Understanding Clinical Trial Data Management Without the Complexity
Imagine trying to conduct a world-class orchestra. Each instrument, note, and timing cue must work together in perfect harmony to create something exceptional. This is a great way to think about data management for clinical trials. While it’s easy to get lost in technical systems and regulatory checkboxes, the real work is about people, processes, and cutting through complexity to move a study forward. It’s about building a foundation of data integrity that the entire research project can stand on.
This foundational work is more crucial than ever. The clinical data management services (CDMS) market is a key part of how new pharmaceuticals and medical devices are developed. There are over 450,000 clinical trials registered worldwide, a number expected to grow by about 5.7% each year through 2030. This explosive growth means the demand for solid data handling has never been greater.
The Real-World Data Journey
Let's set aside the textbook definitions and talk about what experienced data managers wish they knew on day one. At its core, data management is the structured path that information follows, from a patient's first clinic visit to the final, clean dataset ready for analysis.
This journey is made up of several key activities:
- Data Collection: This is where the story begins, capturing information accurately at the source. It could be through electronic Case Report Forms (eCRFs) on a tablet in a clinic or from patient-reported outcomes entered on a smartphone at home.
- Data Entry & Integration: Next, all that information is moved into a central database. This step often means combining data from different places, like lab results, imaging systems, and even wearable devices.
- Data Validation & Cleaning: Here’s where the detective work happens. The team systematically checks for errors, inconsistencies, or missing values to ensure the data is logical, consistent, and reliable.
- Database Lock: This is the final, decisive moment. The dataset is declared complete and "locked" to prevent any more changes, making it ready for statisticians to analyze.
The screenshot above, from ClinicalTrials.gov, gives you a sense of the immense public registry of trials. Each one of those entries represents a massive data management effort, highlighting just how much we need standardized, efficient processes to manage all this information.
From Chaos to Cohesion
Not too long ago, many of these processes were manual and done on paper, which led to big delays and a high chance of errors. Today, the focus has shifted to digital workflows. The heart of effective clinical trial data management is a deep understanding of automated data processing. This simply means using technology to handle repetitive tasks, enforce data standards, and give teams real-time updates.
The goal isn't just to collect data, but to turn it into trustworthy evidence. By getting these fundamentals right, research teams can move away from operational chaos and build a cohesive system that supports faster, more accurate clinical research.
Why Smart Teams Are Embracing Risk-Based Quality Management
Imagine you're in charge of inspecting a massive aircraft before takeoff. One way is to check every single component, from the seat cushions to the snack trays to the engine bolts. A smarter approach is to focus intense scrutiny on the systems critical for a safe flight: the engine, the wings, and the navigation equipment. This is precisely the change happening in data management for clinical trials through Risk-Based Quality Management (RBQM).
The old method of questioning every data point and documenting every minor detail isn't just inefficient; it can hide important safety signals in a flood of trivial information. Leading organizations are finding that a targeted approach delivers better results with fewer resources. Instead of treating all data as equally important, RBQM focuses on data and processes that are most critical to patient safety and the study's integrity. This allows teams to direct their energy where it has the most impact.
The Shift From Volume to Value
The central idea behind RBQM is that not all risks are created equal. A typo in a non-essential field might have a tiny impact. However, an incorrect dosage record or an unreported adverse event could threaten patient well-being and the entire study. A risk-based strategy identifies these high-stakes areas early on and builds a monitoring plan to protect them.
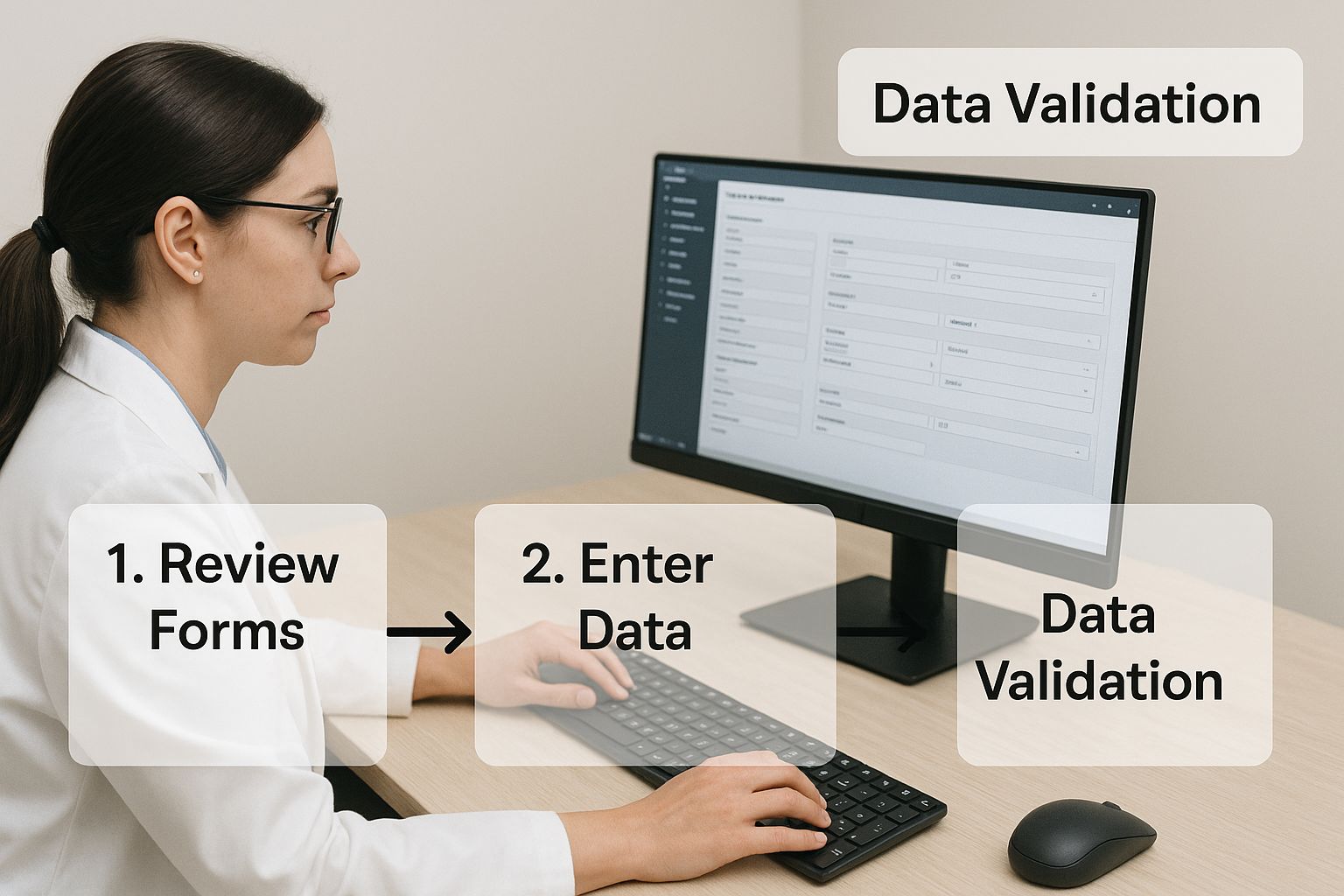
This focus on what matters is especially clear in data validation, a core process in any trial. The infographic below shows how data validation fits into the larger data management workflow, highlighting its importance.
By concentrating validation on critical data, teams ensure the most important information is accurate without getting stuck on minor issues. This strategic focus is a pillar of effective RBQM.
This isn't just a new idea; it's a major trend shaping the industry. A 2024 survey of 156 clinical data leaders in hubs like New York and London found that risk-based methods were seen as having the highest probability of success and value over the next two years. For more details on this shift, you can explore the full report on evolving clinical data trends.
To better understand the practical differences, let's compare the traditional method with the risk-based approach.
| Aspect | Traditional Approach | Risk-Based Approach | Impact |
|---|---|---|---|
| Verification Strategy | 100% Source Data Verification (SDV) for all data points. | Targeted SDV focusing on critical data and primary endpoints. | Resources are redirected to high-risk areas, improving efficiency and focus. |
| Data Review | All data is treated with equal importance, leading to high query volume. | Data is prioritized based on its impact on patient safety and trial integrity. | Reduces noise from trivial queries, making critical signals easier to detect. |
| Monitoring | Primarily on-site monitoring, which is reactive and resource-intensive. | A mix of centralized, remote, and targeted on-site monitoring. | Enables proactive issue detection and reduces travel costs and site burden. |
| Risk Identification | Informal and often occurs after issues arise. | Formal, cross-functional risk assessment conducted at the start of the trial. | Risks are anticipated and managed from the beginning, preventing problems. |
This table shows a clear move away from a "check everything" mentality toward a more intelligent, targeted strategy that ultimately protects patients and produces more reliable data.
Putting RBQM into Practice
Adopting a risk-based approach changes how data management is planned and carried out from day one. It involves several key activities:
- Risk Assessment: At the very start, the trial team works together to identify potential risks to data quality and patient safety. This means analyzing the study protocol, pinpointing critical data points, and thinking through potential operational hurdles.
- Targeted Monitoring: Instead of the standard 100% Source Data Verification (SDV), where every entry is checked against source documents, teams use targeted SDV. They concentrate verification efforts on the most important data, like primary endpoints and safety information.
- Centralized Monitoring: Teams use technology to analyze data from all sites in near real-time. This allows them to see trends, spot sites that are outliers, and catch potential problems early, long before they grow into systemic issues.
By embracing this smarter strategy, clinical trial teams can move beyond the one-size-fits-all model. They can build more resilient, efficient, and effective data management for clinical trials, ensuring their attention stays on what matters most: protecting patients and delivering trustworthy scientific evidence.
How AI Is Actually Transforming Clinical Data Management
The conversation around artificial intelligence often drifts into futuristic scenarios, but its real impact on data management for clinical trials is much more practical and happening right now. AI isn't about replacing human experts; it’s about giving them powerful tools to handle repetitive, error-prone tasks.
Think of AI as a tireless assistant that can spot subtle patterns in patient data that might take human reviewers weeks to find. It can identify data inconsistencies in real-time and even predict which clinical sites might struggle with enrollment. This frees up data managers to focus on strategic decisions that guide the trial toward success.
This shift is more than a small improvement; it's a fundamental change in how trials are conducted. Projections show that by 2025, artificial intelligence tools could manage up to 50% of data-related tasks in clinical trials. Furthermore, adding predictive analytics can lower overall trial costs by a significant 15–25%, offering major financial relief for sponsors and contract research organizations. You can explore more about these powerful trends in clinical data research to see where the industry is heading. This move toward intelligent automation is a necessary evolution for handling the growing complexity of modern research.
From Reactive Fixes to Proactive Insights
Traditionally, data management has been a reactive process. A problem appears—a missing value or a contradictory entry—and a query is raised to fix it. AI flips this model on its head by enabling proactive and predictive actions. Instead of just cleaning data after the fact, AI algorithms can learn from past trials to forecast future challenges.
For example, predictive analytics can analyze historical site performance data to identify which locations are most likely to face enrollment delays or produce high rates of data errors. Armed with this insight, a sponsor can provide targeted support to those sites before problems occur, preventing costly delays. This is a huge step beyond simply flagging errors; it's about stopping them from happening in the first place.
Practical AI Applications in Today's Trials
The value of AI is best understood through its specific applications. These tools are already being added to existing workflows to improve quality and speed. To see the wider impact of AI in medicine, you can read about the 8 Ways AI Medical Staff Reshape Healthcare in 2025.
The table below provides a snapshot of how AI is being applied across different phases of a clinical trial. It highlights the direct link between these applications and measurable gains in efficiency and cost savings.
| AI Application | Trial Phase | Efficiency Gain | Cost Reduction |
|---|---|---|---|
| Automated Data Cleaning | Data Review & Validation | Up to 70% reduction in manual query generation. | Lowers the cost of data cleaning and monitoring. |
| Predictive Site Selection | Study Startup & Planning | Identifies high-performing sites, shortening startup timelines. | Reduces costs associated with underperforming sites. |
| Patient Cohort Identification | Recruitment | Scans electronic health records (EHRs) to find eligible patients faster. | Lowers patient recruitment costs and speeds up enrollment. |
| Safety Signal Detection | Ongoing Monitoring | Early detection of adverse event patterns across the trial. | Mitigates risks and prevents costly safety-related trial holds. |
As shown, AI's role is not a single function but a collection of specialized tools that address key bottlenecks in the trial process. From planning to monitoring, these applications work together to make the entire operation more intelligent and resource-efficient.
One of the most impactful applications is in data cleaning. An AI tool, like those we develop at PYCAD, can be trained to recognize common error patterns specific to a study protocol. It can automatically flag illogical date sequences, inconsistent lab values, or unusual patient-reported outcomes with a high degree of accuracy. This doesn't remove the need for human oversight, but it does dramatically reduce the number of trivial queries. This allows data managers to focus their expertise on complex issues that require critical judgment, making the entire data management for clinical trials process smarter.
Navigating Regulatory Requirements That Actually Matter
Regulatory compliance in clinical trials can feel like trying to solve a maze while blindfolded. But what experienced data managers know is that it’s not about memorizing every single guideline. The real goal is to build systems that naturally meet the core expectations of bodies like the Food and Drug Administration (FDA) and the European Medicines Agency (EMA). This approach turns compliance into a natural outcome of good work, not an extra burden.
This is especially important as data management for clinical trials grows more complex with decentralized trials and AI-driven analysis. Yet, the essential principles of data integrity haven't changed. Regulators are most concerned with one thing: is the final data reliable, attributable, and accurate enough to support conclusions about a new therapy's safety and effectiveness?
The Foundation: Data Integrity Principles
Think of regulatory guidelines as the "rules of the road" for your data. They exist to ensure everyone's safety—specifically, patient safety and data quality. The most critical rules revolve around a few key principles. These are the elements that can make or break an audit, so they are worth focusing on.
Regulators care most about these key principles:
- Traceability: Can every data point be tracked back to its source? A complete audit trail logging every change—who made it, when, and why—is non-negotiable.
- Accountability: Are roles and responsibilities clearly defined? Regulators must see that only authorized individuals can enter or modify data.
- Legibility: Is the data readable and understandable? This applies to both electronic records and any original source documents.
- Contemporaneous Recording: Was the data recorded at the same time it was generated? Backdating records or entering data from memory days later is a major red flag.
By building your data management system around these pillars, you create a foundation that naturally aligns with most regulatory expectations. This makes specific compliance checks much simpler down the line.
Understanding the Official Guidance
Regulatory bodies like the FDA provide detailed guidance documents to help trial sponsors. These documents explain the specific expectations for electronic records, digital signatures, and overall data handling.
For example, this screenshot from the FDA's website shows the wide range of guidance available for clinical trials.

The main takeaway here is that regulators are transparent about what they require. Documents like 21 CFR Part 11 are not mysterious obstacles; they are blueprints for building trustworthy electronic systems. This particular regulation provides the framework for making sure electronic records and signatures are just as reliable as their paper equivalents.
Achieving compliance isn't a one-time check, but a continuous process. It involves regular staff training on standard operating procedures (SOPs) that are aligned with these guidelines. It also means choosing technology, like the AI-powered tools from PYCAD, that has compliance features built-in, such as robust audit trails and secure access controls.
Ultimately, navigating regulatory requirements is less about fearing an audit and more about a commitment to quality. By focusing on the core principles that truly matter to regulators, you can design a data management for clinical trials strategy that is both compliant and efficient. This proactive approach saves months of work during regulatory reviews and builds confidence in your results, ensuring your study's data is strong enough to support the next medical breakthrough.
Building Data Workflows That Actually Work in Practice
Creating a functional data management workflow is like designing the plumbing system for a new house. A complex blueprint might look impressive, but if the pipes don't connect correctly, you’ll have leaks and backups. We’ve all seen elaborate workflow charts that crumble under the pressure of a real clinical trial. This section covers practical workflows that stand up to the test, from initial database setup to the final lock.
The aim is to create a system that is strong enough to maintain data integrity yet simple enough for a busy clinical team to use without constant headaches. A well-designed workflow anticipates common problems, clarifies communication channels, and makes producing high-quality data the easiest option. It’s the difference between a trial that runs smoothly and one that’s in a constant state of crisis management.
Designing Case Report Forms That People Can Use
The Case Report Form (CRF), whether on paper or in a digital system, is the starting point for all trial data. A confusing or poorly organized CRF is a major source of errors and frustration for site staff. The goal is to strike a balance between collecting all necessary data and not overwhelming the people responsible for entering it.
Here are a few guidelines for creating user-friendly CRFs:
- Keep It Logical: Arrange questions in the same order they would be gathered during a patient visit. Group related items together to create a natural flow.
- Be Unambiguous: Use plain, clear language. Avoid technical jargon or questions that could be interpreted in more than one way.
- Minimize Free Text: Use dropdown menus, checkboxes, or radio buttons wherever you can. This practice not only cuts down on typos but also standardizes the data right at the source—a fundamental principle of good data management for clinical trials.
A frequent misstep is designing CRFs that attempt to capture every imaginable piece of information. A more effective strategy is to concentrate only on the data required to support the study's primary and secondary goals.
From Data Entry to Clean Data: The Review Cycle
Once data is in the system, the review and cleaning process kicks off. This shouldn't be a frantic scramble just before the database lock. Instead, it should be a consistent, ongoing cycle that identifies and corrects errors as they happen. An effective review cycle requires clear rules for data validation, managing discrepancies, and resolving queries.
This entire process usually happens within an Electronic Data Capture (EDC) system. The image below shows what a typical EDC interface looks like, serving as the central hub for data entry and validation.

This interface shows how structured entry fields and instant validation checks are built directly into the process. For example, the system can automatically flag an entry if a patient's age is typed as "200," stopping a simple typo from becoming a bigger problem. A properly configured EDC system is a team's best defense against poor data quality.
The workflow for handling discrepancies found by these systems generally follows these steps:
- Automated Check: The EDC system runs pre-set validation checks (like range checks or logic checks) to flag potential mistakes.
- Query Generation: A query is created, either automatically or by a data manager, to notify the clinical site of the issue.
- Site Review: The site coordinator looks at the query, checks the original source document, and either corrects the value or provides a clarification.
- Query Resolution: The data manager reviews the site's response and closes the query once the issue is fixed.
By following this clear, repeatable process, teams can maintain a steady rhythm of data cleaning throughout the trial. This approach prevents a massive pile-up of unresolved queries, which is a common cause of delays in locking the database. Building in this flexibility and structure ensures that when unexpected issues pop up, the core workflow remains stable and productive.
Choosing Technology Solutions That Won't Let You Down
Picking the right technology for data management in clinical trials often feels like an impossible choice. Vendors promise a quick fix, but the truth is more complicated. The key is to look past the marketing hype and focus on what truly boosts efficiency and data quality, instead of chasing fancy features with little real-world benefit. A smart technology choice is about finding solutions that fit your immediate needs and can grow with you.
This isn't about searching for a single, flawless system. It's about creating a connected environment of tools that cooperate. The most important factor here is integration. A top-tier Electronic Data Capture (EDC) system is practically useless if it can't seamlessly share information with your trial management or lab information systems. When data is isolated, it creates manual work, raises the risk of errors, and undermines the very reason for investing in technology.
Core Features That Truly Matter
When looking at different platforms, it's easy to get sidetracked by impressive dashboards and specialized functions. However, seasoned teams know to prioritize a handful of core features that are the foundation of any reliable clinical data management process. These are the non-negotiable elements that guarantee data integrity, compliance, and smooth operations.
Focus your evaluation on these essentials:
- Robust Audit Trails: This is a basic regulatory must-have. The system needs to automatically track every single change to the data—who made it, when they made it, and why. This creates a permanent, unchangeable record that is critical for any inspection.
- Flexible and Configurable Workflows: No two clinical trials are the same. Your technology should let you set up data validation rules, query management cycles, and user permissions to fit your study protocol. It shouldn't lock you into a rigid, one-size-fits-all approach.
- Intuitive User Interface (UI): If the system is a headache for clinical site staff to use, data quality will inevitably drop. A clean, logical interface means fewer data entry mistakes and less need for extensive training and support, which is a major plus for busy sites.
- Strong Security and Access Controls: Protecting sensitive patient information is non-negotiable. The platform must have solid security measures, including role-based access that ensures users can only see or change the data they are authorized to handle.
This screenshot shows how a unified platform integrates different data management tools into a single view.
The main takeaway from this image is the shift toward integrated suites. These combine EDC, eCOA (electronic Clinical Outcome Assessment), and randomization into one cohesive environment. This unified model helps break down the data silos that often complicate trial management and create bottlenecks.
Making the Right Choice for Your Team
Choosing a platform should be a collaborative effort that includes data managers, clinical operations staff, IT, and quality assurance. As you compare options, it's helpful to see what different technology providers offer. For example, you can Explore ferndesk's offerings to see how various companies present their solutions.
In the end, the best technology is the one your team will actually use. Managing the rollout is just as important as the selection. This means planning for data migration, offering complete training, and showing how the new system adds value to get everyone on board. Choosing technology is not just an IT decision; it's a strategic choice that directly affects the speed, quality, and outcome of your clinical trials.
Measuring Success Beyond Basic Metrics
Focusing only on operational metrics like query rates or database lock timelines is like judging a chef by how quickly they wash dishes. While dishwashing is important, those numbers don't tell you anything about the quality or impact of the food. In data management for clinical trials, the most effective teams look beyond these simple process metrics to measure what truly matters for a trial's success.
The real aim is to see how data management activities affect the bigger picture. For example, a clunky and difficult data collection process can frustrate site staff, which might lead to more patients dropping out. On the other hand, a smooth, intuitive process can improve patient retention. This changes the question from "How fast did we clean the data?" to "Did our data management strategy help keep patients in the trial?"
Establishing Meaningful Benchmarks and KPIs
To measure what matters, teams need to connect their daily work to the high-level goals of the clinical trial. This means creating Key Performance Indicators (KPIs) that show strategic value, not just operational speed. These benchmarks create a clear link between data management tasks and the overall health of the study, helping sponsors make smarter decisions.
A strong KPI framework goes beyond simple counts to measure impact and reliability. For instance, tracking timeline predictability—how accurately your actual database lock date matched the initial forecast—is much more useful to stakeholders than just reporting the final date. It shows that you have control over the process and that your projections can be trusted.
To understand how high-performing teams measure their true impact, it helps to look at the specific KPIs they track. The table below outlines a few essential metrics that connect data management efforts to trial quality and efficiency.
Essential Clinical Data Management KPIs
Key performance indicators for measuring clinical data management effectiveness and quality
| KPI Category | Metric | Target Range | Impact on Trial Success |
|---|---|---|---|
| Data Quality | Critical Data Error Rate | < 1% | Ensures that the primary endpoint and safety data are reliable enough for final analysis. |
| Efficiency | Cycle Time from Data Entry to Query Resolution | < 5 business days | Reduces backlogs and keeps the data cleaning process moving forward without major delays. |
| Site Performance | Site Query Rate | < 10% of total data points per site | Helps identify specific sites that might need more training or support to improve their data quality. |
| Predictability | Timeline Adherence for Major Milestones | 95-100% | Builds confidence with sponsors and allows for more accurate resource and budget planning. |
These KPIs shift the focus from merely being busy to being effective. By tracking and improving these metrics, data management teams can clearly show how their work directly contributes to a more reliable and successful clinical trial.
Communicating Value to Executive Leadership
One of the biggest hurdles for data management leaders is demonstrating the value of their work to executives who are focused on the bottom line, not technical specifics. The key is to translate data management wins into the language of business: risk, cost, and speed.
Instead of sharing a dashboard filled with query statistics, frame the results around return on investment (ROI). For example:
- Cost Savings: Explain how automating data validation reduced the need for on-site monitoring, saving the company a specific dollar amount in travel expenses.
- Risk Mitigation: Show how the early detection of a data trend helped prevent a potential safety issue, avoiding a costly trial hold and protecting patients.
- Accelerated Timelines: Demonstrate how efficient data cleaning processes helped lock the database four weeks ahead of schedule, which could bring a new treatment to market sooner.
When you link clean data to faster approvals and lower operational risk, your data management for clinical trials program becomes a strategic asset. This approach proves that investing in solid data management technology and processes, like the AI-powered solutions from PYCAD, isn't just a cost center—it's a direct driver of clinical and commercial success.
Ready to see how AI can optimize your data workflows and deliver measurable ROI? Explore PYCAD's advanced medical imaging solutions today.






