations. Rigid transformations involve simple rotations and translations, and are well-suited for aligning images of rigid structures like bones. Imagine aligning two X-rays of a skull; a rigid transformation would be sufficient to overlap them. However, soft tissues can deform and change shape, requiring more complex deformable transformations. These sophisticated transformations account for bending and stretching, ensuring precise alignment even in challenging cases.
Similarity metrics also play a vital role. They measure how well the two images match after the transformation is applied. A high similarity score indicates a strong alignment. Medical image registration has advanced considerably over time, particularly with the rise of digital radiology. The introduction of computed tomography (CT) in 1971 marked a key moment in the development of digital radiology. This shift to digital imaging paved the way for more precise image registration techniques, which are essential for aligning images from different modalities or across different time points. Explore this topic further here.
Different Approaches to Image Registration
Image registration techniques can be broadly classified into intensity-based and feature-based methods. Intensity-based methods focus on the pixel values within the images, looking for transformations that maximize the similarity of corresponding pixel intensities. Feature-based methods, conversely, identify specific anatomical landmarks or features in the images and use these to guide the registration. Each approach has its own advantages and disadvantages, and the best choice depends on the particular clinical application.

How Medical Image Registration Evolved Into Today's Game-Changer
Medical image registration, the process of aligning multiple medical images, has seen incredible progress. From its humble beginnings to the advanced techniques used today, its journey showcases a constant push for better diagnostics and patient care. The development of medical imaging technologies has been fundamental to the growth of image registration. The discovery of X-rays in 1895 paved the way for later imaging modalities like CT scans and MRI.
MRI, first used clinically in 1980, provides detailed soft tissue images crucial for accurate registration and analysis. Learn more about developments in medical imaging here.
This continuous evolution has transformed medical image registration from a manual, time-intensive process to a precise, automated tool. Initially, image alignment relied heavily on manual adjustments, often using physical markers or anatomical landmarks.
This method was not only laborious but also susceptible to human error. The transition to digital imaging, however, set the stage for more accurate and efficient approaches.
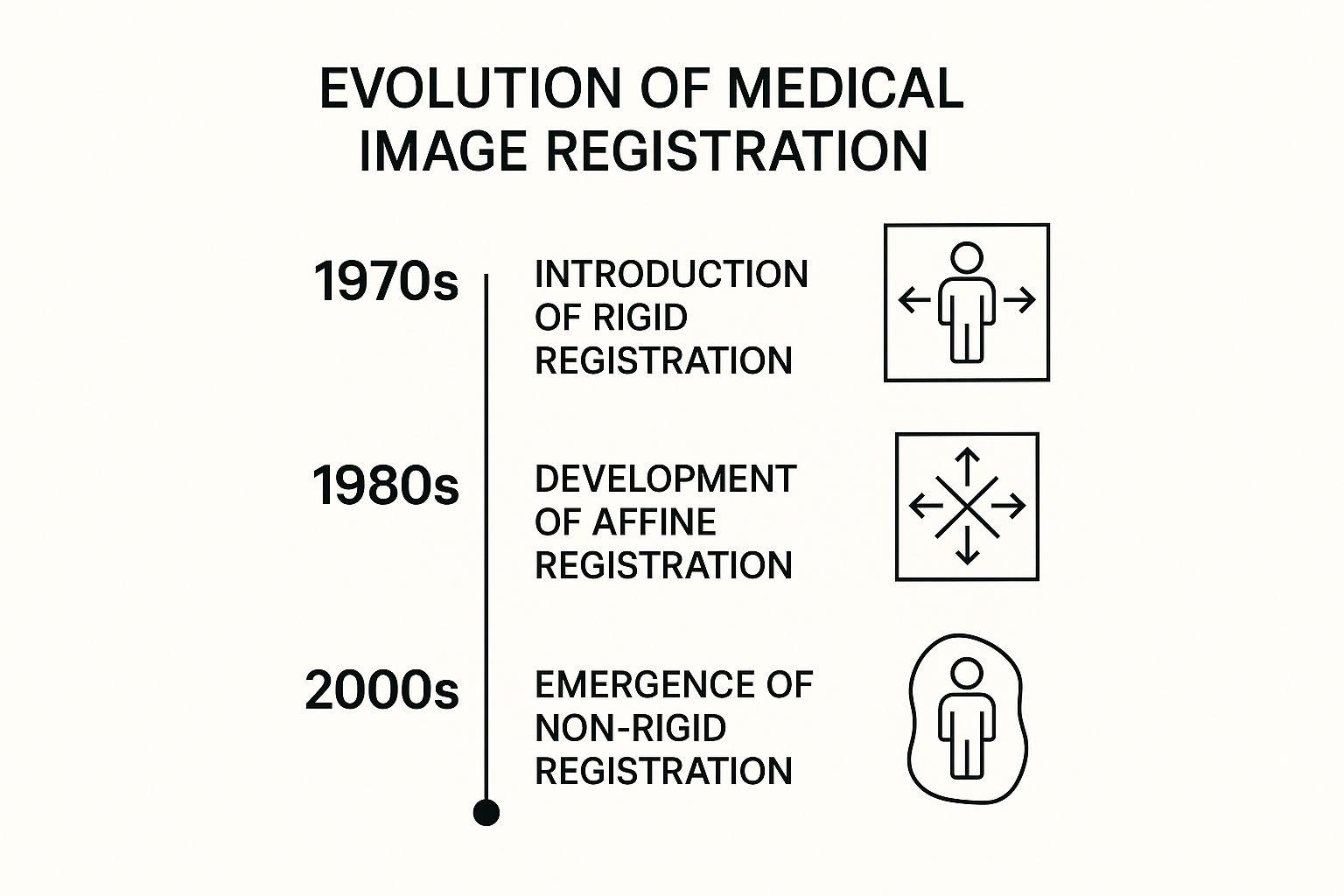
The infographic above illustrates key milestones in this journey, particularly the advancements in registration techniques. Beginning with rigid registration in the 1970s, where images were aligned using basic rotations and translations, the field advanced to affine registration in the 1980s. Affine registration incorporated scaling and shearing.
Finally, the arrival of non-rigid registration in the 2000s enabled more complex transformations. Non-rigid registration accommodates the deformable nature of soft tissues. This progress highlights the increasing sophistication and precision of medical image registration through the years.
Advancements in Multi-Modal and Cross-Modal Registration
Further progress in multi-modal and cross-modal registration has expanded the uses of this technology. Multi-modal registration combines images from the same modality acquired at different times or from various angles, such as monitoring tumor growth with several CT scans.
Cross-modal registration, conversely, integrates data from different imaging modalities, like aligning a CT scan with an MRI. This provides a more complete picture of a patient's anatomy and function. These developments have created opportunities for new clinical applications, leading to more informed diagnoses and treatment plans.
The Impact of Computational Power and Algorithms
The evolution of medical image registration has also been significantly shaped by the growth of computational power and development of advanced algorithms. Early registration methods were constrained by processing limitations, which restricted the complexity of possible transformations and the size of datasets.
With increased computing power, more complex and computationally demanding algorithms have become viable, ushering in more precise and efficient registration methods. These advancements have considerably improved both the speed and accuracy of medical image registration, facilitating real-time applications and enhancing clinical workflows.
Essential Registration Techniques That Actually Work
This section explores the core algorithms behind effective medical image registration in today's clinical settings. We'll examine several techniques, highlighting their strengths and practical uses. Our discussion will encompass how these methods operate, their ideal applications, and real-world examples of successful implementation.
Intensity-Based Registration
Intensity-based registration utilizes the pixel values within the images themselves. These methods analyze voxel intensity patterns to determine the optimal transformation for aligning two images. A common approach is mutual information, particularly well-suited for cross-modal registration. Mutual information measures the statistical relationship between the intensity distributions of the two images. This makes it robust when aligning images acquired from different modalities, such as CT and MRI scans, which possess inherently different contrast properties.
Feature-Based Registration
Rather than relying on raw pixel data, feature-based registration identifies specific anatomical landmarks. These landmarks serve as reference points, guiding the alignment procedure. This method proves valuable when distinct anatomical features are readily discernible, such as aligning bone structures in orthopedic imaging. Feature-based methods often involve the detection of edges, corners, or other prominent characteristics. The transformation is then calculated to precisely match these corresponding features.
Hybrid Registration Techniques
Capitalizing on the advantages of both methodologies, hybrid registration techniques combine intensity-based and feature-based approaches. This combination offers the potential for enhanced accuracy and reliability. By initially employing feature detection for a preliminary alignment, followed by refinement using intensity-based methods, these techniques can yield more precise outcomes. This approach is especially beneficial in cases where anatomical variations might pose challenges for techniques relying solely on intensity or features.
Iterative Optimization for Sub-Pixel Accuracy
Many registration techniques utilize iterative optimization algorithms. These algorithms progressively fine-tune the transformation, approaching optimal alignment with each iteration. This iterative process enables achieving sub-pixel accuracy, essential for clinical applications demanding precise alignment. Iterative methods often complement both intensity-based and feature-based strategies, further augmenting their precision. By iteratively adjusting the transformation, these methods accommodate subtle image discrepancies, ultimately achieving a more accurate and clinically relevant result. Selecting the most suitable method depends heavily on the specific clinical situation and the nature of the images being aligned.
The following table provides a concise comparison of these common medical image registration algorithms:
Comparison of Medical Image Registration Algorithms
| Algorithm Type | Primary Application | Accuracy Level | Processing Time | Best Use Cases |
|---|---|---|---|---|
| Intensity-based (e.g., Mutual Information) | Multi-modal image registration (e.g., CT and MRI) | Moderate to High | Moderate | Aligning images with varying contrast properties, soft tissue registration |
| Feature-based | Single modality image registration, bone structures | High for distinct features, lower for subtle features | Low to Moderate | Orthopedic imaging, aligning images with clear landmarks |
| Hybrid | Combining strengths of intensity-based and feature-based | High | Moderate to High | Cases with anatomical variations, complex registrations needing high accuracy |
This table summarizes the key characteristics of each algorithm type, assisting clinicians in choosing the best approach based on their specific needs. Factors such as the required accuracy, available processing time, and the types of images being registered all influence the decision-making process. Choosing the right technique is crucial for achieving optimal clinical outcomes in medical image analysis.
Real-World Clinical Applications That Transform Patient Care
Medical image registration has become essential in modern healthcare, significantly improving patient care across various medical specialties. This valuable technology empowers clinicians with improved diagnostic abilities and allows for more accurate treatment planning, leading to better patient outcomes.
Oncology: Precise Tumor Tracking and Personalized Therapy
In oncology, medical image registration is crucial for monitoring tumor development and its response to treatment. By precisely aligning images taken at different times, oncologists can accurately track tumor growth or shrinkage. This allows for adjustments to personalized therapy throughout the treatment process, contributing to more effective treatment strategies and increasing the chances of positive results.
Surgery: Multi-Modal Registration for Enhanced Surgical Planning
Surgical planning greatly benefits from medical image registration, especially multi-modal registration. Combining data from different imaging methods like CT scans and MRI scans gives surgeons a comprehensive view of the patient's anatomy. This detailed information allows for meticulous pre-operative planning, which can potentially minimize surgical complications and improve the precision of surgical procedures. For instance, registered images can help surgeons precisely locate critical anatomical structures, reducing the risk of damage during complex surgeries.
Cardiology: Temporal Registration for Assessing Heart Function
Temporal registration, which aligns images taken over a period, is crucial for evaluating heart function in cardiology. This technique enables cardiologists to monitor changes in heart wall motion and blood flow, providing valuable insights into the development of cardiovascular diseases. This information is essential for determining appropriate treatments and monitoring patient responses to therapy.
Quantifiable Benefits and Emerging Applications
The advantages of medical image registration are measurable and extensive. These include fewer diagnostic errors, increased treatment precision, and shorter procedure times. These improvements lead to more efficient healthcare delivery and better patient experiences. The positive impact of medical image registration on diagnostic and therapeutic outcomes is statistically significant. For example, studies show that accurate image registration can enhance the accuracy of tumor delineation in cancer treatment, reducing margins of error by up to 30%. More detailed statistics can be found here.
Beyond these established applications, medical image registration is constantly evolving, finding new uses in personalized medicine and large-scale population studies. As technology continues to advance, medical image registration is poised to play an even greater role in shaping the future of healthcare, offering exciting possibilities for further improvements in diagnosis, treatment, and patient care.
Mastering Multi-Modal Registration For Maximum Impact
Medical image registration truly shines when combining data from different imaging modalities. This approach, known as multi-modal registration, provides a more complete picture of a patient's condition than any single imaging technique. Leading medical centers increasingly integrate data from CT, MRI, PET, SPECT, and ultrasound to create thorough patient assessments. Medical image registration is also increasingly important in healthcare research. For example, AI agents like the one for Healthcare Medical Researcher are being developed to help push these advancements further.
Challenges of Cross-Modal Registration
Multi-modal registration presents some distinct difficulties. Each imaging technique relies on different physical principles, resulting in variations in image contrast, resolution, and anatomical representation. For instance, CT scans excel at visualizing bone structures, while MRI provides detailed soft tissue information. These inherent differences can make accurate alignment difficult if not addressed properly.
A CT scan might clearly show bone fractures, while an MRI of the same area reveals soft tissue damage surrounding the fracture. Combining this information demands sophisticated registration techniques that consider each modality's unique characteristics.
Advanced Techniques for Multi-Temporal Studies
Another vital application of medical image registration is in multi-temporal studies. These studies track changes over time, such as monitoring tumor growth or evaluating treatment response. Accurate alignment between images taken at different time points is essential for proper assessment.
This can be particularly challenging with soft tissues, which can deform over time. Advanced techniques that account for these deformations are crucial for precise tracking of changes.
Mutual Information and Normalized Cross-Correlation
Mutual information and normalized cross-correlation are two essential methods used in multi-modal registration. Mutual information measures the statistical dependence between the intensity distributions of two images. This allows for effective registration even when images have dramatically different contrast properties, which is crucial for fusing data from modalities like CT and MRI.
Normalized cross-correlation, on the other hand, measures the similarity between corresponding image regions based on their intensity patterns. These techniques, combined with advanced deformable registration algorithms, allow for the successful combination of complementary imaging data.
For example, aligning PET scans, which show metabolic activity, with CT scans, which provide anatomical detail, can pinpoint the exact location of metabolically active tumor regions. Institutions seeing strong results with multi-modal registration frequently employ these techniques alongside rigorous quality control measures to ensure accuracy and reliability. This integrated approach offers a wealth of diagnostic information unavailable from a single modality.
To further illustrate how multi-modal registration is applied across various medical specialties, the following table provides specific examples:
The table below details how different specialties use multi-modal registration to improve diagnoses and treatment planning.
| Medical Specialty | Primary Modalities | Registration Purpose | Clinical Benefits | Accuracy Requirements |
|---|---|---|---|---|
| Oncology | CT, PET, MRI | Tumor localization and treatment planning | Precise radiation therapy targeting, improved surgical planning | High (sub-millimeter) |
| Neurosurgery | MRI, CT, fMRI | Brain mapping and surgical guidance | Improved accuracy of surgical interventions, minimized damage to healthy tissue | High (sub-millimeter) |
| Cardiology | CT, Ultrasound, MRI | Cardiac function assessment and intervention planning | Accurate assessment of blood flow, improved placement of stents | Medium (1-2 millimeters) |
| Orthopedics | CT, MRI | Joint assessment and pre-operative planning | Precise implant sizing and placement, improved surgical outcomes | Medium (1-2 millimeters) |
| Radiation Oncology | CT, MRI, PET | Target delineation and dose calculation | Accurate delivery of radiation dose, minimized side effects | High (sub-millimeter) |
As this table demonstrates, multi-modal registration offers distinct advantages for various medical specialties, leading to more informed clinical decisions and improved patient care.
Practical Insights From Leading Institutions
Leading institutions in multi-modal registration emphasize the importance of strong validation and quality assurance protocols. They often create specialized workflows and training programs to guarantee consistent, high-quality registration across different operators and over time. These institutions frequently share best practices and contribute to developing standardized guidelines for multi-modal image registration, promoting the advancement and accessibility of this valuable technology.
Overcoming Implementation Challenges That Stop Most Teams

Implementing medical image registration in a clinical setting presents unique challenges. Successfully adopting this technology requires careful planning and execution. This section explores common hurdles and offers practical solutions based on real-world experience.
Computational Requirements and Workflow Integration
Medical image registration algorithms can be computationally demanding, especially when dealing with large datasets or intricate transformations. High-resolution 3D images, for instance, require significant processing power and memory. This necessitates investing in robust hardware and software infrastructure.
Integrating medical image registration into existing clinical workflows also presents complexities. It requires careful consideration of data management, image transfer protocols, and compatibility with current systems. A seamless integration is essential to minimize disruption to daily clinical routines.
Staff Training and Quality Assurance
Effective use of medical image registration relies heavily on proper staff training. Clinicians and technicians must be proficient in operating the software, interpreting the results, and troubleshooting any issues that may arise. Comprehensive training ensures the technology is used to its full potential.
Establishing robust quality assurance protocols is equally important. These protocols help ensure consistent registration accuracy and identify any errors. Regular quality checks are essential for validating results and minimizing variability between operators and over time.
Addressing Edge Cases and Managing Large-Scale Projects
Medical image registration algorithms can encounter challenging edge cases, such as images with artifacts or significant anatomical variations. Developing strategies to handle these scenarios is crucial for reliable and accurate results. This might involve specialized algorithms or manual intervention for particularly difficult cases.
Managing data and maintaining consistency in large-scale registration projects can be a significant undertaking. Efficient data management strategies and automated quality control procedures are vital for successful implementation when working with numerous images and users.
Budgetary Constraints and Stakeholder Buy-In
Budgetary limitations are often a major obstacle to implementation. Medical image registration can involve upfront costs for software, hardware, and staff training. Demonstrating the long-term benefits and return on investment is key to securing necessary funding and stakeholder support.
Building a compelling case for medical image registration requires highlighting its potential to improve diagnostic accuracy, reduce treatment errors, and optimize clinical workflows. Clearly communicating the benefits and implementation plan to stakeholders is crucial for fostering understanding and encouraging adoption.
Key Takeaways

Medical image registration has become a vital tool in modern healthcare, offering significant benefits across various medical specialties. This section highlights key insights for successful implementation and achieving lasting impact.
Understanding the Core Value
The primary value of medical image registration lies in its ability to combine data from multiple images. This allows clinicians to gain a more holistic view of a patient's anatomy and to monitor changes over time. This comprehensive understanding is critical for informed decision-making and improved patient care. For instance, image registration enables precise tumor tracking in oncology, leading to more targeted and effective treatment strategies.
Choosing the Right Technique
Selecting the appropriate registration technique is paramount. Intensity-based methods, such as mutual information, are well-suited for aligning images with varying contrast properties. These are commonly used in multi-modal image registration. Feature-based methods excel at aligning images with clearly defined anatomical landmarks, often used in orthopedic imaging. Hybrid techniques, combining the strengths of both approaches, offer increased accuracy in complex scenarios.
Implementing Effectively in Clinical Settings
Successful implementation depends on several factors. Addressing computational requirements and integrating the process seamlessly into existing workflows necessitate careful planning and investment in appropriate hardware and software. Comprehensive staff training is essential for maximizing the technology's potential and accurately interpreting the results. Implementing robust quality control protocols ensures reliability and consistency across all users. Overcoming these challenges often requires a well-defined strategy.
Ensuring Long-Term Success
Long-term success hinges on adapting to the ever-changing clinical landscape and integrating technological advancements. Regularly reviewing and updating registration protocols ensures alignment with best practices and maintains optimal performance.
Measuring and Demonstrating Value
Tracking key performance indicators (KPIs) showcases the tangible benefits of medical image registration to stakeholders. These metrics might include improved diagnostic accuracy, reduced procedure times, and enhanced patient outcomes. Clearly communicating these positive results reinforces the value of the investment and justifies continued use.
Specific Recommendations for Different Healthcare Settings
- Small Clinics: Concentrate on integrating user-friendly software with current systems and providing focused staff training.
- Large Medical Centers: Implement scalable solutions that can manage extensive datasets and complex workflows. Prioritize robust quality assurance procedures for consistency across various departments.
By addressing these key takeaways, healthcare providers can effectively implement and leverage medical image registration to improve patient care and elevate clinical outcomes. PYCAD offers advanced AI-driven solutions for medical image registration, empowering healthcare providers to overcome implementation obstacles and unlock the full potential of this valuable technology. Visit PYCAD to learn how their specialized knowledge can enhance your medical imaging capabilities.






