Picture this: a world-class radiologist's assistant who can scan thousands of images in seconds, flagging subtle details that need a closer look.That’s the core promise of artificial intelligence for radiology—a field where machine intelligence isn’t a replacement, but a powerful collaborator for human experts.
The New Era of Medical Imaging with AI
In modern healthcare, radiologists are grappling with a tidal wave of complex medical images. This surge in data, coupled with a global shortage of radiologists, puts immense pressure on diagnostic workflows. Artificial intelligence (AI) steps in here, not to take over, but to augment the abilities of these skilled professionals.
Think of it this way: a radiologist is a highly trained detective, meticulously searching for clues in medical scans. AI is their advanced forensics kit. It can analyze thousands of pieces of evidence in an instant, highlighting the most critical areas that demand attention. This partnership allows the human expert to focus their invaluable skills where they matter most, leading to faster and more accurate diagnoses.
Enhancing Human Expertise with Data
The real power of AI in radiology comes from its ability to learn from enormous datasets of medical images. By studying countless examples of both healthy and diseased tissue, these algorithms learn to spot patterns that might be too subtle or time-consuming for the human eye to consistently catch.
This translates into some very real benefits for the clinic:
- Reduced Workload: AI can take on routine, time-sucking tasks like measuring lesions or screening for common abnormalities. This frees up radiologists for the more complex and nuanced cases.
- Improved Consistency: It offers an objective, data-driven second opinion, which helps reduce the natural variability in interpretations between different readers.
- Faster Turnaround Times: By prioritizing urgent cases and speeding up the review process, AI helps get critical results into the hands of physicians and patients much more quickly.
The impact of integrating AI into a standard radiology practice is clear. It brings measurable improvements in both efficiency and accuracy, as this graphic shows.
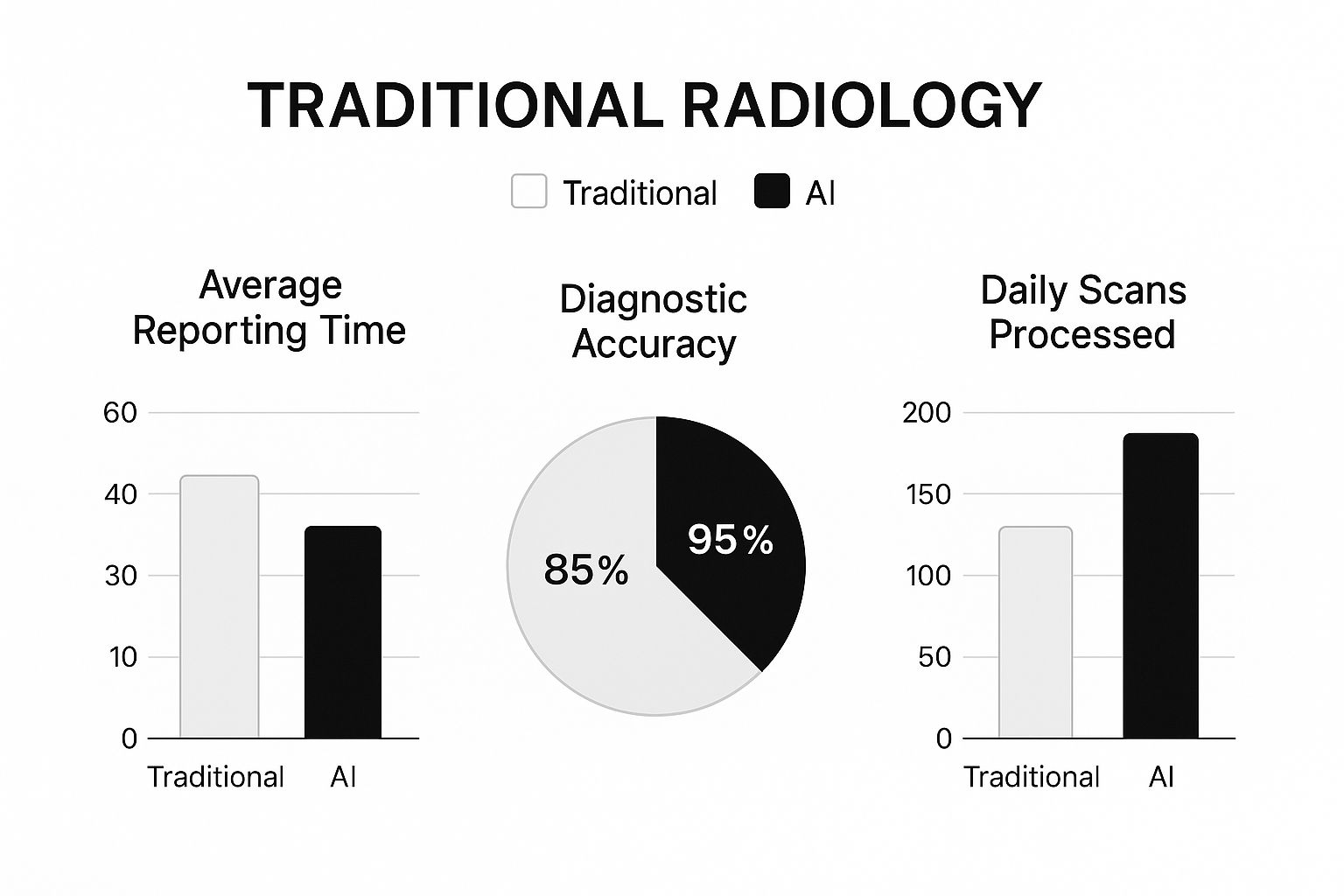
As the data illustrates, bringing AI into the workflow can dramatically cut reporting times while simultaneously boosting diagnostic accuracy and the number of scans a department can handle. The end result is a more efficient and effective environment that ultimately elevates the standard of patient care.
How AI Improves Diagnostic Accuracy and Speed
When we talk about AI in radiology, we're really talking about two fundamental improvements: making diagnoses more accurate and getting them done faster. Think of AI not as a replacement, but as an incredibly sharp, tireless assistant for the radiologist—one that can perceive patterns the human eye might miss, especially at the end of a long shift.
How does it do this? The magic is in the training. These algorithms learn from enormous, carefully prepared datasets of medical images. The quality of this training, specifically the image annotation, is what teaches the AI to tell the difference between healthy tissue and potential pathology with stunning reliability.
After analyzing millions of scans, an AI model builds an almost encyclopedic knowledge of anatomy and disease. It can then flag a tiny lung nodule, a hairline fracture, or the faintest signs of a developing condition that might otherwise be overlooked. It acts as a vital safety net.
This relationship between machine and expert is where the real power lies. The AI handles the heavy lifting of initial screening, allowing the radiologist to focus their expertise on the most challenging and nuanced cases that demand human judgment.
Accelerating Workflows and Triage
Beyond finding subtle abnormalities, AI is a massive accelerator for the entire diagnostic workflow. A busy hospital can be flooded with hundreds, sometimes thousands, of scans in a single day. This creates a backlog where urgent cases can get buried. AI tools can cut through this volume in minutes.
This speed translates into a few key benefits:
- Intelligent Triage: The AI can instantly spot and prioritize scans with red flags, like a potential stroke or pulmonary embolism. This bumps the most critical patients to the front of the line for immediate review.
- Faster Reporting: Many AI tools can pre-populate reports with standard measurements, lesion descriptions, and normal findings, significantly cutting down on tedious manual documentation.
- Enhanced Throughput: By offloading the more routine scans, departments can handle a higher volume of patients without burning out their staff. It’s about working smarter, not just harder.
A recent Northwestern Medicine study offers a compelling real-world example. They deployed a generative AI model across an 11-hospital network and analyzed nearly 24,000 reports. The result? Report completion became 15.5% more efficient on average, with some radiologists speeding up their workflow by as much as 40%. Crucially, this happened with no decrease in diagnostic accuracy. It's a clear demonstration of how this technology can help tackle radiologist shortages and deliver critical findings in seconds.
Practical AI Applications in Clinical Radiology
Let's move from the theoretical to the clinical floor, where AI is already making a real difference in patient care. These tools aren't some far-off dream; they are active in reading rooms right now, helping clinicians spot diseases earlier and with greater precision.
The applications are incredibly varied, spanning just about every subspecialty in medical imaging. At their heart, they all share a common goal: to enhance the radiologist's ability to find critical information quickly and confidently.
Detecting Disease Earlier and Faster
One of the most powerful roles for AI is in early disease detection. Think of it as a vigilant second pair of eyes, scanning for tiny abnormalities that could signal a condition in its most treatable stage.
Here’s what this looks like in practice:
- Mammography and Breast Cancer: AI models, trained on vast libraries of mammograms, are exceptionally good at identifying suspicious lesions or calcifications. They flag cases that need a closer look, which can lead to catching breast cancer much sooner.
- Chest X-Rays and Lung Nodules: Spotting a small, potentially cancerous lung nodule on a chest X-ray is a tough job. AI is built for this kind of detailed work, systematically scanning the entire lung field and highlighting areas of concern for the radiologist to review and confirm.
- Neuroimaging and Stroke Detection: When a stroke is suspected, every second is critical. AI can analyze brain CT scans in moments, flagging signs of a bleed or major blockage. This speed allows stroke teams to jump into action faster, saving precious brain function.
These AI tools essentially create an advanced triage system. By automatically flagging the most critical findings, they push urgent cases to the top of the worklist. This directly improves patient care by cutting down the time between diagnosis and treatment.
This visual from Vesta Teleradiology shows how AI is being used to build smarter screening and referral workflows.
As the screenshot shows, AI's role can extend beyond just analyzing images. It can also help manage departmental efficiency by intelligently routing procedure requests.
From Detection to Quantitative Analysis
AI’s job doesn’t stop at just finding problems. It also provides objective, quantitative data that used to be incredibly time-consuming, if not impossible, to get. Instead of a radiologist just observing that a tumor has grown, an AI tool can measure the change in its volume down to the millimeter.
This ability is a game-changer for tracking how a disease responds to treatment. In oncology, for instance, an AI can automatically measure a tumor’s size across multiple scans over time. This gives physicians a clear, data-driven picture of whether a treatment is working, helping them create more personalized and effective care plans.
In a similar way, when assessing conditions like multiple sclerosis, AI can precisely count the number of brain lesions and measure their total volume. This provides an objective metric for monitoring disease progression. This move from qualitative observation to quantitative measurement is a huge leap forward for evidence-based medicine, all driven by artificial intelligence for radiology.
Optimizing Workflows Beyond Image Analysis
When most people think about artificial intelligence for radiology, their minds jump straight to image analysis. And while that's a huge part of the story, AI's influence is reaching far beyond the reading room, quietly overhauling the entire operational backbone of the department.
Think of a busy radiology practice like an air traffic control center. The images are the planes, and the radiologists are the controllers guiding them. But behind the scenes, there's a mountain of coordination—scheduling arrivals, routing planes to the right gates, and handling all the paperwork. AI is stepping in to automate this "ground control," creating a more efficient and responsive environment for everyone involved.
Intelligent Routing and Scheduling
One of the most persistent bottlenecks in radiology is simply getting the right study in front of the right subspecialist. It happens all the time: a request for a complex neuroradiology exam lands on a generalist's worklist by mistake, leading to delays and frustrating manual rerouting.
AI is putting an end to this logistical headache. Modern workflow management systems can analyze incoming procedure requests and automatically assign them to the best-suited radiologist based on their subspecialty, availability, and even their current workload. It's a simple function, but its impact is massive, cutting down administrative lag and ensuring experts see the cases they were trained for.
This intelligent routing has been a game-changer for interventional radiology (IR). It can connect referring clinicians to the right IR provider almost instantly, preventing misplaced procedure orders and getting patients scheduled for treatment much faster.
The results speak for themselves. A recent study out of Duke University Medical Center used large language models (LLMs) to manage IR referrals. The system achieved a stunning 96.4% accuracy in routing requests correctly, all for a tiny cost of just $0.03 per query. This proves we have a scalable way to dramatically improve clinical coordination. You can find out more about these advances in AI-powered referral workflows.
Automating Reports and Documentation
The administrative load on radiologists is immense, with documentation consuming a huge chunk of their time. AI is providing much-needed relief here in a few practical ways:
- Preliminary Report Generation: LLMs can analyze images and clinical notes to draft structured, preliminary reports. These drafts highlight key findings, list measurements, and suggest standard impressions, giving the radiologist a solid starting point to review, edit, and finalize.
- Voice-to-Text Transcription: The growth of AI voice recognition in healthcare has been a lifesaver. Modern dictation systems now use AI to convert speech to text with incredible accuracy, easily handling complex medical terms and formatting reports as the radiologist speaks.
- Data Management: Behind the scenes, AI can automatically anonymize patient data for research projects, sort and archive studies based on specific protocols, and even flag missing or inconsistent information in the electronic health record.
By taking over these repetitive but critical tasks, AI gives radiologists their time back. This shift allows them to focus less on clerical work and more on what truly matters: solving complex diagnostic puzzles, consulting with patients, and collaborating with referring physicians. The end result is a smoother, less error-prone workflow from the moment a patient checks in to the final report being delivered.
The Financial and Operational Case for AI

While the clinical benefits of AI in radiology get a lot of attention, the business case for adopting it is just as strong. For any hospital administrator or practice manager, AI is a serious tool for boosting the bottom line and untangling the knots in daily operations. We're moving beyond just image analysis here—we're talking about tackling the core administrative and economic headaches that every radiology department knows all too well.
The financial upside often starts with the revenue cycle. Let’s be honest, revenue cycle management (RCM) is a complicated beast, full of traps that can trip you up. Manual medical coding, for example, is a classic source of errors that leads directly to claim denials and frustrating payment delays. AI can step in, analyze clinical reports and imaging data, and suggest the right codes, slashing the rate of human error.
Streamlining Revenue and Access
When you get your RCM automated, the positive effects ripple through your entire financial workflow. By submitting cleaner claims right out of the gate, AI naturally brings down your denial rate. That, in turn, cuts the administrative slog of appealing and resubmitting claims, leading to a faster and more reliable revenue stream.
But it’s not just about the money coming in. AI is also knocking down walls that prevent patients from getting the care they need, especially when it comes to prior authorizations. We've all seen how this painfully slow, manual process can put essential imaging procedures on hold for days or even weeks.
AI changes the game by analyzing clinical documents in real time and checking them against insurer rules. It can automatically pull together and submit the required information, drastically cutting down approval times. Patients get scheduled faster, and your staff gets back precious hours they used to spend on paperwork and phone calls.
When you add it all up, you’re looking at a much healthier and more efficient financial engine for the whole practice.
Optimizing Operations with Data
The other side of the AI coin is pure operational efficiency. Radiology departments are intricate ecosystems with countless moving parts—patient scheduling, scanner usage, staff assignments, you name it. AI-powered analytics give you a clear, data-driven look under the hood, helping you find those hidden bottlenecks and smart ways to improve.
For example, these analytics can show you:
- Underutilized Equipment: You might discover scanners sitting idle during specific blocks of time, which is a perfect opportunity to adjust scheduling and increase throughput.
- Staffing Inefficiencies: The data could reveal that patient volume consistently swamps your radiologists at certain times, pointing the way to smarter staffing choices.
- Workflow Delays: You can pinpoint exactly where things are slowing down, like the lag time between a scan being finished and the report becoming available.
AI is already making a huge impact on radiology billing and patient management. Tools that automate RCM are improving financial outcomes by correctly processing claims, minimizing errors with CPT and ICD-10 codes, and heading off denials before they happen. These improvements reduce the administrative load while also making for a better patient experience, proving AI’s value on both the clinical and business fronts. You can learn more about how AI is changing radiology billing on adsc.com.
By targeting these operational weak spots, AI helps you build a leaner, more responsive department that gets more done with the resources it already has.
Your Roadmap for Implementing AI in Radiology

Bringing artificial intelligence for radiology into your practice is much more than just a tech purchase; it’s a strategic shift. You need a clear, step-by-step plan that fits your unique clinical and operational reality. The real goal is to integrate these powerful tools in a way that truly helps your team, not just adds another layer of complexity to their day.
The first step, before you look at any software, is to ask: "What problem are we trying to solve?" Are you hoping to slash report turnaround times for urgent findings? Maybe you want to boost diagnostic accuracy for subtle conditions like early-stage lung cancer, or simply automate some of the administrative grunt work. Pinpointing clear, measurable goals is the only way to pick the right solution and know if it’s actually working down the line.
A successful AI implementation isn't about chasing the newest gadget. It's about solving a real-world problem for your clinicians and patients. Always start with the "why" before you get caught up in the "what" or "how."
Once you know what you’re aiming for, the real planning begins. This is where you have to think about data, technology, and, most importantly, people. Many AI initiatives hit unexpected roadblocks right here because these core elements weren't thought through properly.
Building Your Implementation Framework
A solid plan needs to address both the nuts-and-bolts technical side and the human element of introducing AI. It means making sure your current infrastructure can handle it and that your team is ready for the new way of working.
Here are a few key things to think about:
- Vendor Selection: Look for a partner who gets the clinical world, not just the code. Dig into their track record, check the regulatory status of their products (like FDA clearance), and find out what their support and training look like after the sale.
- Systems Integration: This is a big one. The AI tool you choose has to play nice with your existing Picture Archiving and Communication System (PACS) and Electronic Medical Record (EMR). A clunky integration will cause friction in your workflow and kill adoption before it even starts.
- Data Security and Compliance: Protecting patient data is absolute. Any solution you consider must be fully compliant with HIPAA and other regulations. You need to have frank conversations with vendors about how they handle data anonymization and security. For many, moving to the cloud is a foundational step to securely manage massive datasets and scale up AI efforts.
Managing Change and Fostering Adoption
Ultimately, whether this whole thing works comes down to your team. Radiologists and technologists are the ones who will use this technology every day, so their buy-in is everything. Get them involved right from the start—from setting the initial goals to beta-testing the software.
Good change management is all about open communication. Be clear that AI is here to augment their skills and make their jobs easier, not replace them. Offer comprehensive training and create a system for feedback so you can iron out wrinkles and adjust workflows after launch. When you empower your team, you're not just installing software; you're building a foundation for a smarter, more efficient future.
Common Questions About Bringing AI into Your Radiology Practice
Whenever new technology enters the medical field, it’s natural to have questions. Let's tackle some of the most common ones we hear about implementing artificial intelligence in radiology.
Will AI Replace Radiologists?
This is probably the biggest question on everyone's mind. The short answer is no. The overwhelming consensus is that AI will empower radiologists, not replace them.
Think of it this way: AI is becoming an incredibly sophisticated co-pilot. It’s brilliant at handling the high-volume, repetitive tasks and flagging potential issues that a human eye might miss after a long shift. This frees up the radiologist to focus on the truly complex cases, consult with other physicians, and interact with patients—areas where human expertise, empathy, and critical judgment are absolutely essential.
The phrase you'll hear a lot, because it's true, is: "AI won't replace radiologists, but radiologists who use AI will replace those who don't."
What Is the Real Cost of an AI System?
The sticker price for the software is just the beginning. To get a realistic picture of the investment, you need to factor in several other costs.
You'll have to consider the expense of integrating the new system with your existing PACS and EMR, which can be a complex technical project. There might also be hardware upgrades needed to run the AI models effectively. Don't forget the ongoing costs, like maintenance plans or annual subscription fees, and—critically—the budget for training your staff. Proper training is what turns a powerful tool into a useful one.
A critical first step is to define a clear problem you want to solve. This focus helps avoid overspending on features you don't need and ensures any investment in AI for radiology delivers tangible value.
Ready to build the future of medical imaging? PYCAD offers end-to-end services, from data handling to model deployment, to bring your AI-powered vision to life.






