Understanding Data Interoperability Healthcare Fundamentals
Imagine walking into any clinic, and your complete medical history is instantly available to the doctor. No more filling out the same forms, recounting your health story, or worrying that a crucial piece of information is missing. This is the simple but powerful promise of data interoperability in healthcare. At its heart, it acts like a universal translator for medical information, allowing different hospital systems, clinics, and healthcare apps to speak the same language. This fluid communication is more than a technical convenience; it’s about building a connected care system that puts you, the patient, first.
The idea of healthcare data interoperability is built on three distinct but connected layers. Each one is essential to ensuring that data isn't just moved from one place to another but is also understood and usable across different healthcare environments.
The Three Layers of Interoperability
To really see how this works, let's break down the foundational layers:
- Technical Interoperability: This is the base layer, like the digital plumbing that connects different systems. It sets the rules for how data packets are sent between applications and networks. Think of it as making sure the electrical plug from one country fits the outlet in another. Without this basic connection, no information can flow.
- Semantic Interoperability: Once systems are connected, they must understand each other. This layer ensures the meaning of the data is consistent. For instance, when one system sends a patient's "blood pressure," the receiving system knows it means blood pressure, including the units (mmHg) and context (systolic/diastolic). It’s about having a shared dictionary and context to prevent dangerous mix-ups.
- Organizational Interoperability: This final layer handles the human and policy side of things. It involves creating the governance, rules, and workflows that let different organizations share data securely and legally. It answers questions like: Who can access what data? And for what reason? This requires trust, legal agreements, and aligned business practices among healthcare groups. A key part of achieving this is through solid system integrations, which often call for specialized integration services to connect the dots between diverse organizational setups.
This diagram shows how Health Information Exchanges (HIEs) enable this multi-layered communication between various healthcare providers.

As illustrated, the HIE is the central point that allows entities like hospitals, labs, and pharmacies to share patient information securely, which supports all three layers of interoperability. A 2019 survey found that 92% of hospitals and 69% of physician offices were part of these networks, showing a significant shift toward connected care. Ultimately, effective data interoperability in healthcare means mastering all three layers to create a system where a patient's information follows them smoothly, ensuring safer, more efficient, and better-coordinated care no matter where they go. This foundational knowledge paves the way for a deeper look into the specific market forces driving this change.
The Healthcare Data Revolution: Market Forces Driving Change
The drive for data interoperability in healthcare is no longer just a technical wish—it's a full-blown market movement. A powerful mix of economic and social pressures is forcing healthcare organizations to tear down their data silos. What once seemed like an optional upgrade is now a must-have for staying relevant and competitive. These forces aren't abstract; they are real-world pressures impacting daily operations, financial stability, and patient care everywhere.
A major catalyst is the shift from fee-for-service to value-based care. In this new model, providers get paid for positive patient outcomes, not just the volume of services rendered. This approach is unworkable without a complete picture of a patient's health journey. For instance, a hospital needs to know if a patient saw their primary doctor after discharge to avoid a costly readmission. Without connected data, providers are essentially working in the dark, unable to coordinate care or prove their effectiveness.
Financial and Patient-Driven Imperatives
Beyond new payment structures, the financial reasons to connect systems are massive. Inefficiencies caused by disconnected data lead to significant monetary losses, from ordering duplicate lab tests to administrative bloat. The need for financial improvement is a key part of the healthcare data revolution, as shown by instances of AI-powered cameras helping hospitals recover millions in missed charges. This economic reality is a strong motivator for adopting integrated data systems.
At the same time, patient expectations have completely changed. People are used to seamless digital experiences in banking and retail, and they now demand the same from healthcare. This growing consumer pressure includes:
- Easy access to their personal health records.
- Smooth communication between their different specialists.
- The ability to integrate data from their personal fitness trackers and health apps.
Healthcare providers that can't deliver on these expectations risk losing patients to more modern competitors. This consumer demand makes interoperability a central feature of their service.
This momentum is clearly visible in the market's rapid growth. The global health data interoperability market was valued at around USD 84.58 billion in 2025 and is expected to climb to USD 352.13 billion by 2032. This reflects a compound annual growth rate (CAGR) of 22.65%, showing the immense investment and effort being directed toward building a truly connected healthcare system. You can read more about these trends in a detailed industry report about health data interoperability from Coherent Market Insights. These market forces are not just influencing the industry; they are creating the demand for the specific standards needed to make this data exchange possible.
Mastering Healthcare Standards: FHIR, HL7, And DICOM Decoded
For healthcare data to move freely and effectively between systems, they need more than a simple connection; they require a shared language. This is where data standards come into play, acting as the universal rulebooks that allow different systems to communicate without error. Think of them as the grammar and vocabulary that prevent critical information from being lost in translation. Without these standards, one hospital's electronic health record (EHR) would send digital nonsense to another.
The following diagram breaks down the main focus of the three most important standards in healthcare today.
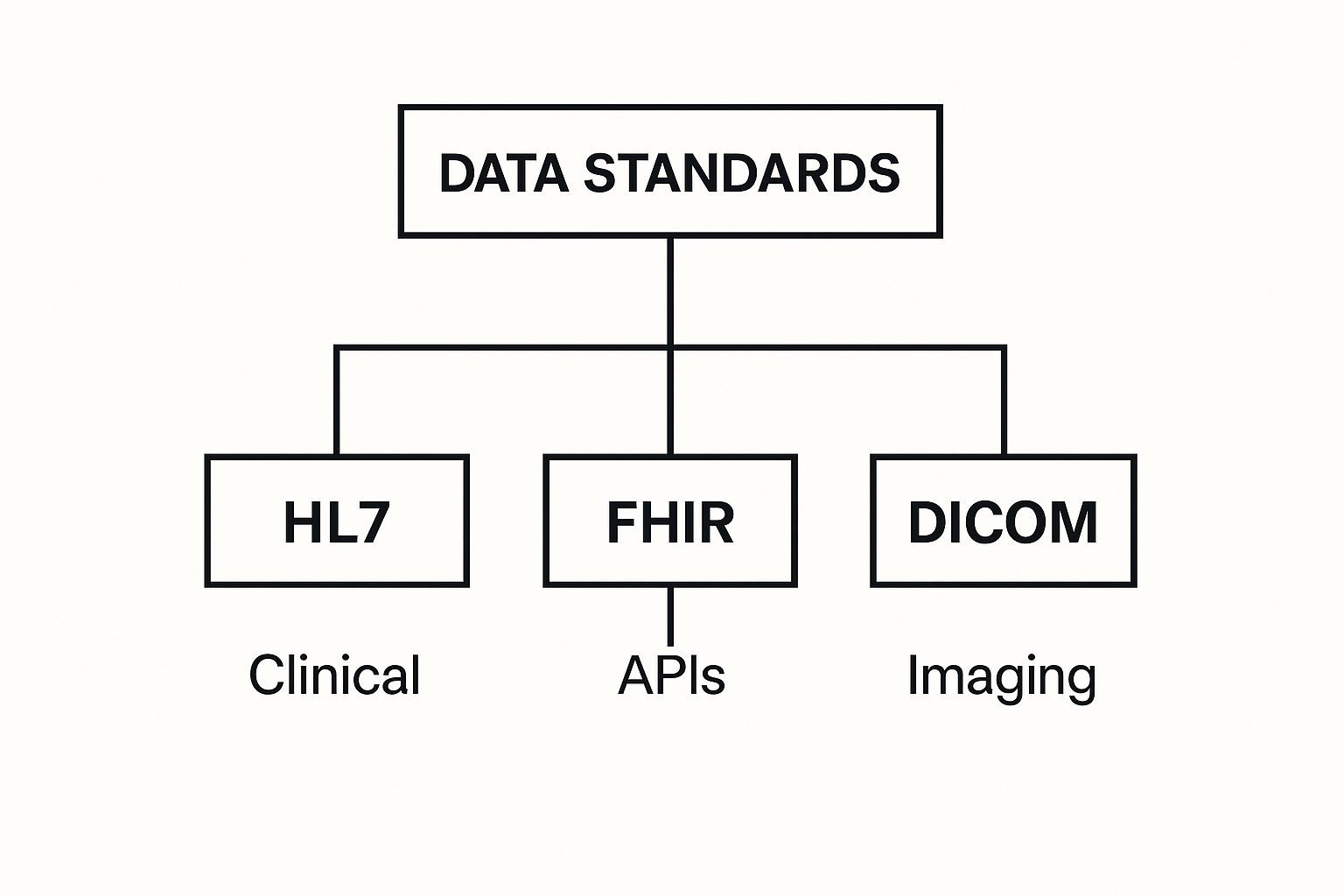
This visual shows how each standard governs a specific yet essential area of healthcare data, working together to build a connected information network.
HL7: The Foundation for Clinical Data
For many years, Health Level Seven (HL7) has been the dependable engine for clinical data exchange. Imagine HL7 as the formal, established grammar for healthcare messages. It sets the structure for communicating events like patient admissions, lab orders, and billing information. HL7 Version 2 (V2) is especially common, functioning as the behind-the-scenes operator that makes sure a patient admitted in the ER is correctly registered in the hospital's main system.
While very reliable, older HL7 versions can be rigid. Working with them can feel like trying to assemble a complex piece of furniture with a very dense instruction manual.
DICOM: The Standard for Medical Imaging
While HL7 manages text-based clinical data, Digital Imaging and Communications in Medicine (DICOM) is the global standard for medical images. It's the reason a CT scan taken at one clinic can be viewed and analyzed perfectly by a specialist using different equipment miles away. DICOM does more than just store the image; it bundles vital metadata with it, such as:
- Patient identification details
- The type of scan performed
- Date and time of the study
This process ensures the image always travels with its full context, preventing dangerous mix-ups. For any company working in medical imaging, like PYCAD, a deep understanding of DICOM is essential for building tools that fit into clinical workflows.
FHIR: The Modern Approach to Data Exchange
The newest and most flexible standard is Fast Healthcare Interoperability Resources (FHIR). If HL7 V2 is the detailed instruction manual, FHIR is the modern, developer-friendly API that powers today’s mobile health apps. It uses the same web technologies as popular sites like Google and Facebook, making it much easier for developers to work with.
FHIR breaks down complex medical records into manageable "resources"—like a single patient profile, a specific allergy, or a lab result. This modular structure allows an application to request only the specific piece of data it needs, rather than an entire bulky document. This efficiency is why an estimated 90% of health systems are expected to adopt FHIR APIs by 2025, paving the way for the next generation of connected healthcare.
To help clarify the roles of these key standards, the table below offers a direct comparison of their primary functions, complexity, and adoption.
Healthcare Interoperability Standards Comparison Guide
Essential comparison of FHIR, HL7, DICOM, and emerging standards showing their real-world applications, implementation complexity, and adoption patterns
| Standard | Primary Use Case | Data Types | Implementation Complexity | Adoption Rate | Key Benefits |
|---|---|---|---|---|---|
| HL7 V2 | Clinical & administrative data exchange (admissions, orders, results). | Text-based, segment-delimited messages. | High | Very High (Legacy) | Widespread industry support; reliable for core hospital operations. |
| DICOM | Medical imaging storage, transmission, and printing. | Images (CT, MRI, X-ray) and associated metadata. | Moderate | Universal (in Imaging) | Global standard for all imaging modalities; ensures image quality and context. |
| FHIR | Real-time data access via web APIs for modern applications. | Modular "resources" (Patient, Observation, etc.) using JSON/XML. | Low to Moderate | Rapidly Growing | Developer-friendly, flexible, supports mobile and web apps, cost-effective. |
| IHE | Process and workflow integration across systems. | Profiles that use other standards like DICOM and HL7. | High | Moderate | Standardizes entire clinical workflows, not just data points. |
This table shows that while older standards like HL7 V2 and DICOM remain critical for their specific domains, FHIR is rapidly becoming the standard for modern, agile data exchange. Each standard plays a distinct but complementary role in achieving true interoperability.
The FHIR Revolution: Modern APIs Transforming Healthcare
While older standards like HL7 and DICOM laid the groundwork for exchanging data, Fast Healthcare Interoperability Resources (FHIR) is the engine driving a new era of connectivity. Think about the difference between sending a fax and using a real-time messaging app on your phone. That’s the kind of jump FHIR provides. It uses modern web-based APIs—the same technology behind your social media feed and mobile banking—to make medical information accessible, secure, and instantly shareable.
This approach is fundamentally changing how healthcare systems communicate.
This fresh take on data interoperability in healthcare centers on the idea of "resources." Instead of trading heavy, complex documents, FHIR breaks down medical information into smaller, logical units. A "patient" is one resource, a specific "medication order" is another, and a "lab result" is a third. This modular structure means a doctor's mobile app can request just the latest blood sugar reading for a diabetic patient without downloading their entire medical record. This efficiency is critical for building responsive and truly helpful healthcare applications.
Real-World Applications of FHIR
The practical effects of FHIR are already being felt across the healthcare system. Organizations are using it to create tools that were once too complex to build, simplifying workflows that used to depend on hours of manual work and phone calls.
Here are a few clear examples of FHIR in action:
- Functional Patient Portals: Patients can finally view their own lab results, book appointments, and talk to their care team through portals that actually work. FHIR APIs pull specific, current information from the EHR in real time to make this possible.
- Provider-to-Provider Data Sharing: A specialist can instantly pull up a referred patient's relevant history, allergies, and current medications directly within their own system. This improves diagnostic accuracy and patient safety from the very first visit.
- Support for New Health Apps: App developers can build tools that connect securely to hospital systems, allowing patients to manage chronic conditions, monitor their wellness, or share data from wearable devices with their doctors.
The Inevitable Shift to FHIR
This move toward API-driven data sharing isn't just a fleeting trend; it's the direction the entire industry is headed. The speed and flexibility offered by FHIR are so compelling that its adoption is picking up pace worldwide. Industry analysis suggests that 90% of health systems globally will have adopted FHIR APIs by 2025, confirming its position as the new standard for connected care.
This widespread integration is a core piece of achieving universal data interoperability healthcare. You can dive deeper into expert predictions about the future of FHIR API adoption on ottehr.com. This massive uptake shows that forward-thinking healthcare organizations are building their digital strategies around FHIR-based solutions, seeing it as the essential link to a more connected and efficient future.
Conquering Implementation Challenges: Real Solutions For Real Problems
Achieving data interoperability in healthcare is like conducting a complex orchestra. Every instrument, from old legacy systems to modern APIs, must play in perfect harmony. While the goal is clear—seamless data flow—the path is often filled with predictable hurdles. Organizations frequently grapple with technical and organizational barriers that can stop progress in its tracks. Successfully navigating these requires a sharp understanding of the problems and a commitment to practical solutions.
The challenges are not just about technology. They involve people, processes, and the very culture of an organization. By anticipating these issues, healthcare leaders can build a strategy that addresses them head-on, turning potential roadblocks into stepping stones for success.
Tackling Technical Hurdles
The technical side of implementation often feels like wrestling with a tangled web of systems. Many organizations rely on decades-old legacy platforms that were never built to share data. Connecting these dinosaurs to modern, API-driven platforms is a significant challenge.
A common pain point is data mapping, which is the process of matching fields between two different systems. Think of it as translating between two languages where a single mistake can change the entire meaning. A small error here—like confusing different units of measurement for a lab result—can have major clinical consequences.
Beyond mapping, other technical issues include:
- API Performance: New interoperability solutions must be fast. An API that takes too long to respond can disrupt a clinician's workflow, making it more of a hindrance than a help. Optimizing these connections for speed and reliability is crucial.
- Security Implementation: Security can't be an afterthought. Implementing strong authentication and authorization without slowing down data access is a delicate balance. The goal is to make data sharing both easy and secure. According to one study, data breaches cost the healthcare industry an average of $10.93 million per incident, which shows why getting security right is non-negotiable.
- Data Quality: Inconsistent, incomplete, or inaccurate data entering the system can derail an entire project. This "garbage in, garbage out" problem undermines trust and can lead to poor clinical decisions. Establishing strong data validation rules from the start is essential.
Overcoming Organizational Barriers
Often more difficult than any technical problem are the organizational and human barriers. Technology can be fixed, but changing workflows and mindsets requires careful planning and strong leadership.
A successful implementation depends on managing the human element effectively. This means addressing concerns and building support from the ground up. Key strategies include:
- Managing Workflow Disruption: New systems inevitably change how people do their jobs. It's vital to involve clinical staff early in the design process to ensure the new workflows are intuitive and actually improve their daily tasks, rather than adding complexity.
- Building Staff Buy-In: People resist change when the "why" isn't clear. Leaders must consistently communicate the benefits of interoperability—better patient outcomes, less administrative work, and improved safety—to get everyone on board.
- Establishing Data Governance: Creating clear rules for data ownership, access, and stewardship is critical. A strong governance framework ensures that as data flows between departments and organizations, it remains accurate, secure, and used appropriately. This turns a potentially chaotic implementation into a well-managed process.
To help you navigate these obstacles, we've put together a table that outlines common challenges and practical solutions.
| Challenge Category | Specific Challenge | Impact Level | Recommended Solution | Implementation Time | Success Rate |
|---|---|---|---|---|---|
| Technical | Integrating with Legacy Systems | High | Use a data integration middleware or platform that acts as a translator between old and new systems. Create data wrappers for legacy databases. | 6-12 Months | 80% |
| Technical | Ensuring Data Quality & Consistency | High | Implement automated data validation rules at the point of entry. Establish a master data management (MDM) strategy. | 4-8 Months | 85% |
| Technical | API Performance & Scalability | Medium | Load-test APIs before deployment. Use API gateways for traffic management and caching. Optimize database queries. | 2-4 Months | 90% |
| Organizational | Lack of Staff Buy-In & Resistance | High | Involve clinicians and staff in the design process. Create "super-user" champions to promote adoption. Clearly communicate benefits. | Ongoing | 70% |
| Organizational | Vague Data Governance | High | Form a multi-disciplinary data governance committee. Define clear policies for data ownership, access control, and security. | 3-6 Months | 95% |
| Organizational | Workflow Disruption for Clinicians | Medium | Map existing workflows and design new ones with clinical input. Provide extensive hands-on training and at-the-elbow support during rollout. | 4-6 Months | 75% |
This table highlights that while technical issues require significant effort, organizational barriers often demand a more sustained, people-focused approach. The most successful interoperability projects address both sides of the coin with equal seriousness.
Success Stories: Healthcare Organizations Getting It Right
The ideas behind data interoperability in healthcare feel more real when we look at organizations that have tackled the challenges and achieved remarkable outcomes. These aren't just theories; they're stories from real-world healthcare systems that transformed data-sharing headaches into strategic wins. They show how focused interoperability work leads directly to better patient care and more efficient operations.

Reducing Waste and Improving Safety
One of the clearest benefits of connected data is slashing redundant and expensive procedures. Imagine a large health system struggling with duplicate tests. Patients moving between its hospitals and clinics often had the same lab work and imaging scans done repeatedly because providers couldn't access prior results. This was not only wasteful but also exposed patients to needless radiation and stress.
To address this, the organization created a central data hub using HL7 and FHIR standards. This system provided clinicians with a complete view of a patient's diagnostic history, no matter where the first test was conducted.
- The Strategy: They built an enterprise master patient index (eMPI) to correctly link records. Then, they used FHIR APIs to pull recent test results directly into the clinician's electronic health record.
- The Result: In just 18 months, the health system reported a 40% drop in duplicate imaging tests. This saved millions of dollars and boosted patient safety by cutting down on unnecessary procedures. The success proves how technical standards can produce real financial and clinical benefits.
A New Approach to Chronic Disease Management
Managing chronic conditions like diabetes or heart disease requires constant, coordinated care from a team of providers. A regional healthcare network faced this problem head-on. Their primary care doctors, cardiologists, and endocrinologists all used different EHR systems, which resulted in disjointed care and poor patient outcomes. Information was stuck in separate systems, making proactive health management almost impossible.
Their answer was to launch a Health Information Exchange (HIE) that connected every provider on a single, shared platform. This allowed crucial data points—like blood sugar levels, medication adjustments, and specialist notes—to flow freely.
- The Approach: They focused on semantic interoperability, making sure that a "medication list" from one system meant the same thing to every other system. They also introduced a patient portal, letting people upload data from their home monitoring devices.
- The Outcome: The network achieved a 15% improvement in key quality metrics for patients with diabetes, including better A1c control. Giving the entire care team—and the patient—access to the same timely data enabled faster interventions and more personalized treatment plans.
Creating Frictionless Referrals in Specialty Care
The handover from a primary care physician to a specialist is often where things break down in healthcare. An orthopedic specialty clinic noticed that incomplete patient information from referring doctors was causing treatment delays and unhappy patients. Clinic staff would spend hours on the phone hunting down medical histories, imaging reports, and lab results.
To solve this, the clinic collaborated with its main referring practices to set up a direct, secure data connection using DICOM for images and FHIR for clinical summaries.
- The Implementation: They offered their referral partners a simple, secure web portal to upload all necessary documents and images before the patient's first visit.
- The Benefit: This straightforward adjustment greatly improved efficiency, cutting patient intake time by an average of 20 minutes for each new visit. More importantly, specialists had a full understanding of the patient's situation from the beginning, resulting in better-informed consultations and treatment strategies. This example highlights how even targeted interoperability projects can fix specific operational issues and improve the patient experience right away.
The Future of Healthcare Data: Emerging Trends and Technologies
The path to healthcare data interoperability is evolving. It's moving beyond the simple goal of sharing a patient record between two hospitals. We're now building a connected ecosystem where artificial intelligence (AI), blockchain, and the Internet of Medical Things (IoMT) work together. This creates a more intelligent, secure, and predictive healthcare environment. Imagine a world where AI actively helps manage data and a smartwatch's health readings become a core part of a patient's clinical chart.
AI and Automation in Data Exchange
Artificial intelligence is becoming the new foundation for interoperability. Instead of requiring people to manually map data, AI-driven systems can automatically spot and fix inconsistencies between different data formats. For instance, AI can use natural language processing (NLP) to scan a doctor's unstructured clinical notes—the detailed narratives where they record observations—and transform them into structured, searchable information. This makes a huge amount of previously locked-away data usable.
The image below shows several key areas where AI is making a real difference in healthcare.
This diagram highlights how AI's reach extends from diagnostics to administrative functions, all of which rely on access to high-quality, interoperable data. These technologies aren't just improving what we already do; they are creating entirely new ways to deliver care and conduct research.
Blockchain and IoMT Integration
Alongside AI, other technologies are making the data-sharing framework stronger:
- Blockchain for Data Integrity: Picture blockchain as a secure, unchangeable digital logbook. In healthcare, it can create a clear audit trail for every time a patient's record is viewed or changed. This adds a powerful layer of security and transparency, making sure data remains trustworthy across different hospital networks.
- Internet of Medical Things (IoMT): The growing number of connected devices, like continuous glucose monitors and smart inhalers, produces a constant flow of health data. Real interoperability means bringing this patient-generated health data directly into the electronic health record (EHR). This gives doctors a much fuller, real-time picture of a patient's health between appointments.
This technological shift is attracting major market investment. The healthcare data interoperability market, valued at USD 6.23 billion in 2024, is expected to reach USD 14.06 billion by 2029. This reflects a robust compound annual growth rate (CAGR) of 17.6%. You can explore the complete study on global market projections for healthcare data interoperability. This growth highlights the industry's dedication to building these advanced, interconnected systems. From AI-guided diagnostics to blockchain-secured records, these trends are fundamentally altering what's possible in patient care.
Your Interoperability Action Plan: From Vision to Implementation
Understanding the concepts behind data interoperability in healthcare is one thing, but translating that knowledge into a working plan is where progress truly starts. This section is a practical guide for healthcare leaders who are ready to move from vision to reality. It’s about taking structured, deliberate steps to build interoperable systems that produce real results. An effective plan begins with an honest look at where your organization stands today.
Assess Your Starting Point
Before you can chart a course to your destination, you need to know your exact location. A maturity model is an excellent tool for this self-assessment. It helps you grade your organization’s current state across several key areas, like technical infrastructure, data governance, and staff skills. The goal isn’t to find faults; it’s to identify your strengths and pinpoint the most logical places to begin your efforts.
You can use a simple framework to score your organization on a scale of 1 to 5 in these domains:
- Technical Infrastructure: Do you have modern systems ready for API integration, or are you mostly working with older, legacy platforms?
- Data Standards Adoption: Are your teams comfortable with FHIR, HL7, and DICOM, or is this knowledge limited to only a few people?
- Data Governance: Are there clear policies for data ownership, security, and quality control? A successful interoperability plan requires implementing a robust data governance framework to maintain data quality and compliance.
- Clinical Workflow Integration: How smoothly do your data systems support the daily jobs of your clinicians?
This baseline gives you the clarity needed to create a realistic and phased implementation strategy.
Build a Phased Implementation Roadmap
Attempting to achieve total interoperability in one giant leap is often a recipe for frustration. A phased approach, however, lets you secure early victories, which builds momentum and shows value to stakeholders. Your roadmap should break down the larger goal into a series of manageable projects.
Here is a sample phased approach:
- Phase 1: Foundational Wins (First 6 Months): Start by tackling a single, high-impact problem. For example, focus on automating the exchange of lab results between your inpatient and outpatient clinics. This is a contained project that offers immediate benefits to both clinicians and patients.
- Phase 2: Expanding Connections (Months 7-18): Widen your scope. Connect with one or two key external partners, like a major referring physician group or a regional imaging center. This phase puts your ability to share data outside your organization’s walls to the test.
- Phase 3: Scaling for Enterprise-Wide Value (Months 19+): With proven successes under your belt, you can now make the case for bigger, enterprise-level initiatives. This might involve joining a regional Health Information Exchange (HIE) or creating a patient-facing app using FHIR APIs.
This step-by-step method reduces disruption and gives your team the chance to learn and adjust as you progress. By concentrating on specific actions and measurable outcomes, you can steadily advance your data interoperability healthcare goals, improving organizational efficiency and patient care one project at a time.
For organizations that focus on medical imaging, making sure your systems communicate fluently with hospital networks is essential. PYCAD’s AI-powered solutions are built with interoperability at their foundation, fitting into existing clinical workflows using standards like DICOM and FHIR. To see how our expertise can accelerate your action plan, visit us at pycad.co.