The Evolution of AI in Radiology: From Basic Tools to Brilliant Diagnostics
The field of radiology has dramatically changed since the days of meticulously reviewing blurry films. Early computer-aided detection (CAD) systems were the first step toward automating image analysis, concentrating on identifying straightforward patterns. This initial shift began the move from purely human interpretation to a more technologically driven approach, setting the stage for more sophisticated uses of artificial intelligence in radiology.
Early Stages of AI in Radiology
The initial AI algorithms were designed to find specific, well-defined characteristics in medical images. Early CAD systems, for example, could flag potential microcalcifications in mammograms or identify possible lung nodules on chest X-rays.
However, these early systems relied on manually crafted features and couldn't adapt to the variations found in medical images. This often resulted in inconsistent performance and a tendency toward false positives, highlighting the need for more sophisticated and adaptive technologies.
The Deep Learning Revolution
The introduction of deep learning in the 2010s represented a major advance. Inspired by the human brain, deep learning algorithms can learn complex patterns from massive amounts of data. This has allowed AI systems to analyze medical images with increased accuracy, identifying subtle anomalies a human eye might miss.
To illustrate the progress of AI in radiology, the following table outlines key milestones in the field:
To understand the evolution of AI in radiology, let's look at the key milestones:
Evolution of AI in Radiology: Key Milestones
| Time Period | Technology Development | Clinical Impact |
|---|---|---|
| 1970s | Invention of Computed Tomography (CT) | Revolutionized medical imaging with cross-sectional views of the body |
| 1980s – 1990s | Early Computer-Aided Detection (CAD) Systems | Automated identification of simple patterns, primarily for mammography and chest x-rays |
| 2010s | Rise of Deep Learning | Development of algorithms capable of learning complex patterns from vast datasets, leading to improved accuracy and identification of subtle anomalies |
| Present | Integration of AI into clinical workflows | AI assists radiologists with diverse tasks, including lesion detection, image segmentation, and automated reporting, increasing efficiency and diagnostic precision |
This table shows the evolution from the basic technology of CT scans to breakthroughs in deep learning and the integration of AI into radiology practices.
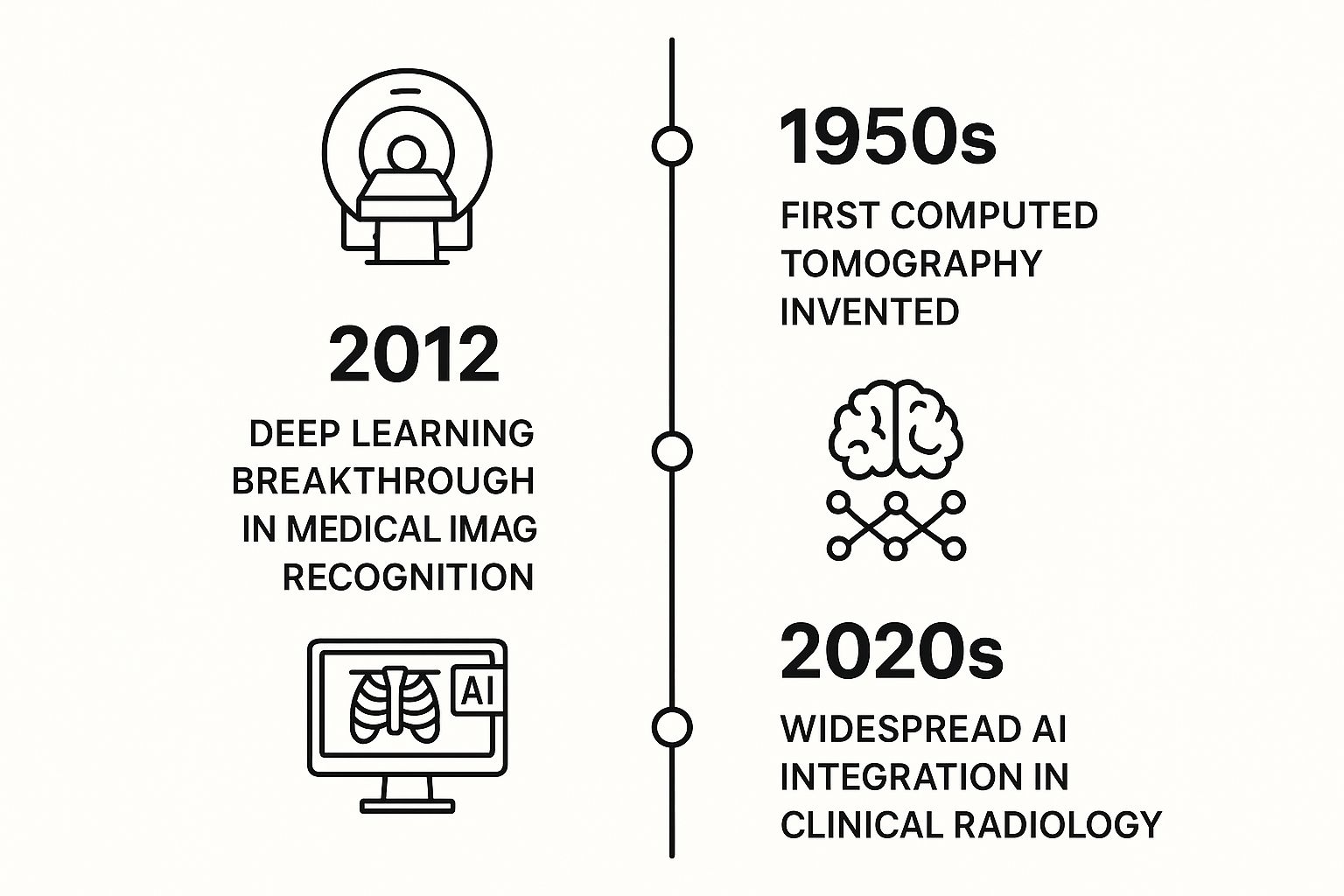
This timeline visualization further emphasizes how far the field has come. The deep learning breakthrough of 2012 was a pivotal moment in medical image recognition. AI Will Be An Integral Part Of Your CS Tech Stack.
The global market for AI in medical imaging is growing rapidly. From a value of USD 1.28 billion in 2024, the market is projected to reach approximately USD 14.46 billion by 2034, with a CAGR of 27.10%. AI in Medical Imaging Market Size This growth underscores AI's potential to enhance diagnostic accuracy and efficiency in radiology.
The Future of AI in Radiology
Today, AI algorithms analyze images from various sources, including X-rays, CT scans, MRI, and ultrasound. They assist radiologists with tasks ranging from spotting small lesions to automating routine measurements. This continuing progress is poised to further improve diagnostic abilities and transform how radiology is practiced. The use of AI in radiology has evolved from a futuristic idea to a crucial tool, improving patient care and reshaping the field.
Seeing What Humans Miss: How AI Transforms Diagnostic Accuracy

Even highly trained radiologists can sometimes overlook subtle details, particularly after reviewing numerous images. This natural human limitation highlights the potential of Artificial Intelligence (AI) in radiology. Unlike humans, AI algorithms don't experience fatigue and can consistently process vast quantities of data. This ability allows AI to improve diagnostic accuracy by identifying anomalies that might be missed by human eyes.
AI's Impact on Diagnostic Accuracy
AI excels at recognizing subtle patterns and variations in medical images. For instance, AI algorithms can detect tiny calcifications in mammograms, which can indicate early-stage breast cancer, that may be missed during manual review. AI can also identify small lung nodules on chest X-rays. Furthermore, AI can pinpoint intracranial hemorrhages with remarkable precision. These examples show how AI can act as a valuable second reader, helping radiologists make more accurate diagnoses.
AI-powered tools are also proving invaluable in identifying subtle signs of disease progression. This early detection is crucial for informing treatment decisions and improving patient outcomes. In time-sensitive situations, such as stroke diagnosis, AI can analyze images and flag critical findings faster than traditional methods. This allows for quicker intervention, potentially minimizing long-term consequences.
The Synergy Between Human Expertise and AI Precision
While AI algorithms are enhancing diagnostic capabilities, human expertise remains essential. Radiologists possess crucial clinical knowledge and contextual understanding. This allows them to interpret AI findings in conjunction with patient history and other diagnostic information. AI is not intended to replace radiologists but to enhance their abilities, creating a more effective diagnostic process. Leading institutions are forming “diagnostic dream teams” where radiologists and AI work together, leveraging each other’s strengths.
This collaborative approach is leading to real-world improvements in patient care. By reducing false negatives, AI helps ensure patients receive timely and effective treatment. Improved accuracy also reduces the need for unnecessary follow-up examinations and procedures. This can minimize patient anxiety and lower healthcare costs. The global AI in radiology market highlights this growing trend. Its current value of about USD 310 million in 2022 is projected to reach USD 2154.4 million by 2032. You can find more detailed statistics here. Just as AI is transforming radiology, it's also changing wealth management. You can explore the Evolution of AI in Modern Wealth Management.
The following table offers a comparison of diagnostic performance between traditional radiology and AI-assisted radiology:
AI vs. Traditional Radiology: Diagnostic Performance Comparison
This table compares diagnostic accuracy metrics between AI-assisted and traditional radiological interpretations across different conditions.
| Condition | Traditional Radiology Accuracy | AI-Assisted Accuracy | Improvement |
|---|---|---|---|
| Breast Cancer Detection (early stage) | 85% | 92% | 7% |
| Lung Nodule Detection | 78% | 89% | 11% |
| Intracranial Hemorrhage Detection | 90% | 95% | 5% |
This table showcases the potential for improvement in diagnostic accuracy across a range of conditions when AI is integrated into radiological practices. While traditional radiology maintains a solid baseline, AI assistance demonstrates a consistent improvement in accurately identifying critical findings. This data underscores the potential of AI to enhance patient care through earlier and more accurate diagnoses.
AI technology continues to advance, promising further progress in diagnostic accuracy and patient care in radiology and other medical fields.
Breathing Room: How AI Is Rescuing Radiologists From Burnout
The ongoing radiologist shortage continues to strain healthcare systems. This leads to increased workloads and the potential for burnout among these highly skilled professionals. Artificial intelligence (AI) in radiology offers much-needed support, transforming overwhelmed departments into more efficient diagnostic centers.
AI-Powered Workflows: Prioritizing and Automating
One key benefit of AI is its ability to prioritize critical cases. AI algorithms analyze incoming images and flag those needing immediate attention, such as a suspected stroke or pulmonary embolism. This allows radiologists to focus their expertise where it’s most urgently needed.
AI also automates time-consuming tasks. For instance, AI can perform routine measurements of organs and lesions. This frees up radiologists to concentrate on more complex image interpretations and valuable patient consultations. Automating the generation of structured reports further reduces administrative burdens.
Delegating Tasks, Reclaiming Time
Many repetitive tasks can be safely delegated to AI assistants. These include bone age assessments, basic chest X-ray interpretations, or initial reviews of mammograms for obvious abnormalities.
This delegation allows radiologists to dedicate more time to demanding tasks, like analyzing complex MRI scans or discussing findings with patients and colleagues. This increases efficiency and lets radiologists focus on the most rewarding aspects of their profession.
Faster Turnaround Times, Improved Quality, and Job Satisfaction
Forward-thinking institutions are using AI to significantly reduce turnaround times. AI-powered workflows can shorten reporting times, sometimes from days to just hours. This allows patients to receive diagnoses and begin treatment sooner.
AI provides a second set of "eyes," reducing human error and potentially improving diagnostic quality. By alleviating workloads, automating tedious tasks, and boosting diagnostic confidence, AI contributes to greater job satisfaction among radiologists. This renewed focus on patient care and complex diagnostics can reignite professional passion.
Addressing Integration Challenges
While AI offers significant advantages, integration challenges require attention. Implementing new technologies necessitates careful planning and staff training. Ensuring data privacy and addressing potential biases in algorithms are also crucial.
However, many institutions are successfully navigating these challenges by partnering with experienced AI providers. This demonstrates the potential for seamless adoption and maximizing the benefits of AI for both patients and radiologists.
Beyond X-Rays: How AI Is Transforming Every Imaging Modality
Artificial intelligence is rapidly changing the field of medical imaging. Its impact extends far beyond X-rays, influencing virtually every imaging modality. Let's explore how AI is making a difference across radiology, from CT and MRI to ultrasound and nuclear medicine.
AI-Powered CT: Reducing Radiation and Enhancing Image Quality
Computed Tomography (CT) scans provide highly detailed anatomical images, but they also expose patients to radiation. AI is helping to mitigate this risk. Sophisticated AI algorithms can reconstruct high-quality CT images from lower-dose scans. This allows healthcare providers to significantly reduce radiation exposure while maintaining the diagnostic quality necessary for accurate interpretations. This is particularly important for patients requiring frequent scans, such as those undergoing cancer treatment monitoring.
Streamlined MRI: Cutting Scan Times and Improving Patient Comfort
Magnetic Resonance Imaging (MRI) can be a time-consuming and sometimes uncomfortable experience for patients. AI is helping to address this issue. AI-powered acquisition protocols optimize the way MRI data is collected, leading to significant reductions in scan times—in some cases, by as much as 50%. This not only improves patient comfort but also increases department efficiency, enabling a higher patient throughput and reducing wait times for crucial diagnoses.
Ultrasound Guidance: Enhancing Diagnostic Accuracy for Less Experienced Practitioners
Ultrasound imaging is highly operator-dependent. The quality of the images relies heavily on the skill and experience of the sonographer. AI-powered guidance systems are changing this dynamic by providing real-time feedback and adjustments during ultrasound examinations. These systems help less experienced practitioners obtain diagnostic-quality images consistently, leading to more accurate diagnoses, especially in areas with limited access to highly trained sonographers.
Nuclear Medicine and PET Scans: Enhancing Interpretation and Treatment Planning
AI is also making significant strides in nuclear medicine, particularly in Positron Emission Tomography (PET) scans. AI algorithms enhance PET scan interpretation by detecting subtle changes in metabolic activity that could indicate the presence of disease. This detailed information aids in more precise treatment planning, especially for cancer patients. By providing a more complete picture of the disease’s extent and activity, AI empowers more personalized medicine approaches.
Real-World Implementation and Practical Guidance
The examples above represent just a glimpse into how AI is transforming the field of radiology. Each application brings its own set of real-world implementation stories, measurable improvements, and practical considerations for radiology departments looking to integrate AI solutions. Data from these implementations demonstrate tangible performance gains in terms of speed, accuracy, and overall efficiency, offering invaluable guidance for other institutions exploring AI in radiology. The continued success of these implementations drives further innovation and wider adoption of AI in medical imaging, shaping the future of the field.
The Trust Factor: Navigating AI Radiology's Ethical Landscape

As artificial intelligence (AI) becomes more prevalent in radiology, it brings important ethical considerations. Responsible implementation requires careful attention to potential biases, patient consent, data security, and regulatory compliance. Establishing clear guidelines and best practices is essential to ensure AI benefits patients while upholding the highest ethical standards.
Addressing Algorithmic Bias and Patient Outcomes
AI algorithms learn from the data they are trained on. If this data reflects existing societal biases, the algorithm may perpetuate or even amplify these biases, potentially leading to disparities in patient care. For example, an algorithm trained primarily on images from one demographic group might be less accurate when analyzing images from other groups.
Identifying and mitigating these biases is crucial for ensuring equitable access to high-quality AI-powered radiology services. One approach is to use diverse and representative datasets for training AI models. Regular audits of AI systems can also help identify and address any emerging biases after deployment.
Navigating the Regulatory Landscape and FDA Approval Pathways
The regulatory landscape for AI in healthcare is constantly evolving. Understanding current Food and Drug Administration (FDA) approval pathways is crucial for institutions implementing AI solutions. This includes staying updated on guidelines for premarket submissions, clinical trials, and post-market surveillance.
Compliance with these regulations ensures patient safety and builds trust in the use of AI in radiology. Working closely with regulatory experts and legal counsel is vital for navigating this complex landscape and ensuring all AI tools are used responsibly and legally.
Patient Consent and Transparent AI Practices
The use of AI in medical decision-making raises important questions about patient consent. How do we ensure patients understand how AI is being used in their care? Transparency is key.
Providing clear and accessible information to patients about the role of AI in their diagnosis and treatment is critical. This includes explaining how AI assists radiologists, the potential benefits and limitations, and how their data is being protected. Open communication fosters trust and empowers patients to make informed decisions about their healthcare.
Data Security and Responsible AI Implementation
AI systems in radiology rely on access to large amounts of patient data. Protecting the privacy and security of this data is paramount. Implementing robust data security measures, including encryption and access controls, is essential.
Additionally, institutions should establish clear protocols for data governance and anonymization. This responsible approach safeguards sensitive information and maintains patient confidence.
Building Ethical Frameworks for AI in Radiology
Developing practical frameworks for evaluating AI systems before implementation is crucial. This involves assessing potential ethical risks, addressing bias concerns, and establishing clear accountability for AI-generated results. Ongoing monitoring after deployment is equally important to detect unintended consequences and make necessary adjustments.
This proactive approach is essential for ensuring the responsible adoption of AI in patient care settings. By combining technical expertise with ethical considerations, we can build a future where AI enhances radiology while prioritizing patient well-being and trust.
Partners, Not Replacements: Building the Radiologist-AI Dream Team
The conversation surrounding artificial intelligence (AI) in radiology often centers on the idea of machines replacing human radiologists. However, the real power of AI lies in its ability to collaborate with radiologists, forming a strong partnership. This collaboration is transforming diagnostic workflows, leveraging both human expertise and the precision of machines.
A Day in the Life With AI: How Workflows Are Evolving
Imagine a radiologist beginning their workday. Instead of facing a massive backlog of images, an AI system has already pre-screened and prioritized cases based on urgency and potential findings. Perhaps an AI tool has identified a small lung nodule on a chest X-ray, bringing it to the radiologist's attention – an area that might have been missed after hours of reviewing images. This prioritization allows radiologists to focus their specialized skills on the most complex and subtle interpretations.
The AI can then automatically perform routine measurements of the nodule, saving the radiologist valuable time. This efficiency allows them to move quickly to other critical cases, perhaps analyzing intricate brain abnormalities on MRI scans. It also frees up more time for essential discussions with patients and their care teams.
Essential Skills for the AI-Powered Radiologist
Radiologists are adapting and acquiring new skills to thrive in this collaborative environment. A core skill is the critical assessment of algorithmic outputs. This involves understanding the inherent limitations of AI, recognizing potential biases, and confidently evaluating the reliability of AI-generated results.
Another key skill is the ability to focus expertise on the most demanding cases. As AI handles routine tasks, radiologists can dedicate their time to cases requiring detailed analysis, incorporating clinical context, and collaborating with other specialists.
Emerging Career Opportunities: Radiology Informatics and AI Quality Assurance
The integration of AI into radiology is creating exciting new career paths. Radiology informatics specialists are becoming indispensable for designing, implementing, and managing AI-driven workflows. These professionals bridge the gap between technology and clinical practice, ensuring seamless integration and optimal use of AI tools.
AI quality assurance is another expanding field. Professionals in this area concentrate on evaluating the performance and safety of AI systems, monitoring for biases, and guaranteeing reliable and ethical AI deployment within radiology departments.
The Impact of AI on Professional Satisfaction and Future Outlook
Radiologists at all career stages are experiencing the positive effects of AI. Many are reporting increased job satisfaction due to reduced workloads, streamlined workflows, and a renewed focus on the most intellectually stimulating aspects of radiology.
AI offers invaluable learning opportunities for trainees. By observing AI-generated findings and comparing them with expert interpretations, trainees gain a deeper understanding of image analysis and diagnostic reasoning.
For experienced radiologists, AI serves as a powerful tool to expand their capabilities and allow them to contribute at even higher levels. By handling routine tasks, AI frees radiologists to concentrate on challenging diagnostic puzzles and contribute to groundbreaking research.
Practical Guidance for Departments Transitioning to Human-AI Workflows
Transitioning to a human-AI collaborative workflow requires careful planning and implementation. Start by identifying tasks well-suited for AI assistance, such as initial image screening, automated measurements, and report generation.
Next, prioritize staff training on the effective use and interpretation of AI-generated results. Establishing clear communication between radiologists and informatics specialists is crucial for addressing integration challenges and optimizing workflows. Finally, continuously monitor AI performance and gather feedback from radiologists to refine and improve AI-assisted practices.
Ready to explore how AI can transform your radiology department? PYCAD offers complete solutions, from data handling and model training to seamless deployment. Learn more about how PYCAD can help you build your radiologist-AI dream team.






