Analysis imaging software isn't just another image viewer. Think of it more like a high-powered digital microscope for medical scans, turning the complex visual data from MRIs, CT scans, and X-rays into precise, measurable, and actionable insights. It’s the tool that bridges the gap between subjective observation and truly objective, data-driven diagnostics.
Decoding the Digital Detective
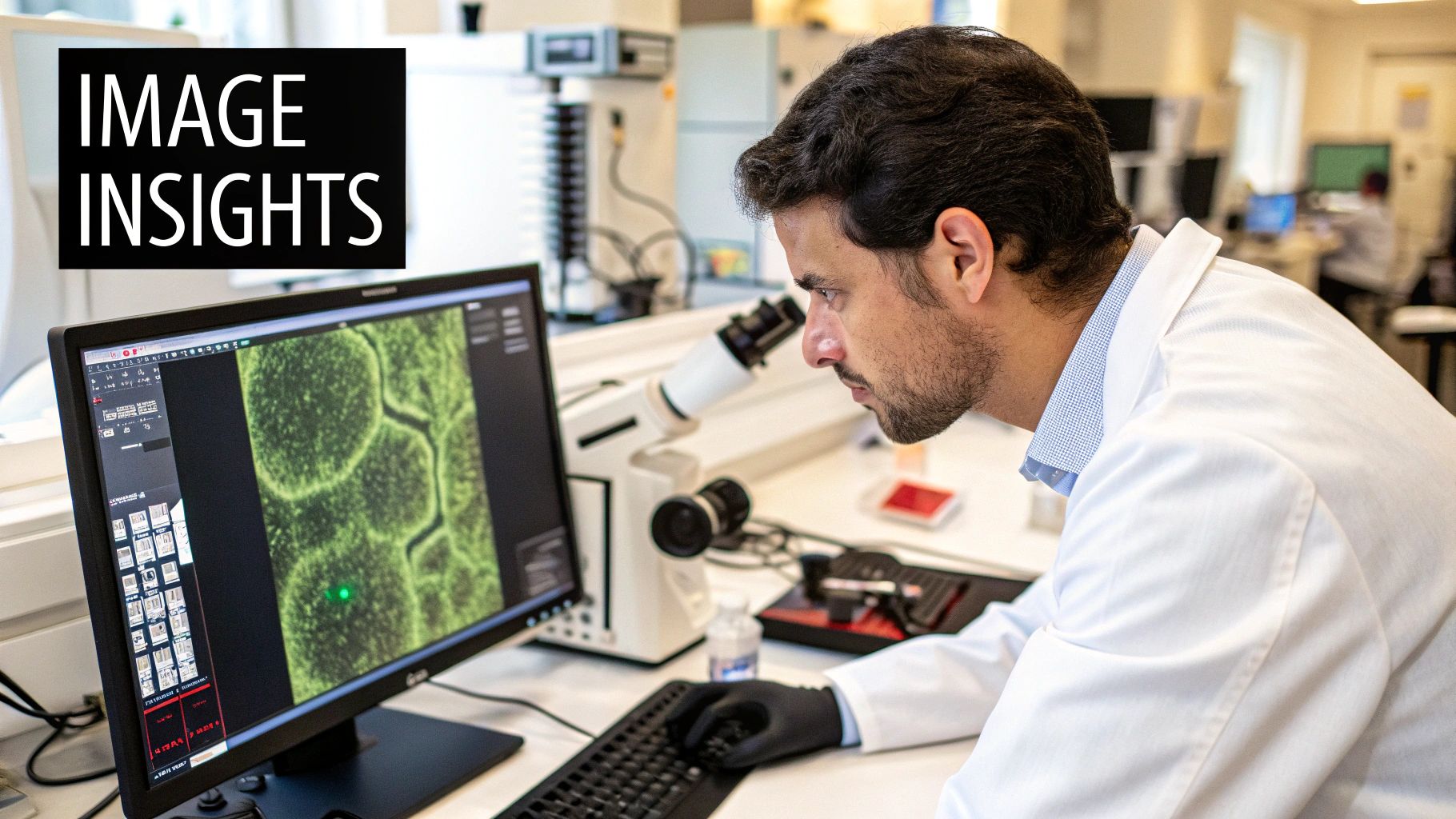
Picture a radiologist studying a brain MRI. With a trained eye, they can certainly spot an anomaly. But measuring the exact volume of a tumor or quantifying subtle shifts in tissue density over time? That’s an entirely different challenge. This is precisely where analysis imaging software comes in, acting like a brilliant detective's toolkit.
Instead of simply showing a static picture, the software gets to work, meticulously examining every single pixel. It can digitally trace the exact boundaries of a tumor, calculate its volume with millimeter accuracy, and even build a 3D model of its structure. This isn't just about seeing the image; it's about interrogating it to uncover every last piece of hidden data.
From Pixels to Clinical Insights
At its heart, the purpose of this software is to convert qualitative images into quantitative data. It arms clinicians with objective numbers and metrics that bolster their diagnostic reasoning, effectively taking the guesswork out of incredibly complex assessments. That shift is absolutely critical for modern medicine.
A few key functions make this possible:
- Segmentation: This involves automatically or semi-automatically outlining specific structures—like an organ or a lesion—to isolate them for a closer look.
- Quantification: Here, the software measures specific properties such as size, shape, density, or blood flow, assigning real numerical values to them.
- Registration: This powerful feature aligns multiple scans taken at different times, allowing doctors to precisely track changes and see if a treatment is working.
This data-first approach is pushing healthcare forward in a big way. The demand is reflected in market growth; one report shows the medical imaging and radiology software market jumped from $7.35 billion in 2024 to $8 billion in 2025. Even more telling, it’s projected to top $11 billion by 2029, largely because of the push toward precision medicine and the universal adoption of digital imaging. You can read the full medical imaging software market report for a deeper dive.
By turning images into hard data, analysis imaging software provides a common, objective language for clinicians to discuss patient cases, plan treatments, and monitor progress with unparalleled confidence and accuracy.
A Digital Assistant for Clinicians
In a way, you can think of this software as a tireless digital assistant. It handles the laborious and time-consuming work of detailed measurement and comparison, which in turn frees up experts to focus on what they do best: high-level interpretation and patient care. The software highlights suspicious areas, tracks changes between scans, and presents its findings in a clear, organized report.
This kind of support is invaluable in fields like oncology, neurology, and cardiology, where even the smallest changes can carry massive clinical weight. By automating these analytical tasks, the software doesn't just make the process faster—it also makes diagnoses more consistent and reliable across the board.
Unpacking The Core Capabilities
To really get what makes analysis imaging software so powerful, you have to look past the basic definition and see what it actually does. These aren't just fancy picture viewers; they're powerful analytical tools built to pull real, measurable data out of complex medical scans. Think of each feature as a highly specialized instrument, giving doctors a much deeper view than they could ever get with the naked eye.
These core functions are the bedrock of modern diagnostics. They give healthcare professionals the power to make critical decisions based on precise data, not just visual guesswork. This move from a "what it looks like" assessment to a "what it measures" approach is a game-changer for improving patient outcomes.
The diagram below breaks down the main categories these features fall into, showing how they all click together within the software.
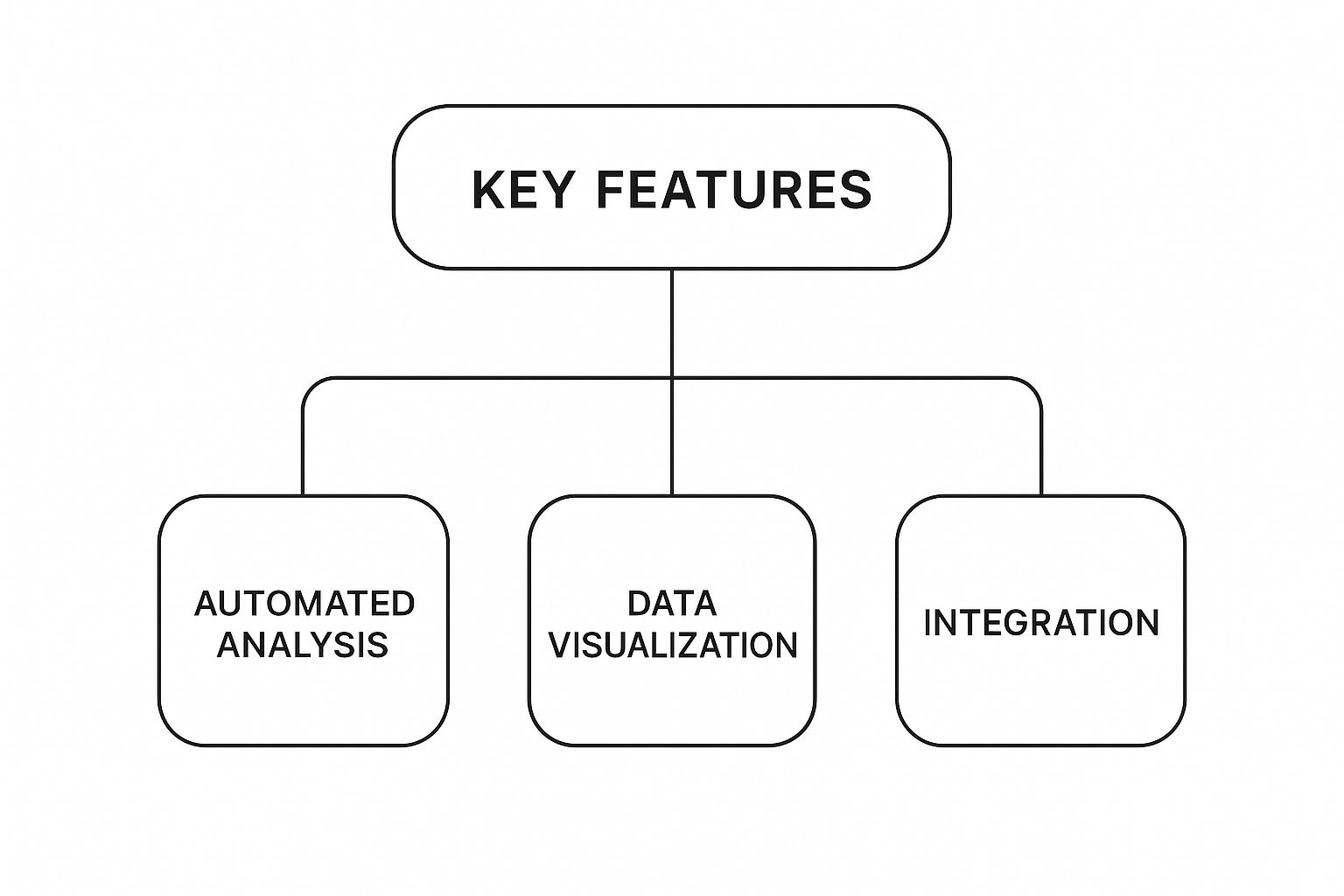
As you can see, the real magic happens when automated analysis and advanced visualization are combined, all while fitting neatly into the hospital's existing workflow.
Image Segmentation: Digital Precision
One of the most fundamental features is image segmentation. The best way to picture this is as a digital scalpel with incredible precision. The software can carefully trace the exact outline of an organ, a tumor in the liver, or a lesion in the brain, separating it perfectly from all the surrounding tissue.
This is absolutely essential for getting accurate measurements. Once an object is "segmented" or isolated, the software can calculate its volume, shape, and density with a level of detail that’s impossible to do by hand. This completely removes the guesswork of manual outlining, making every measurement objective and repeatable.
3D Modeling: Visualizing For Surgery
This software can also take a whole stack of 2D scan slices—like from a CT or MRI—and stitch them together into a fully interactive 3D model. It’s like creating a detailed, digital replica of the patient's internal anatomy. Surgeons can spin this model around, look at it from any angle, and even do a virtual "fly-through" to get a feel for the complex spatial relationships inside the body.
This is an indispensable tool for planning surgeries. For example, a neurosurgeon can map out the safest route to remove a brain tumor, identifying and plotting a path around critical blood vessels long before the patient is even in the operating room. This kind of detailed prep work can dramatically reduce surgical risks and lead to much better results.
To give you a better idea of these capabilities, here’s a quick breakdown of the key features you’ll find in most analysis imaging platforms.
Key Features of Analysis Imaging Software
| Feature | Description | Clinical Application Example |
|---|---|---|
| Image Segmentation | Automatically or semi-automatically outlines anatomical structures, lesions, or tumors. | Isolating a cancerous tumor from healthy liver tissue to calculate its exact volume. |
| 3D Modeling & Visualization | Reconstructs 2D scan slices into interactive 3D models. | Creating a 3D model of a patient's heart to plan a complex valve replacement surgery. |
| Quantitative Analysis | Extracts objective numerical data (e.g., volume, density, blood flow) from images. | Measuring a 15% reduction in tumor size after a course of chemotherapy. |
| Longitudinal Tracking | Aligns and compares scans taken at different times to track changes. | Overlaying two brain MRIs taken a year apart to monitor the progression of multiple sclerosis. |
Each of these features works together to paint a far more complete and accurate picture of a patient's condition, moving diagnostics from an art to a data-driven science.
Quantitative Analysis: The Power Of Numbers
Maybe the most significant capability is quantitative analysis. This is where the software translates visual information into cold, hard data. Instead of a radiologist describing a tumor as just "larger," the software can report a precise volumetric increase of 15%. Gaining a wider perspective on data analysis services can clarify the foundational tech that drives these imaging solutions; you can explore offerings like Datagrove's data services for more context.
This is used in countless ways across medicine:
- Oncology: Tracking tumor volume to get an objective read on how well chemotherapy is working.
- Cardiology: Calculating the speed of blood flow in an artery to diagnose a blockage.
- Neurology: Measuring the rate of brain tissue loss in patients with Alzheimer's disease.
These numbers provide a solid, evidence-based launching point for making crucial clinical decisions.
The ability to assign concrete numbers to visual observations is the core strength of analysis imaging software. It replaces subjective interpretation with objective, actionable data, leading to more consistent and reliable diagnoses.
Longitudinal Tracking: Monitoring Change Over Time
Finally, longitudinal tracking is what allows clinicians to compare scans taken over weeks, months, or even years with perfect alignment. The software stacks new scans right on top of old ones, automatically highlighting even tiny changes that would be impossible for a person to spot. This is critical for keeping an eye on chronic diseases or checking if a long-term treatment is doing its job.
By precisely tracking how a disease is progressing or regressing, doctors can make proactive adjustments to treatment plans. It ensures every patient gets the most effective care exactly when they need it. This feature essentially turns a series of static snapshots into a dynamic story of a patient's health journey.
How AI Is Giving Image Analysis a Major Upgrade
Think of Artificial Intelligence (AI) as a powerful supercharger for modern analysis imaging software. It takes standard image processing and turns it into a dynamic, predictive tool that can see things far beyond the limits of human observation. AI algorithms are trained on huge datasets—we're talking millions of medical images—which teaches them to recognize patterns, anomalies, and subtle signs of disease that could easily be missed.
This isn't just about making things faster; it's about completely changing how diagnostic work gets done. Imagine an AI-powered system as a highly trained assistant working right alongside a radiologist. This "assistant" can pre-analyze hundreds of scans, instantly flag potential areas of concern, and prioritize the most critical cases so a doctor can review them immediately.
Automating Anomaly Detection
One of the biggest game-changers AI brings to the table is its ability to automate anomaly detection. Instead of a clinician having to manually scrutinize every single pixel of a scan, an AI model can do it in seconds. It learns what "normal" tissue is supposed to look like and can instantly highlight any deviation, whether it's a tiny lung nodule on a CT scan or an unusual cell structure on a digital pathology slide.
This capability is a huge help in easing the massive workload healthcare professionals face. It provides a consistent, vigilant first look at every image, acting as an essential safety net.
The real value of AI here is its tireless precision. It can perform repetitive, detail-oriented tasks without ever getting tired, freeing up expert clinicians to focus their skills on what really matters: complex diagnoses, treatment planning, and talking with patients.
This move toward automation isn't just a nice idea; it's driving serious market growth. The medical imaging software market, which was valued at around USD 3.5 billion in 2024, is expected to jump to USD 7.5 billion by 2034. This explosive growth is almost entirely fueled by AI's power to make diagnoses more accurate and faster, a critical need as chronic diseases become more common around the world. You can find more details about this trend in this report on the growth of the medical imaging software market.
The image below shows how AI tools are being woven into different areas of healthcare, from diagnosis to treatment.
As you can see, medical imaging is right at the center of it all, with AI adding real value at every step, from the first detection to long-term patient monitoring.
Shifting from Reactive to Predictive Analysis
AI is doing more than just finding existing problems; it's pushing analysis imaging software into the world of predictive medicine. By analyzing imaging data along with other patient information—like genetics and clinical history—AI models are starting to forecast the risk and progression of diseases.
Picture an algorithm that analyzes a routine brain MRI and spots subtle structural changes. While these changes might not be causing symptoms yet, they could correlate with a high risk of developing Alzheimer's disease down the road. This gives doctors a chance to step in much earlier than was ever possible before.
Some key predictive capabilities include:
- Risk Stratification: AI can sort patients into high, medium, or low-risk groups for certain conditions based on their scans, which helps doctors prioritize preventative care.
- Treatment Response Prediction: By comparing a tumor's features to those in its vast training data, AI can help predict how it might respond to different therapies, opening the door for truly personalized treatment plans.
- Outcome Forecasting: Some advanced models can even look at post-operative scans to predict a patient's recovery path or the likelihood of a disease coming back.
The Brains Behind the Operation: Machine Learning and Deep Learning
The engine making all of this happen is machine learning (ML), a field of AI where systems learn directly from data. For image analysis, the most powerful tool in the ML toolkit is deep learning, which uses complex neural networks designed to mimic the human brain. These networks are exceptionally good at visual recognition.
Here’s a simple look at how it works:
- Training Data: A deep learning model is "fed" millions of labeled medical images (e.g., "this image shows a malignant tumor," "this one is benign").
- Pattern Recognition: The model teaches itself to identify the incredibly complex features and textures associated with different diagnoses.
- Inference: Once trained, it can apply that knowledge to brand-new images it has never seen before, making highly accurate classifications or predictions in real time.
This is the process that allows AI to spot a hairline fracture on an X-ray that a person might miss or tell the difference between benign and malignant lesions with stunning accuracy. It's this integration of sophisticated algorithms that makes modern analysis imaging software an indispensable part of advanced medical care, directly leading to better patient outcomes by making diagnostics faster, more precise, and increasingly predictive.
Real-World Applications in Modern Medicine
The true power of analysis imaging software isn't in its list of features; it's what happens when those tools get into the hands of clinicians in real, everyday medical settings. It’s one thing to read about the technology, but it’s another to see it solve concrete problems and genuinely improve patient lives. This isn’t just some background utility—it's an active partner in diagnosis and treatment across a huge range of specialties, bringing clarity where there was once only uncertainty.
Whether we're talking about fighting cancer or protecting brain health, these applications show a fundamental shift toward data-driven medicine. Each use case is a story of a tough clinical challenge being met with a smart technological solution, ultimately leading to a better patient outcome.
Let's dive into a few of these scenarios.
Precision in Oncology
In oncology, the battle against cancer is often a game of millimeters. A doctor needs to know, with total confidence, if a tumor is shrinking, growing, or holding steady after months of chemotherapy. Just relying on the human eye to compare two CT scans taken weeks apart is incredibly challenging. Subtle changes are just too easy to miss.
This is exactly where analysis imaging software shines. Using longitudinal tracking, the software can overlay a new scan directly on top of an old one, aligning them perfectly. It then automatically maps out the tumor's exact boundaries in both images and calculates its volume down to the cubic millimeter.
So, instead of a subjective guess like "it looks a little smaller," the oncologist gets a hard number: "The tumor has decreased in volume by 18%." That objective data gives them the confidence to stick with a winning treatment or quickly pivot to a new strategy, personalizing care when it matters most.
Clarity in Cardiology
Cardiovascular health is all about the dynamic movement of the heart and blood. A common hurdle is diagnosing coronary artery disease, where plaque narrows the arteries and chokes off blood flow. In the past, this often meant an invasive procedure like an angiogram. Now, software offers a powerful non-invasive alternative.
Using images from a standard cardiac CT scan, the software can build a stunningly detailed 3D model of the heart and coronary arteries. From there, it can run a quantitative analysis to measure the exact percentage of a blockage in a specific vessel or even simulate how blood flows through it.
A cardiologist can see a precise map of arterial blockages and calculate key metrics like ejection fraction—the amount of blood the heart pumps with each beat—all without making a single incision. This gives them a complete picture of cardiac function, allowing them to plan interventions like stenting with incredible accuracy.
By turning static images into dynamic, functional models, the software gives cardiologists the insights they need to diagnose complex conditions and plan treatments with far less risk to the patient.
Insight in Neurology
Neurological conditions can be frustratingly slow and subtle, which makes them notoriously difficult to track over time. For diseases like multiple sclerosis (MS) or Alzheimer's, clinicians need a way to measure changes in the brain that are almost invisible from one year to the next.
Take an MS patient. The disease is defined by lesions forming in the brain and spinal cord. An analysis platform can take an MRI scan and automatically detect, map out, and count every single lesion. Even better, when a follow-up scan is done a year later, the software can compare the two and flag not only new lesions but also any tiny change in the size of existing ones.
This provides an unbiased, objective measure of disease progression. For someone with Alzheimer's, the software can do something similar by precisely measuring the volume of the hippocampus—a key brain region hit hard by the disease—and tracking its rate of shrinkage over several years. This data is absolutely critical for staging the disease and seeing if new therapies are actually working.
For more practical case studies and a closer look at how imaging software is being used, you might want to explore Salthea's Blog for further insights. These real-world examples really drive home the impact these advanced tools are having on the front lines of medicine.
How to Choose the Right Imaging Software
Picking the right analysis imaging software is a huge decision. It’s less like buying a new gadget and more like hiring a key member of your team. The wrong choice can lead to data bottlenecks and frustrated clinicians. But the right one? It can feel like a natural extension of your diagnostic process, boosting efficiency and ultimately leading to better patient care.
To get it right, you need a solid game plan. This isn't just about ticking boxes on a feature list. It's about figuring out how a new tool will fit into your existing world. After all, even the most advanced software is worthless if it can't talk to the systems you already rely on every day.

This decision sets the stage not just for today, but for how you’ll handle medical imaging and data for years to come.
Evaluate Interoperability and Integration
First things first: interoperability. This is the absolute make-or-break factor. The software you choose must connect seamlessly with your core infrastructure, especially your Picture Archiving and Communication System (PACS) and Electronic Health Records (EHR). This connection is what allows patient information to flow smoothly from one point to the next.
Without it, your team is stuck with clumsy workarounds like manually exporting and re-uploading data. Not only does this waste precious time, but it’s a recipe for human error. Real integration means a radiologist can open the analysis tool directly from a patient’s file and have the finished report automatically save right back into the EHR. No extra steps, no friction.
When you’re talking to vendors, push for a live demonstration showing how their software works with your specific PACS and EHR systems. Vague promises won't cut it—you need to see proof of a smooth, two-way street for your data. This single point will have the biggest day-to-day impact on your team.
Prioritize Regulatory Compliance and Security
In the world of healthcare, compliance isn't optional. Any analysis imaging software you even consider has to meet tough industry standards for patient safety and data privacy. This is a baseline requirement that should immediately filter out any subpar options.
Here are the key checkpoints to look for:
- FDA Clearance: For any tool used for clinical diagnosis in the U.S., this is often a must-have. It's the seal of approval that the software is safe and does what it claims to do.
- HIPAA Compliance: The software needs ironclad security to protect patient data. Think data encryption, strict access controls, and detailed logs of who accessed what and when.
- CE Marking: This is the European equivalent of FDA clearance, required for software sold in the European Economic Area.
A vendor’s dedication to meeting regulatory standards says a lot about their commitment to quality and patient safety. Always ask for documentation and verify these credentials yourself.
Standalone Specialty Platforms vs. Integrated Solutions
One of the biggest forks in the road is deciding between a standalone, specialized platform and a broader solution that's integrated into a larger suite. Standalone software often goes incredibly deep into one specific area, like cardiology or neurology. An integrated solution, on the other hand, provides a wider range of tools for multiple departments, all under one roof.
This choice is at the heart of a major market shift. By 2025, the global medical image analysis software market is expected to hit around USD 4.26 billion. Digging into those numbers, you can see a clear trend: standalone products are predicted to shrink to 37% of the market, while integrated solutions climb to 42%. For a closer look at these numbers, you can find more medical image analysis software statistics that highlight this move toward comprehensive platforms.
Deciding between a standalone or integrated solution really comes down to your organization's unique needs. To help clarify this choice, think about how each approach stacks up against your priorities.
Software Selection Checklist: Standalone vs. Integrated
| Evaluation Criteria | Standalone Software | Integrated Solution |
|---|---|---|
| Specialization | Deep, best-in-class features for a specific discipline (e.g., oncology). | Broader, generalist tools that cover multiple departments. |
| Workflow | May require separate logins and data transfers, creating potential friction. | Offers a unified user experience within a single ecosystem (e.g., PACS). |
| Vendor Management | Involves managing multiple vendor relationships and contracts. | Simplifies procurement and support with a single point of contact. |
| Implementation | Can be faster to deploy for a single department's specific needs. | Often a larger, more complex implementation project across the organization. |
| Cost | Potentially lower initial cost, but costs can add up with multiple systems. | Higher upfront investment but may offer better long-term value and TCO. |
| Innovation | Often more agile and quicker to adopt the latest niche-specific advancements. | Innovation pace might be slower but offers stability and broad compatibility. |
Ultimately, a specialized cancer research center might get the most out of a top-tier standalone oncology platform. A large general hospital, however, would likely find more value in an integrated system that serves everyone from radiology to orthopedics. Weigh your daily workflows, budget, and future goals to find the right fit.
Getting From Installation to True Clinical Adoption
Putting a new analysis imaging software platform in place is much more than just an IT rollout. It's a fundamental change to the clinical workflow, and getting it right means focusing as much on the people as on the technology. Simply flipping the switch on the software doesn't guarantee success; real adoption happens when your clinical team feels comfortable, supported, and genuinely helped by the new tools.
The first step is always anticipating the technical speed bumps. You're almost guaranteed to run into challenges when trying to connect a modern platform with older infrastructure, like a legacy PACS or an established EHR system. It's critical to have a solid plan for migrating data and ensuring the new software talks to the old systems without a hitch. If you don't get this right from the start, you'll create frustrating data silos and workflow headaches that can poison the well for your staff.
Building Confidence and Getting People On Board
Let's be honest: the biggest hurdle is rarely the technology itself. It's getting your team to embrace a new way of working. Clinicians, like all of us, get into routines. Any disruption to how they've always done things will naturally be met with a healthy dose of skepticism. This is where a fantastic training program becomes your most important tool.
One of the best ways to do this is with a 'train-the-trainer' approach. Find a few tech-savvy, respected "super-users" in each department and give them deep, hands-on training. These individuals become your internal champions. They can offer shoulder-to-shoulder support to their colleagues, which often feels more approachable and relevant than help from an outside vendor.
Implementation isn't finished when the software is installed. It's finished when clinicians are using it effortlessly to make better decisions for their patients. Success is measured by clinical impact, not by checking off boxes on an IT project plan.
A Step-by-Step Rollout Beats the "Big Bang" Approach
Trying to launch a new system across an entire organization all at once is a recipe for chaos. A phased rollout is a much smarter, calmer way to manage the change. By starting small, you can learn as you go and build momentum.
Think of it as a simple, four-step process:
- Run a Pilot Program: Pick a single, enthusiastic department to be your test site. This is your chance to gather real-world feedback on everything from the user interface to how it fits into their day-to-day work.
- Share the Wins: Once the pilot group starts seeing results—maybe they're diagnosing certain conditions faster or with more confidence—shout it from the rooftops! Sharing these specific success stories gets other departments excited about what's coming.
- Tweak and Improve: Use the feedback from the pilot to iron out any wrinkles in your training materials and your overall implementation plan.
- Expand Incrementally: Now, you can start rolling the software out to other departments. Your original super-users can act as mentors and guides for the new teams, making the transition feel much smoother.
This methodical strategy turns a massive, intimidating project into a series of manageable wins. It ensures your new analysis imaging software ends up being a powerful tool that people rely on, not another piece of technology that just gets in the way.
Frequently Asked Questions
When you start digging into analysis imaging software, a lot of practical questions pop up. How does it actually fit with the systems you already have? What's the learning curve like for the team? Let's clear up some of the most common questions.
Think of this as the quick, straightforward guide to understanding where these powerful tools fit and the value they bring to a modern clinic.
How Is This Different from a PACS System?
This is a great question, and the distinction is critical. Your Picture Archiving and Communication System (PACS) is essentially your digital filing cabinet. Its main job is to safely store and retrieve medical images, making them available wherever they're needed. It’s the library.
Analysis imaging software, on the other hand, is the set of specialized tools you use to actually work with the images. It's what lets you perform complex tasks like segmentation, build 3D models, or run quantitative analysis. A PACS lets you see the image; this software lets you measure it, track changes over time, and pull out clinical data that isn't visible at first glance.
Think of it this way: A PACS is the vault where you store your blueprints. The analysis software is the set of advanced engineering tools you use to interpret those blueprints and make critical decisions.
What Kind of Training Is Needed for Staff?
While most modern imaging software is designed to be intuitive, you can't just hand it over and expect everyone to get the most out of it. Good training is key. Most of the time, getting a team up to speed involves a few smart steps.
- Vendor-Led Kick-Off: The software company usually provides the initial, in-depth training for a core group of "super-users" or department leads.
- Peer-to-Peer Champions: These newly trained experts become your internal go-to people. They can offer day-to-day help to their colleagues, which often feels more approachable.
- Continuous Learning: The best vendors also offer a wealth of resources like online tutorials, webinars, and detailed guides for ongoing support and for when new features are released.
The goal isn't just about learning which buttons to press. It’s about building the clinical confidence to use the software’s features to solve real-world diagnostic problems.
Can This Software Truly Reduce Diagnostic Errors?
Yes, absolutely. This is one of its biggest strengths. The software provides objective, quantitative data, which helps cut down on the subjective interpretation that can sometimes lead to human error. For instance, it can precisely measure a tumor's change in volume between two scans—a subtle shift that might be missed by the human eye.
AI-driven features take this a step further by automatically flagging areas of potential concern, drawing a radiologist's attention to something that needs a closer look. It’s like having a second set of tireless, highly-trained eyes on every scan. The software doesn't replace the expert's judgment; it arms them with better data to make a more confident final call.
Ready to bring intelligent, data-driven analysis into your medical imaging workflow? PYCAD specializes in developing and deploying custom AI solutions that sharpen diagnostic accuracy and streamline operations. See how our expertise can advance your technology at https://pycad.co.






