Computed Tomography (CT) 3D reconstruction is the process of taking hundreds of flat, 2D scan images and digitally stacking them to create a single, interactive 3D model. This technology transforms the raw data from a CT scanner into a tangible anatomical structure, giving clinicians a complete view they can rotate and examine from any angle.
From 2D Slices to a Dimensional View
Think of a standard CT scan as a loaf of sliced bread. Each individual slice gives you a look at the inside, but you only see a flat, 2D cross-section. It's useful, but it doesn't give you a sense of the whole loaf. To really understand the shape, texture, and structure, you need to see all the slices together.
That’s exactly what computed tomography 3D reconstruction does. It uses sophisticated software to digitally reassemble those individual "slices" of patient anatomy. The process turns a mountain of abstract data points into a complete, interactive 3D model that you can actually work with. It's almost like building a complex model brick by brick, where each scan slice adds another layer of depth and context.
This leap in technology takes medical imaging from being a collection of static pictures to a dynamic, explorable tool. Instead of mentally trying to piece together anatomy from a series of flat images, clinicians can now interact with a "digital twin" of a patient's internal structures.
The Power of Perspective
Being able to turn a 3D model around in virtual space provides insights that are nearly impossible to get from 2D scans alone. By rotating, zooming, and even digitally dissecting the model, medical professionals get a much clearer understanding of complex spatial relationships. This is a game-changer in several critical areas:
- Surgical Planning: A surgeon can map out a complex procedure with millimeter precision, identifying exactly where a tumor sits in relation to vital organs and blood vessels—all before even entering the operating room.
- Disease Diagnosis: The complete, three-dimensional view helps radiologists spot subtle abnormalities and grasp the full extent of a disease, which ultimately leads to more accurate and confident diagnoses.
- Patient Communication: A 3D model is incredibly intuitive. It’s far easier for a doctor to explain a patient's condition or walk them through a planned surgery using a visual model they can both see and understand.
The core benefit of computed tomography 3D reconstruction is its ability to translate complex, layered data into a single, intuitive visual format. This shift from 2D interpretation to 3D interaction fundamentally improves clinical decision-making and safety.
At its heart, this technology bridges the gap between raw data and real-world understanding. It creates powerful diagnostic assets that have become central to modern medicine. The two primary methods used to create these visuals are Surface Rendering and Volume Rendering, each with its own specific strengths.
Key 3D Reconstruction Rendering Techniques
To bring these 3D models to life, reconstruction software relies on rendering techniques. The two most common methods, Surface Rendering and Volume Rendering, are chosen based on what the clinician needs to see. Each offers a different kind of visual output, tailored for specific diagnostic tasks.
This table breaks down the two primary techniques, highlighting what they do best and why you'd choose one over the other.
| Technique | Visual Analogy | Best For Visualizing | Key Advantage |
|---|---|---|---|
| Surface Rendering (SR) | A 3D map of a coastline | Bones, implants, organ surfaces | Creates a clear, solid view of outer structures, ideal for orthopedic planning. |
| Volume Rendering (VR) | Looking into a glass of water | Soft tissues, vascular networks, tumors | Provides a semi-transparent view to see through objects and understand spatial relationships. |
Essentially, if you need to see the solid surface of an object, like planning a bone screw placement, Surface Rendering is your go-to. But if you need to see through structures to understand how they relate—like tracking a blood vessel as it weaves through muscle—Volume Rendering provides that crucial see-through capability.
From Grainy Images to High-Fidelity Models
To really get a feel for the power of modern computed tomography 3D reconstruction, it helps to look back at its origins. It's a story of incredible ingenuity and computational grit, a time when the whole process was painstakingly slow and felt like something straight out of science fiction.
The journey kicked off with the groundbreaking work of Godfrey Hounsfield and Allan Cormack. Their efforts led to the very first CT scan on a live patient on October 1, 1971. The scanner itself was a masterpiece of resourcefulness, pieced together with parts salvaged from a lathe. The process was a marathon: a single scan took about nine days to finish, with another 2.5 hours of computer time just to put the image together. You can discover more about these early technological hurdles and see how they paved the way for today's imaging.
Those early systems were a world apart from what we have now. The first images were incredibly low-resolution, starting at a mere 32×32 pixels. By 1969, even with mainframe computers, the resolution only crawled up to a grainy 80×80 pixels. Just storing this data was a physical ordeal—a single image was saved on a roll of paper tape that could stretch 90 meters long.
Overcoming the Computational Bottlenecks
The biggest roadblock wasn't the X-ray technology itself. It was the sheer computational muscle needed to crunch all the data. Think about it: creating one photographic print from the scan data took a full 60 minutes. The idea of generating hundreds of slices and assembling them into a 3D model was simply out of reach for any practical clinical setting.
This history is so important because it shows us that the core challenge of 3D reconstruction has always been about wrangling huge amounts of information. The leap from those first fuzzy images to the crisp, detailed models we see today is a direct result of overcoming these computational hurdles.
The progress in CT imaging is a tale of two advancements running in parallel: the refinement of scanner hardware and the explosive growth of computing power needed to interpret the data. One could not have succeeded without the other.
Every jump in processing speed and every new, more efficient algorithm unlocked another layer of detail. The slow, methodical reconstruction of the 1970s laid the foundation for the near-instantaneous results that medical professionals now depend on.
From Static Slices to Dynamic Models
In the early days, radiologists worked with 2D slices. They would look at these cross-sections one by one, mentally stacking them to build a three-dimensional picture of the patient's anatomy. This took immense skill and experience, but it was still easy to miss things, especially in complex cases.
The real game-changer came when computers became powerful enough to do the "stacking" automatically and render a complete volumetric model. This shifted the heavy lifting from the clinician to the machine, freeing up experts to focus on what they do best: analysis and diagnosis.
This transition was the birth of modern computed tomography 3D reconstruction as we know it. It was no longer about just looking at pictures; it was about interacting with a dynamic digital object. This evolution has brought several key improvements:
- Enhanced Detail: We've gone from an 80×80 pixel grid to resolutions often exceeding 512×512. This allows us to see tiny structures like small blood vessels and intricate fracture lines that were previously invisible.
- Faster Turnaround: What once took days of processing can now be done in minutes, sometimes even seconds. This speed is critical in emergency rooms and busy clinics.
- Improved Accessibility: User-friendly software has made 3D reconstruction a standard tool, not just for radiologists but for a wide range of medical specialties.
What started as a slow, laborious experiment has become an essential part of medicine. The journey from paper tape and grainy pixels to interactive, high-definition models is a powerful story about the drive for better diagnostic tools, and it has fundamentally changed how we see inside the human body.
How Algorithms Build a 3D Picture
The leap from hundreds of flat, grayscale scan images to a single, interactive 3D model isn't magic—it's math. This transformation is driven by sophisticated algorithms, the invisible engines at the heart of computed tomography 3D reconstruction. They translate raw data into the detailed anatomical views that clinicians rely on every day.
Think of it like two artists being given the same raw materials but using different techniques to create a masterpiece. The two dominant approaches in CT are Filtered Back Projection and Iterative Reconstruction, and each has a unique way of building the final picture.
Filtered Back Projection: The Shadow Puppet Theater
The classic and most established algorithm is Filtered Back Projection (FBP). To get a feel for how it works, picture a shadow puppet theater. If you shine a single light on a puppet, you get one flat shadow—its projection. That shadow gives you a general idea of the shape, but you can’t see any depth or detail.
Now, imagine you have lights positioned all around the puppet, each casting its own unique shadow. FBP operates on a similar principle. The CT scanner captures hundreds of projections (the "shadows") from every angle around the body. The "back projection" step is like layering all of those shadows on top of one another.
As you stack more and more of these projections, a clearer, more defined picture of the original object starts to take shape. The "filtered" part of the name refers to a crucial mathematical step that sharpens the image and smooths out the inevitable blurring, ensuring the final model is crisp and clear. For decades, FBP was the undisputed workhorse of CT imaging, prized for its raw speed.
This technology took hold incredibly fast. By 1980, just a few years after its clinical debut, three million CT scans were being performed worldwide. This explosive growth was driven by the machine's novel ability to create cross-sectional images that computers could then build into detailed anatomical models—a massive leap from flat 2D X-rays. You can dig deeper into this rapid adoption by exploring the history of the CT scan.
Iterative Reconstruction: The Digital Sculptor
While FBP is fast, it has its limits. It can struggle with "noisy" data and sometimes creates distracting artifacts, especially when using low-dose scan protocols. This challenge paved the way for a more refined and computationally intensive method: Iterative Reconstruction (IR).
If FBP is about layering shadows, think of IR as a sculptor methodically chipping away at a block of clay. The process begins with an initial guess—a very rough 3D model. The algorithm then simulates what the CT projections should look like based on that guess. Next, it compares these simulated projections to the actual raw data from the scanner, carefully identifying any differences or errors.
Using this feedback, the algorithm refines the model and starts the process all over again. With each cycle, or "iteration," the 3D model gets progressively closer to the patient's true anatomy.
Think of Iterative Reconstruction as a continuous feedback loop. It makes a guess, checks its work against the real data, corrects its mistakes, and tries again. This meticulous process results in a higher-quality image with fewer imperfections.
This approach offers two huge benefits:
- Superior Image Quality: IR algorithms are fantastic at reducing image noise, which means clearer, more detailed models. This is particularly valuable for visualizing subtle differences in soft tissues.
- Lower Radiation Dose: Because IR can create excellent images even from less-than-perfect data, clinicians can significantly lower the radiation dose during the scan, a major win for patient safety.
Choosing the Right Algorithmic Tool
So, which one is better? The choice between FBP and IR often comes down to balancing clinical priorities. FBP is still used in situations where sheer speed is the most critical factor. However, the powerful combination of better image quality and lower radiation exposure has made IR the new standard for a vast range of applications.
Ultimately, both algorithms are incredible feats of mathematics. They are the essential bridge connecting the physical act of scanning a patient to the interactive digital models that define modern medicine. Without these engines working tirelessly behind the scenes, the detailed visualizations we now take for granted simply wouldn't exist.
From 2D Slices to a 3D Model: The Reconstruction Workflow
So, how do we get from a series of flat, black-and-white CT images to a fully interactive 3D model? It's a fascinating process that combines sophisticated software with a healthy dose of human expertise. Each step carefully builds on the last, turning raw data into a powerful tool for doctors.
The entire computed tomography 3d reconstruction workflow can be broken down into four core stages. Think of it as an assembly line for medical data, where each station refines the product until it's ready for clinical use.
Stage 1: Data Acquisition
Everything starts at the CT scanner. As the machine's gantry rotates around the patient, it captures a massive number of X-ray projections from hundreds of different angles. The scanner's internal computer then does the initial heavy lifting, mathematically crunching this raw data into a stack of cross-sectional images, often called axial slices.
These slices are the foundational building blocks for our 3D model. The quality of these initial images—especially how thin the slices are and their overall resolution—has a huge impact on the final result. Better ingredients make a better cake.
Stage 2: Pre-processing
Once the 2D slices are generated, they move into a clean-up phase known as pre-processing. Raw CT images aren't always perfect; they can have "noise" (which looks like graininess) or artifacts, which are streaks and shadows often caused by things like metal implants or even the patient moving slightly.
Pre-processing algorithms act like a digital filter, smoothing out the noise and correcting for these artifacts. This step is critical because it ensures the data is as clean and accurate as possible before the real reconstruction work begins. You have to get this right, otherwise, small errors here can become big problems later on.
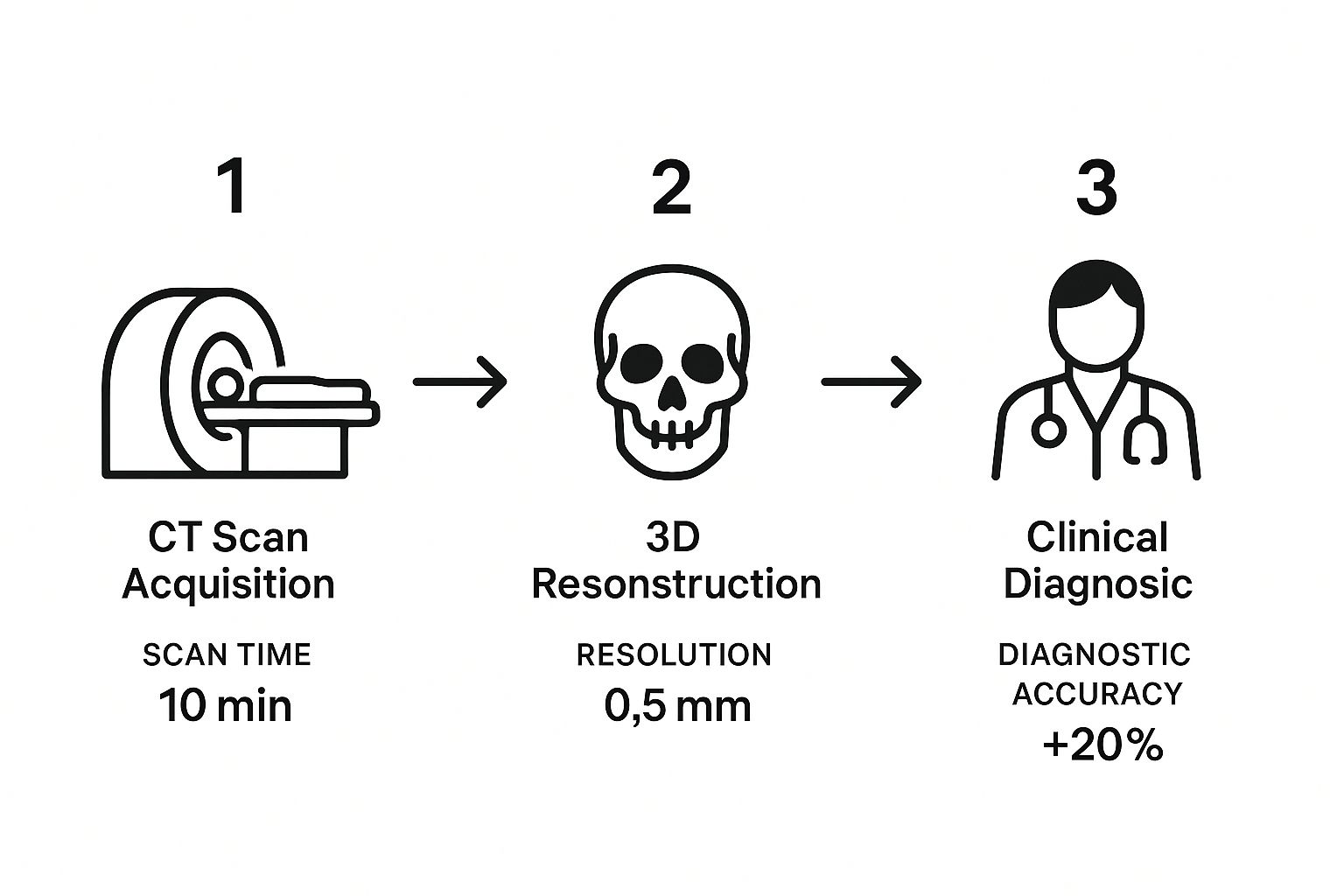
As you can see, while the scan itself is fast, the reconstruction and analysis are where the magic happens, turning those images into accurate, actionable insights.
Stage 3: Segmentation
This is where human skill really comes into play and is often the most hands-on part of the entire process. Segmentation is the art of identifying and isolating specific anatomical structures within the stack of 2D images.
Imagine digitally "coloring in" the parts you care about on each slice—this is bone, this is muscle, this is the tumor we need to examine. A radiologist or a highly trained technologist uses specialized software to painstakingly trace the boundaries of organs, blood vessels, or pathologies. While AI is making this step faster, an expert's anatomical knowledge is still the gold standard for ensuring precision.
Stage 4: 3D Rendering and Post-Processing
With our key structures now cleanly segmented, the software takes over for the final act: rendering. Using powerful algorithms like Volume Rendering, the system stacks all the segmented 2D slices on top of each other and intelligently "connects the dots" to build the final, interactive 3D model.
But it doesn't stop there. In the post-processing phase, clinicians can finally interact with the model. This is where the true clinical value of computed tomography 3d reconstruction shines. They can:
- Manipulate the view: Freely rotate, pan, and zoom to inspect anatomy from any conceivable angle.
- Take precise measurements: Calculate volumes, distances, and angles with incredible accuracy.
- Simulate procedures: Plan complex surgical approaches or virtually place a medical implant to check its fit.
It's easy to take this for granted now, but the computing power required for these tasks used to be a massive hurdle. Back in 1987, it could take a powerful computer over 24 hours just to reconstruct 50-60 CT slices. The introduction of machines like the Pixar Image Computer in the mid-1980s was a huge leap, but we've come an incredibly long way since then. You can learn more about the history of CT processing power to see just how much the technology has evolved.
How AI Is Making 3D Reconstruction Smarter and Safer

The worlds of artificial intelligence and computed tomography 3D reconstruction are colliding, and it's changing the game in medical imaging. Instead of replacing radiologists, AI is stepping in as an incredibly capable co-pilot. It handles the repetitive, time-consuming tasks and uncovers subtle details that might otherwise go unnoticed, making the entire diagnostic process quicker, more precise, and safer for patients.
Take segmentation, for instance. This is the painstaking process where a clinician has to manually trace anatomical structures, slice by agonizing slice. It’s absolutely essential for an accurate diagnosis, but it’s also a significant bottleneck in any busy radiology department. Now, AI algorithms, trained on vast libraries of scans, can do the same job with incredible accuracy in just minutes or even seconds.
This frees up highly trained specialists to do what they do best: interpret complex cases, collaborate with surgeons, and plan treatments, rather than getting bogged down in manual tracing.
Enhancing Images and Reducing Radiation
Perhaps one of AI's most significant contributions is its ability to clean up images from low-dose CT scans. For years, clinicians faced a difficult choice: lower the radiation dose and risk getting a "noisy" image that's harder to read, or use a higher dose to get a crystal-clear picture.
AI-powered deep learning models have completely changed this equation. By studying countless low-dose scans, they've learned to identify and intelligently eliminate the image noise, resulting in a sharp, detailed reconstruction. They essentially restore the image quality without losing any crucial anatomical information.
Think of AI as a sophisticated noise-cancellation filter for medical images. It lets us capture scans with significantly less radiation but cleans them up to look as sharp as a high-dose image. It’s a huge win for patient safety.
This breakthrough allows hospitals and clinics to adopt safer scanning practices across the board, all without sacrificing the diagnostic quality of their computed tomography 3D reconstruction models.
Boosting Precision and Predicting Outcomes
Beyond just making things faster, AI brings a powerful new analytical depth to 3D models. It's not just about seeing structures; it's about understanding them in a way that wasn't possible before. This is especially evident in complex fields like thoracic surgery.
-
Smarter Surgical Planning: Research shows that AI assistance helps surgeons pinpoint lesions and map out tricky networks of pulmonary arteries and veins with greater accuracy. In some studies, the insights from AI-driven models led surgeons to opt for a less invasive, lung-sparing segmentectomy instead of a more drastic lobectomy.
-
Predictive Analytics: AI is exceptionally good at detecting subtle patterns in imaging data that escape the human eye. By analyzing a tumor's texture, volume, and shape from a 3D model, these algorithms can help forecast a patient's risk of recurrence, giving clinicians a powerful new data point for tailoring treatment plans.
-
Faster Reconstruction: The time savings are dramatic. Manually creating a detailed 3D model is a slow process. AI has been shown to reduce the reconstruction time from a typical 30 minutes down to just 5 minutes.
This shift toward AI-driven analysis is making medicine more personalized and precise. We're moving from just looking at pictures to extracting predictive, actionable intelligence from them. To learn more about how artificial intelligence is being applied across different industries, the AI Tools Brief blog is a great resource. Ultimately, this technology isn't just about efficiency; it's about elevating the standard of care.
Seeing the Impact in Real-World Clinical Scenarios
While the technology behind computed tomography 3D reconstruction is impressive, its real power is unlocked in the clinic. This is where abstract data becomes a tangible tool that helps doctors make better decisions and ultimately improves a patient's chances for a good outcome. It’s in these moments that we see a stack of 2D slices truly transform into a life-saving instrument.
These detailed 3D models are much more than just fancy pictures. They offer an intuitive, crystal-clear map of a patient's individual anatomy, giving doctors a degree of confidence in diagnosis and surgical planning that was once hard to come by. Across many medical fields, this approach is making complex procedures safer and far more precise.
Oncology: A Surgeon's Blueprint
In cancer treatment, every millimeter counts. Imagine a surgeon getting ready to remove a tricky tumor lodged deep inside a patient's chest. Using standard 2D scans, they have to mentally reconstruct the tumor’s position in relation to critical structures like the pulmonary arteries and veins. It's a high-stakes puzzle where a small miscalculation can have big consequences.
Now, give that same surgeon a 3D model. They can spin it around, peel back layers, and see the tumor’s exact relationship with the surrounding blood vessels. This digital blueprint enables meticulous planning, often making it possible to save more healthy lung tissue.
Research has shown that when surgeons use AI-assisted 3D models for preoperative planning, they can more accurately localize lesions. In some cases, this superior view has allowed surgeons to change their approach from a more invasive lobectomy to a lung-sparing segmentectomy, directly improving patient outcomes.
Orthopedics: Custom Solutions for Complex Fractures
Orthopedics is another area where this technology shines. When a surgeon is faced with a complex fracture, like a shattered joint, a 3D reconstruction shows them the precise size and placement of every single bone fragment. This clear visualization is incredibly valuable when planning how to piece everything back together.
It gets even better. These models allow for the virtual pre-fitting of custom implants. Surgeons can test out different screws and plates on the 3D model, making sure they have a perfect fit before the patient is even on the operating table. This saves a huge amount of time during the actual surgery and often leads to a much better recovery for the patient.
Cardiology: Navigating the Arteries
For cardiologists, computed tomography 3D reconstruction is key to planning minimally invasive procedures. When a patient has a blocked coronary artery and needs a stent, a 3D model provides a detailed road map of their specific arterial network.
Doctors can use the model to pinpoint the exact location and severity of the blockage. This helps them select the right-sized stent and chart the best path to deploy it, reducing risks and boosting the chances of a successful procedure. These everyday applications show how the clarity from 3D reconstruction makes a profound difference in patient care.
Your Questions About 3D CT Reconstruction, Answered
As 3D reconstructions from CT scans become a bigger part of modern medicine, it's only natural for patients and even medical professionals to have questions. Let's clear up some of the most common ones.
Think of this as a straightforward guide to help you understand the what, when, and how of this powerful imaging technology.
Is 3D Reconstruction Part of Every CT Scan?
Not at all. A computed tomography 3D reconstruction isn't an automatic part of every scan. It's an extra step, a special tool pulled out of the toolbox only when a doctor needs a deeper, more dimensional look at something specific.
So, when is it ordered? A radiologist or your doctor will request one for a few key reasons:
- Complex Cases: Sometimes, standard 2D slices just can't show the whole picture, especially when dealing with complicated anatomy or injuries.
- Surgical Planning: A surgeon planning a delicate procedure, like removing a tumor or performing a joint replacement, needs a detailed 3D map to navigate.
- Patient Communication: It’s often much easier to understand a medical condition or a proposed surgery when you can see it in 3D, rather than trying to interpret flat, black-and-white images.
In short, it’s used when the standard view isn't quite enough to get the job done.
Does 3D Reconstruction Require More Radiation?
This is a great question, and the answer is mostly no. The actual process of building the 3D model happens on a computer after your scan is complete. It uses the data that was already gathered, so creating the model itself adds zero extra radiation exposure. You're long gone from the scanner by then!
Now, there is a small catch. If the medical team knows from the get-go that they'll need a high-quality 3D model, the technician might adjust the initial scan settings. They might capture thinner image "slices" to get more detail. This can sometimes lead to a slightly higher radiation dose for that specific scan, but it's a calculated decision made to ensure the final 3D model is as accurate and useful as possible.
How Long Does It Take to Create a 3D Model?
The time it takes can be anywhere from a few minutes to a few hours. With today's powerful computers, the automated part—where the software stitches the 2D slices into a 3D shape—is incredibly fast.
The real variable is the human element. The most time-consuming step is often segmentation, which involves a skilled technologist manually tracing the exact outlines of complex organs or tumors. This meticulous work is what ensures the final model is clinically precise.
This is where AI is making a huge difference. For example, some studies have shown that AI can slash the time for this manual work from a painstaking 30 minutes down to just 5 minutes, which is a massive leap forward for busy clinics.
At PYCAD, we focus on building AI-powered tools that make medical imaging faster and more accurate. From managing data to deploying custom models, we help medical device companies and healthcare providers bring advanced AI into their daily work. Learn more about how we can help you at https://pycad.co.






