For decades, radiologists have faced a monumental task: meticulously poring over countless medical images, searching for tiny, almost imperceptible signs of disease. Think of it like trying to find a single specific sentence hidden within an enormous library. It's a job that demands incredible focus and, frankly, a lot of time.
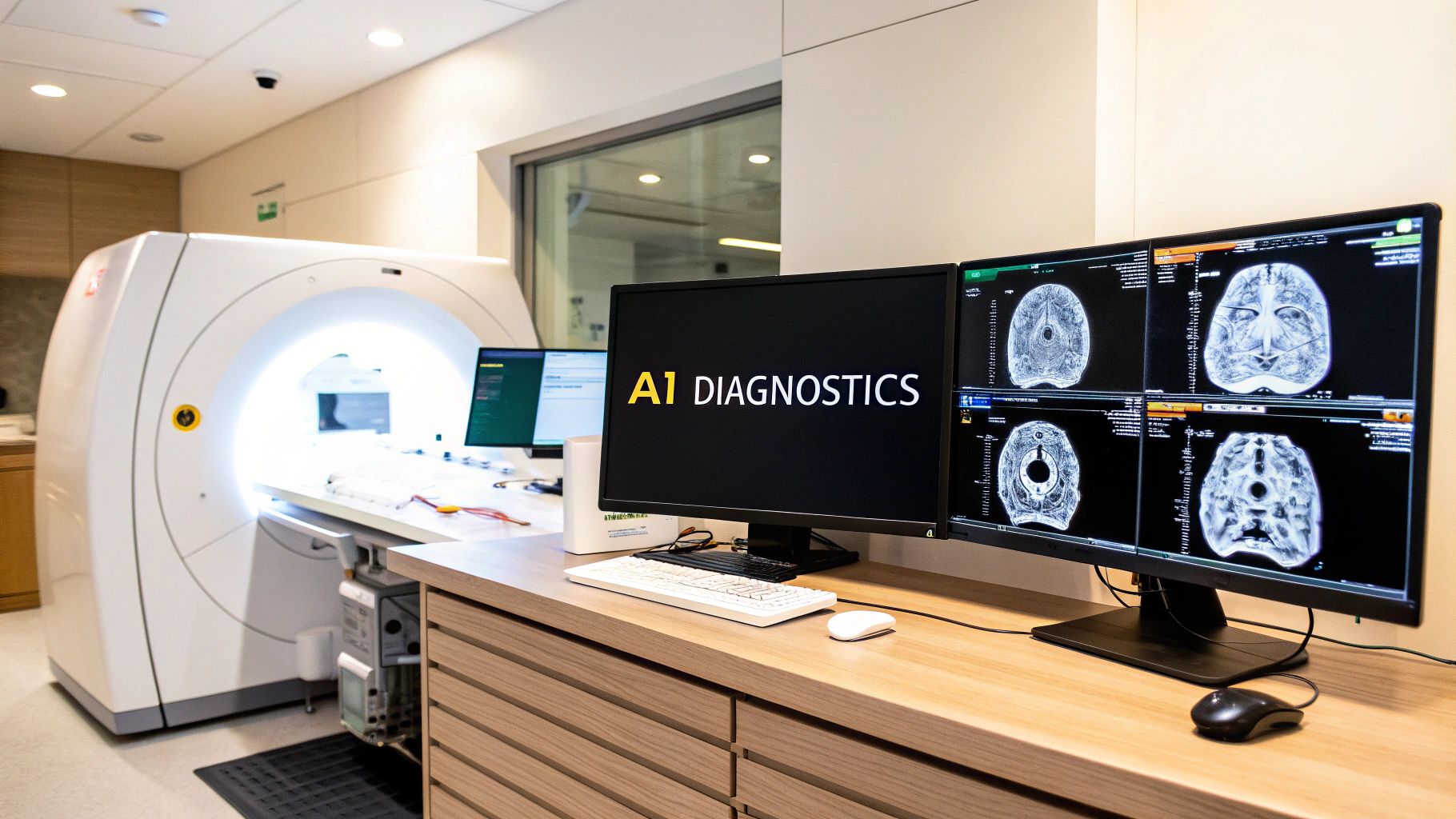
AI radiology software has emerged as a powerful new partner in this effort. It's not a replacement for the radiologist's expertise. Instead, think of it as an intelligent assistant that instantly finds the right book, highlights the exact sentence you're looking for, and even pulls up related texts for crucial context.
The New Partner in Medical Imaging

This technology is becoming an essential tool for tackling the sheer volume of medical images modern healthcare generates. It uses advanced algorithms trained on millions of scans to spot subtle patterns, automate tedious measurements, and flag urgent cases that need immediate attention. At its core, it's about augmenting a radiologist's skills, not making them obsolete.
Enhancing Diagnostic Confidence and Efficiency
The software essentially provides a second set of digital eyes, scanning every pixel for potential issues. These are often things that could be easily missed during a long, demanding shift. AI excels at the repetitive, objective tasks, which frees up clinicians to concentrate on what humans do best—handling complex patient cases, making nuanced diagnostic calls, and planning treatments with the care team.
For instance, an AI can automatically measure a tumor’s dimensions or calculate blood flow in seconds, tasks that would otherwise eat up precious minutes. This kind of automation streamlines the entire diagnostic process from start to finish.
A key thing to remember is that these tools support clinical judgment; they don't replace it. When an AI flags a potential nodule on a lung scan, it’s not making the diagnosis. It’s prompting the radiologist to take a closer look and use their deep medical knowledge to answer the critical question: "Does this finding make sense given the patient's history and other clinical data?"
This collaborative dynamic ultimately builds greater diagnostic confidence and helps reduce the immense cognitive load on specialists. The goal is straightforward:
- Boost Accuracy: Pinpoint hard-to-detect abnormalities and cut down on diagnostic errors.
- Increase Speed: Drastically reduce image interpretation and report turnaround times, which is especially vital in emergencies.
- Improve Workflow: Automate routine work so radiologists can focus their expertise where it matters most.
To give you a clearer picture, here’s a quick breakdown of what these systems are designed to do.
Core Functions of AI in Radiology at a Glance
This table summarizes the primary capabilities of AI radiology software, providing a quick reference for its key applications in a clinical setting.
| Function Area | Description | Primary Benefit |
|---|---|---|
| Anomaly Detection | Identifies and highlights suspicious regions or abnormalities on medical scans (e.g., nodules, fractures, bleeds). | Acts as a second reader, reducing the risk of missed findings and improving diagnostic accuracy. |
| Workflow Triage | Automatically prioritizes scans based on the urgency of potential findings (e.g., flagging a brain bleed for immediate review). | Ensures critical cases are addressed first, significantly shortening time-to-diagnosis in emergencies. |
| Image Quantification | Measures and quantifies anatomical structures or disease progression (e.g., tumor size, organ volume). | Automates time-consuming tasks, provides objective data for tracking treatment response, and improves consistency. |
| Image Segmentation | Outlines specific organs or abnormalities, separating them from surrounding tissue. | Provides precise anatomical context, which is crucial for surgical planning and radiation therapy. |
These functions work together to create a more efficient and effective radiology department.
A Foundation for Modern Healthcare
As we dive deeper into the world of AI in radiology, we'll move from these foundational ideas to real-world examples. You’ll get a solid grasp of the core problems this software solves—from managing overwhelming data loads to helping prevent radiologist burnout. We'll look at the technology behind it, celebrate some clinical success stories, and offer a practical guide for how to evaluate and bring these powerful tools into a clinical setting. This isn't just a futuristic idea; it's a real-world partner helping to deliver better patient care right now.
How AI Radiology Software Learns to See
The idea of artificial intelligence "seeing" a medical image can feel a bit like magic, but the reality is much more grounded. Think of it like training a new medical resident, not casting a spell. A resident learns by poring over thousands of cases under the guidance of an experienced attending physician; in the same way, an AI radiology software algorithm learns by analyzing vast, anonymized datasets of medical scans.
This entire process is powered by machine learning, a fascinating field of AI where systems get smarter through experience, not by being hand-fed a set of rigid instructions. You don’t tell the software, "If you see a bright white spot here, it’s a fracture." Instead, you show it countless examples of scans—some with fractures, some without—and it gradually starts to recognize the incredibly subtle patterns, textures, and shapes that signal a specific diagnosis.
To really get how AI interprets these images, you need to understand the basics of computer vision, which is the science of teaching machines how to see and process visual information from the world.
The Training Ground for AI Models
The fuel for any high-performing AI radiology software is data—and a lot of it. An algorithm's skill at spotting a tiny lung nodule or mapping a complex brain tumor is directly tied to the quality and volume of the images it learned from. This training is a multi-step process.
- Data Curation: First, a massive and diverse library of anonymized images (CTs, MRIs, X-rays) is gathered. Diversity is key here. The dataset needs images from different machines, patient demographics, and disease stages to prevent the AI from developing blind spots or biases.
- Expert Annotation: This is where human expertise is absolutely critical. Radiologists meticulously go through these images and "label" them. They might draw a precise box around a tumor, trace the outline of an organ, or classify a fracture type. This labeling creates the “ground truth”—the correct answer that the AI will learn from.
- Model Training: The AI model, often a type of neural network, then processes these labeled images over and over again. With each pass, it makes a prediction, compares that prediction to the radiologist's ground truth, and adjusts its internal programming to get closer to the right answer.
It's a bit like a high-stakes flashcard quiz. The AI sees an image (the card), makes a guess ("fracture!"), and then gets instant feedback (the correct answer on the back). After running through millions of these "flashcards," it becomes incredibly skilled at getting the answer right all on its own.
This constant cycle of trial and error is what allows the AI to pick up on nuances that can be tough for the human eye to spot consistently, especially when facing a heavy workload. The software isn't just memorizing pictures; it's learning the fundamental visual markers of specific medical conditions.
This visualization shows how all that training effort pays off in the clinic.
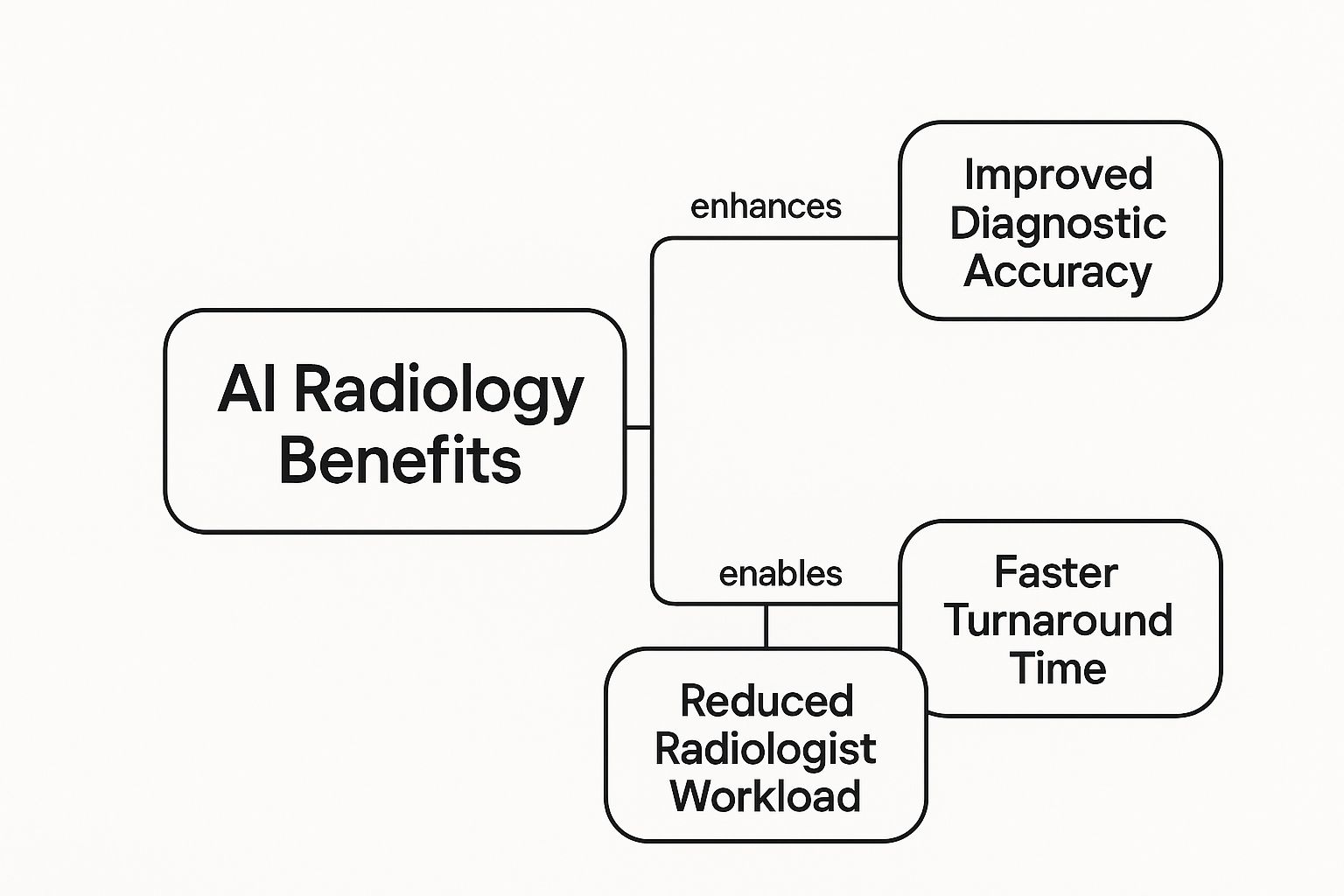
The image perfectly illustrates the link between the AI's learned abilities and the real-world benefits for a hospital, from boosting accuracy to making the workload more manageable for specialists.
From Learning to Performing Specific Tasks
Once an AI model is fully trained, it’s ready to perform specific, high-value jobs in the diagnostic workflow. It's not a single "do-it-all" tool but more like a collection of specialized skills. These skills are sharpened for particular tasks, much like how a human radiologist might specialize in neuroradiology or musculoskeletal imaging.
For instance, an AI tool built for oncology might be an expert at segmentation—the task of precisely outlining a tumor's borders. This is vital for planning radiation therapy or tracking how a tumor responds to treatment. On the other hand, an AI designed for the emergency room might focus on detection and triage, instantly flagging scans with signs of a stroke or pulmonary embolism to push them to the top of the radiologist's worklist.
Ultimately, the software "learns to see" by building a deep, statistical map of visual medical data. It doesn't have human consciousness or clinical judgment, but it delivers an incredibly powerful form of pattern recognition. When that's combined with a radiologist's expertise, it elevates the entire practice of medical imaging.
What AI Actually Looks Like in the Clinic

It's one thing to talk about algorithms and data, but it's another to see how AI radiology software changes the day-to-day reality in a busy hospital. The real value isn't just in the tech itself; it’s in how it transforms a high-pressure, often chaotic environment into something more manageable and efficient. Think of it as giving every radiologist a tireless, incredibly sharp assistant.
Let's step into a typical radiology department. Before AI, the worklist is just a long, chronological queue of scans. A radiologist might go from a routine chest X-ray to a complex brain MRI with no real way of knowing which case needs their attention right now. This linear slog can create dangerous bottlenecks, especially when a critical finding is buried halfway down the list.
Now, let's flip the switch and bring in AI. The software gets to work immediately, presorting that same list. It flags a potential brain bleed or a pulmonary embolism, automatically bumping it to the very top. This simple act of intelligent triage can shave precious minutes—or even hours—off the time to diagnosis for life-threatening conditions. The patient’s outcome can be improved before the radiologist even opens the study.
A Second Pair of Eyes for Greater Confidence
One of the most powerful roles AI plays is that of a reliable second reader. Radiologists are brilliant, but they’re also human. Fatigue, distractions, and crushing caseloads can make it tough to catch every single subtle detail on every scan. This is where AI shines. Trained on millions of images, these algorithms are exceptionally good at spotting faint patterns the human eye might miss.
For instance, an AI tool might highlight a tiny, easily overlooked lung nodule that indicates early-stage cancer. It doesn’t diagnose it—that's still the radiologist's job. Instead, it acts as a digital flag, drawing the expert's attention to a specific spot and prompting a closer look.
This partnership is the key. The AI provides an objective, data-driven nudge, while the radiologist applies their years of medical training and clinical context to make the final call. This synergy minimizes the risk of missed findings and builds a much higher level of confidence in the final report.
This growing trust in AI's ability to augment, not replace, human expertise is fueling its adoption. The market for AI in medical imaging, valued at USD 3.28 billion in 2024, is expected to explode to USD 96.82 billion by 2033. That’s not just hype; it's a reflection of the real-world value clinics are seeing. For a closer look at these numbers, check out this detailed market report.
Cutting Down Report Turnaround Time
Speed is another game-changer. A radiologist's work isn't just about spotting abnormalities. It involves tedious but critical tasks like measuring lesions, segmenting organs, and comparing current scans to previous ones. This all takes time.
AI automates these manual, repetitive jobs with remarkable speed and precision.
- Automated Quantification: Instead of a radiologist spending several minutes manually measuring a tumor's dimensions across dozens of CT slices, the AI can do it in seconds with perfect consistency.
- Lesion Tracking: For cancer patients, AI can automatically compare a new scan to a prior one, instantly showing if a tumor has grown, shrunk, or remained stable. This gives the radiologist an immediate snapshot of treatment effectiveness.
- Report Generation: Some advanced tools can even auto-populate report templates with all the standardized measurements and findings, freeing the radiologist to focus on crafting the narrative and final impression.
By taking these time-sinks off the radiologist's plate, AI radiology software drastically accelerates the entire process. Reports get back to referring physicians sooner, treatment decisions can be made faster, and anxious patients get their answers with less waiting.
Fighting the Burnout Epidemic
Radiology is facing a perfect storm: a growing shortage of specialists combined with a relentless increase in the number of imaging studies ordered. This imbalance is a recipe for burnout, which threatens both the well-being of physicians and the quality of patient care.
AI offers a very practical lifeline.
By automating the most monotonous parts of the workflow, AI allows radiologists to work at the top of their game. They can devote their focus and mental energy to the complex cases—the ones that truly require deep diagnostic expertise and critical thinking. This shift doesn't just lead to greater job satisfaction; it makes the entire diagnostic process more sustainable, safeguarding high-quality care for years to come.
AI Applications Across Imaging Specialties

The real power of AI radiology software snaps into focus when you see how it’s applied in different medical fields. It’s not some generic, one-size-fits-all tool. Instead, it’s a versatile toolkit that gets adapted to solve very specific clinical problems, whether in the chaos of an emergency room or the precision of an oncology clinic.
This specialization is a huge reason the industry is booming. The market for AI in radiology, sitting at around $2.2 billion in 2024, is projected to climb to $8.23 billion by 2029. That growth comes from applying this tech to the workhorses of imaging—CT, MRI, and X-ray—and tailoring it to what doctors in each specialty actually need.
Let's look at a few real-world scenarios to see how this technology delivers tangible benefits for both clinicians and their patients.
Neurology: Fast-Tracking Stroke Detection
In neurology, the mantra is "time is brain." When a patient shows up with stroke symptoms, every single second is critical. The immediate challenge is to look at a CT or MRI scan and figure out if an ischemic stroke—a blockage—is cutting off blood flow, because that determines the entire treatment plan.
This is where AI shines as a first responder. An algorithm, trained on thousands upon thousands of brain scans, can spot the faintest changes in tissue that signal a loss of blood flow. It can automatically highlight the location and size of the problem area, giving neurologists the information they need almost instantly.
This empowers the care team to make faster, more confident decisions about using clot-busting drugs, which have a very short window to be effective. For the patient, the benefit is massive: a quicker diagnosis means quicker treatment, which can dramatically improve their outcome and reduce the chance of long-term disability.
Cardiology: Quantifying Heart Function with Precision
Cardiologists live and breathe echocardiograms and cardiac MRIs. They use them to check on heart health, but manually measuring things like ejection fraction—the amount of blood pumped with each beat—can be tedious and can vary slightly from one doctor to another.
An AI tool built for cardiology automates this whole process. It can precisely outline the heart's chambers on an image and calculate critical metrics with a level of consistency humans can't match. This gets rid of the guesswork and provides a solid, objective baseline to track a patient's health over time.
By standardizing these measurements, AI helps ensure that a change in a patient's numbers reflects a true change in their heart function, not just a difference in how the measurement was taken. This leads to more accurate diagnoses of heart failure and better monitoring of treatment effectiveness.
For a deeper dive into how AI is being applied in clinical practice, you can explore the various applications within AI in Radiology Services.
Oncology: Tracking Tumors with Accuracy
For an oncologist, knowing exactly how a tumor is responding to treatment is everything. This usually means comparing multiple CT scans taken over months or even years to see if a lesion is growing, shrinking, or staying the same. Manually comparing these scans, slice by slice, is a painstaking and demanding job.
AI software brings both automation and precision to this task. It can:
- Segment Tumors: Automatically draw an exact outline of the tumor's boundaries on a scan.
- Calculate Volume: Give a precise volumetric measurement, which is far more accurate than just measuring the diameter.
- Track Changes: Compare the new scan to older ones, highlight any changes in size or density, and present it all in a report that's easy to digest.
This automated tracking frees up the radiologist's time and gives the oncologist objective, data-driven insights. For the patient, it means their treatment plan is based on the most accurate picture of their disease, allowing for faster and smarter adjustments to their therapy.
Emergency Medicine: Identifying Critical Findings on X-Rays
The emergency department is a pressure cooker. Chest X-rays are one of the most common exams performed, but a radiologist might have a long queue of them waiting to be read. The challenge is spotting something critical but subtle, like a collapsed lung (pneumothorax) or pneumonia, in the middle of that rush.
An AI triage tool can be a game-changer here. It scans every chest X-ray as it’s acquired and flags any with potentially urgent findings. If the algorithm thinks it sees signs of pneumonia, it can automatically move that study to the top of the radiologist's worklist. This simple step ensures the sickest patients get attention first, leading to faster care when it matters most.
A Guide to Choosing and Integrating AI Software
Picking the right AI radiology software is a major decision, and it goes way beyond flashy demos and vendor promises. You’re not just buying a piece of software; you’re making a serious investment in your clinical workflow, patient outcomes, and your team's sanity. A thoughtful evaluation process ensures you bring in a tool that actually delivers value, not just another layer of IT complexity.
Think of it like hiring a new, highly specialized member of your team. You’d vet their credentials, see how they perform in your specific environment, and make sure they communicate well with everyone else. A robust AI solution needs to be more than a clever algorithm—it has to be a validated, secure, and well-supported medical device. By following a clear roadmap and asking the right questions, you can navigate this process with confidence and find a partner that truly elevates your diagnostic capabilities.
Evaluating Potential AI Solutions
First things first: look past the marketing fluff and get down to the fundamentals of performance and safety. Not all AI tools are created equal, so you have to verify the claims. Start by confirming the software has the proper regulatory clearances for your region, like an FDA approval in the United States or a CE mark in Europe. These are non-negotiable—they prove the software has met strict standards for safety and effectiveness.
But regulatory clearance is just the price of entry. The real test is seeing how the algorithm performs with your data.
- Request a Pilot Study: The best way to know for sure is to test the software on a set of your own anonymized patient images. This is where the rubber meets the road. It shows you how the AI handles the specific patient demographics and imaging equipment unique to your institution.
- Assess Algorithm Accuracy: Ask for the hard numbers. You need to see detailed performance metrics on sensitivity (how well it finds disease) and specificity (how well it identifies healthy tissue). Compare these stats to published studies and, most importantly, to what you see in your own pilot.
- Ensure Clinical Relevance: The AI has to solve a real problem. Does it automate a mind-numbing, tedious task? Does it improve diagnostic accuracy for a particularly tricky condition? Even the most technically impressive tool is useless if it doesn’t address a genuine pain point in your daily workflow.
It's absolutely critical that the AI’s findings are easy to understand and act on. A "black box" algorithm that just spits out an answer without showing its work is far less useful than one that highlights its findings directly on the image. This lets radiologists quickly verify the results and place them in the proper clinical context.
Key Questions for Vendors
Once you’ve got a shortlist, it’s time to dig into the practical side of things. Your questions should laser-focus on integration, security, and what happens after the sale. This is about finding a long-term partner, not just a supplier.
Here are the essential questions you should be asking any AI radiology software vendor:
- Integration and Compatibility: How, exactly, does your software plug into our existing PACS and EHR? Is it a clean, seamless integration, or are we looking at a complex, custom-built project?
- Data Security and Privacy: What are you doing to keep our patient data secure and compliant with regulations like HIPAA? Where is the data processed—on our own servers or in the cloud—and what are the security protocols for each setup?
- Scalability and Performance: Can your solution handle our current imaging volume? What about in three years? We also need to know how running this software will impact our network and storage infrastructure.
- Training and Support: What kind of training do you provide for our radiologists and IT staff? What does your ongoing technical support look like, and what are your guaranteed response times when something goes wrong?
- The Business Case: Show us the math. Can you provide a clear return on investment (ROI) model? This should cover everything from time saved per study and potential for increased patient throughput to the impact on diagnostic accuracy.
The AI in medical imaging market is exploding—it was valued at USD 1.28 billion in 2024 and is projected to hit USD 14.46 billion by 2034. This massive growth, fueled by better tech and supportive policies, shows just how central these tools are becoming in modern healthcare. You can explore the market growth projections from Precedence Research for more details. Choosing the right partner now sets you up to ride this wave, not get swamped by it.
The Future of Augmented Radiology
The conversation around AI radiology software is changing. It's less about AI being a helpful assistant and more about it becoming a true diagnostic partner. We're moving into an era of augmented radiology, a model that isn't designed to replace radiologists but to elevate their expertise to a whole new level. The goal is to shift from just detecting today's diseases to actually forecasting future health risks, making patient care genuinely proactive.
This isn't science fiction; it's already starting to happen. The next big leap is from reactive diagnosis to predictive analytics. Instead of just spotting a tumor that's already there, AI is being trained to find incredibly subtle imaging biomarkers—faint patterns the human eye would almost certainly miss. These biomarkers can signal a patient's risk of developing a disease years before any symptoms show up.
Imagine this: a patient gets a routine chest CT. An AI analyzes the scan and flags them with a high statistical probability of developing lung cancer within five years, all based on microscopic patterns in their lung tissue. This insight allows doctors to start targeted monitoring and preventative care, completely altering that patient's long-term outcome.
Personalized Medicine Through Imaging
Looking ahead, AI's role in radiology is set to become deeply personal. It will be central to crafting individualized treatment plans by interpreting the unique biological story told within a patient's medical images.
For instance, two patients might have the same type of cancer, but their tumors could show very different genetic and textural signatures on an MRI. A sophisticated AI could analyze these complex details to predict which patient will respond better to a specific chemotherapy or immunotherapy.
This approach is known as radiomics. It’s the science of extracting massive amounts of quantitative data from medical images and connecting it to clinical outcomes. Essentially, radiomics turns a standard scan into a rich, personalized roadmap that helps oncologists choose the most effective therapy right from the start.
Democratizing Expertise Across the Globe
Perhaps one of the most exciting prospects is AI's power to make top-tier medical expertise available everywhere. In many parts of the world, getting a scan read by a sub-specialist radiologist is simply not an option. By integrating advanced AI radiology software with teleradiology platforms, we can finally close that gap.
- Global Access: A small, rural clinic could gain access to world-class diagnostic insights, with an AI providing an initial, expert-level analysis on any scan, day or night.
- Consistent Quality: The software introduces a reliable, high standard for image interpretation, smoothing out the inconsistencies that can occur between different facilities or even individual doctors.
- Knowledge Sharing: As these systems are adopted more widely, they'll build a global, anonymized data network that continuously trains and improves the algorithms for the benefit of everyone.
The impact of AI isn't limited to medicine; you can see parallels when looking at how AI is revolutionizing various software platforms across different industries. The future is collaborative—one where technology empowers clinicians to make smarter, faster, and more personalized decisions, pushing human health forward on a global scale.
Frequently Asked Questions About AI Radiology Software
As any hospital or imaging center starts looking into this technology, a lot of practical questions naturally come up. Getting these answered is the first step in building trust with the people who will actually use and manage the software—the radiologists, administrators, and IT staff.
Let's walk through some of the most common questions we hear.
Will AI Replace Radiologists?
The short answer is no. The consensus among experts is clear: AI is here to augment radiologists, not replace them.
Think of an AI tool as a highly specialized co-pilot. It’s brilliant at the tireless, repetitive work that can lead to human fatigue, like spotting a tiny nodule in a sea of images or taking precise measurements over and over. This frees up the radiologist to focus on the irreplaceable human element—applying deep clinical judgment to complex cases, collaborating with referring physicians, and providing nuanced patient care.
The goal isn't to create an automated radiologist but to build a partnership. It's about "augmented intelligence," where a physician's expertise is amplified by the AI's speed and consistency.
How Is AI Software Accuracy Validated?
Before an AI algorithm ever makes it into a clinical setting, it goes through a rigorous, multi-stage validation process to ensure it's both safe and reliable. It’s not a black box you just have to trust.
Here’s what that looks like:
- Training and Testing: First, the models are trained on massive, diverse, and completely anonymized imaging datasets. Their performance is then benchmarked against a "ground truth"—a definitive diagnosis established by a panel of expert radiologists or confirmed by something concrete, like a biopsy.
- Regulatory Scrutiny: In the United States, the FDA requires a mountain of evidence showing the software is safe and effective before it gets clearance for clinical use.
- Local Confirmation: Before going live, most hospitals conduct their own internal validation. They run the AI on their own patient scans to make sure it performs as expected with their specific imaging machines and patient demographics.
What Are the Main Implementation Challenges?
The biggest hurdles are usually technical and operational. Getting the new AI software to talk seamlessly with your existing IT infrastructure—especially the PACS and EHR systems—is a major technical lift. Data security and patient privacy are, of course, non-negotiable and at the top of the list.
But beyond the tech, the human side can be just as challenging. Change management is huge. You have to address the natural skepticism that comes with any new tool. Success hinges on clear communication about what the AI does (and doesn't do), along with hands-on training that gives the clinical team the confidence to integrate it into their daily workflow.