Tissue perfusion is the unsung hero of your body's physiology. It’s the process that ensures oxygen-rich blood actually reaches the tissues that need it most. Think of it as the final, most crucial leg of your body's internal delivery service, making sure every single cell gets the fuel it needs not just to function, but to survive.
What Is Tissue Perfusion Really

Let's get past the textbook definition of tissue perfusion and use an analogy that makes more sense. Picture your body as a sprawling, vibrant city. Your circulatory system is the intricate network of highways, streets, and alleyways, and your red blood cells are the fleet of delivery trucks.
These trucks are packed with essential cargo—namely, oxygen and nutrients—that every home, factory, and office (your cells) desperately needs to keep the lights on.
Tissue perfusion is that "last-mile" delivery. It's the moment the delivery truck pulls up to the doorstep and the package is handed off. It’s not just about blood flowing near the cells; it’s about the successful exchange that happens in the microscopic alleyways of your city, the tiny blood vessels we call capillaries.
The Two-Way Street Of Cellular Health
But it's not a one-way trip. This process is a constant, bustling exchange. As those delivery trucks drop off their vital supplies, they also pick up the garbage—metabolic waste products like carbon dioxide.
This waste is then hauled away for disposal, keeping the cellular neighborhood clean and running smoothly. If the sanitation department went on strike, toxins would pile up, leading to cellular damage and eventually, system-wide failure.
So, in medical terms, tissue perfusion is the flow of blood through the capillary bed of a tissue. It’s the mechanism for delivering what's needed for metabolism and carting away what's not. When this process breaks down, we call it ineffective tissue perfusion. The tissue's needs go unmet, and the consequences can range from organ damage to far more serious outcomes, a topic well-covered in nursing care resources.
At its core, tissue perfusion is the lifeblood of cellular function. It's the difference between a thriving, vibrant city and one where the supply lines have been choked off, grinding everything to a halt.
To really appreciate how vital this process is, it helps to break down its core functions. Each one plays a distinct and critical role in keeping your internal city humming.
Key Components of Healthy Tissue Perfusion
The table below outlines the four critical jobs performed by tissue perfusion, using our city analogy to make each one clear.
| Function | Description | Real-World Analogy (Delivery Network) |
|---|---|---|
| Oxygen Delivery | Transporting oxygen from the lungs to every cell for energy production. | The primary cargo delivery service ensuring every home has power. |
| Nutrient Supply | Distributing nutrients like glucose and amino acids absorbed from digestion. | The grocery delivery service that stocks the pantries of the city. |
| Waste Removal | Collecting metabolic byproducts like carbon dioxide and lactic acid. | The sanitation department that removes trash to keep the city clean. |
| Temperature Regulation | Helping to distribute heat throughout the body to maintain a stable temperature. | The city’s HVAC system, ensuring all buildings are comfortable. |
From delivering power and food to taking out the trash and managing the climate, tissue perfusion is a masterclass in logistics. When every component works in harmony, your body thrives.
The Engine Driving Your Body's Delivery System
Think of tissue perfusion as the final, crucial step in a massive logistics operation happening inside you every second. If perfusion is the last-mile delivery to your body's cellular neighborhoods, then the cardiovascular system is the powerful engine and complex network of highways that makes it all happen. This isn't a passive process; it's actively managed by a few key players working in perfect harmony.
The heart is mission control, the central pump pushing everything forward. It’s responsible for dispatching the fleet of "delivery trucks"—your red blood cells—fully loaded with life-sustaining oxygen. How hard and how often the heart pumps dictates the total volume of goods shipped out at any given moment.
The Dynamics of Blood Flow
This brings us to three critical factors that really define the efficiency of your internal delivery system. You can think of them as the key performance indicators for your body's logistics network:
- Cardiac Output: This is the total volume of blood the heart pushes out every minute. It’s a direct measure of how much supply is available to meet the body's constant demand.
- Blood Pressure: This is the force that keeps traffic moving through the highways (your arteries). It needs to be strong enough to propel blood to the most remote tissues, but not so forceful that it starts damaging the arterial walls themselves.
- Vascular Resistance: This is all about the condition of the roads. Are the arteries wide open and clear, or are they narrowed and congested? Smooth, flexible arteries offer low resistance, letting blood flow easily. But when vessels are constricted—like a highway down to one lane for construction—resistance skyrockets, slowing everything down.
These three elements are in a constant, delicate dance. For example, if vascular resistance goes up because arteries have narrowed, the heart has to work harder (increasing cardiac output) to maintain the necessary blood pressure and keep those deliveries on schedule. It's an incredibly adaptive and responsive system.
This infographic helps visualize how these core components are directly linked.
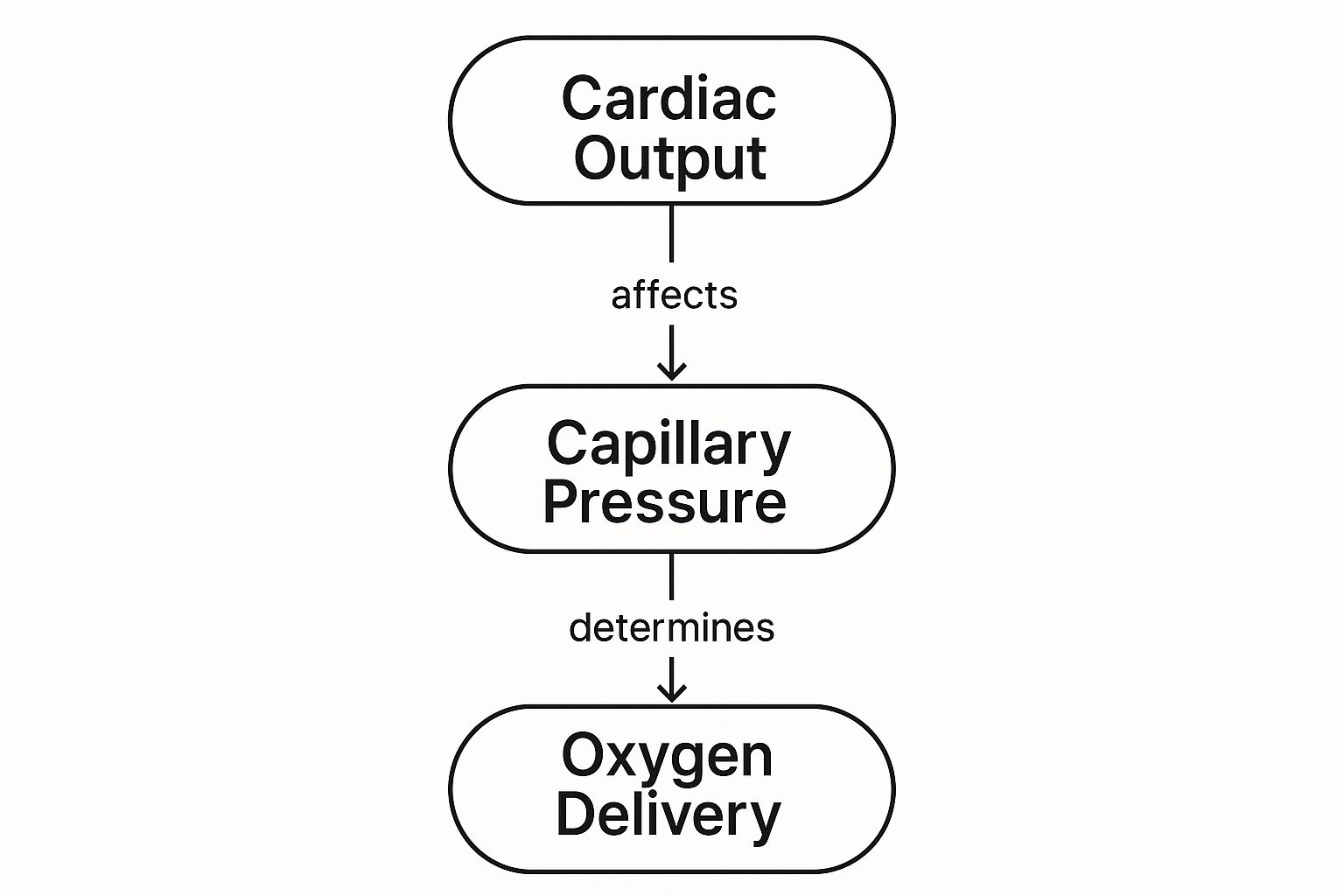
As you can see, it all starts with a healthy cardiac output. That initial push from the heart generates the capillary pressure needed to successfully deliver oxygen from the blood into the tissues.
The All-Important Cargo Carrier
Of course, even the world's best delivery network is useless if the trucks are empty. The cargo itself has to be packaged correctly, and that's where hemoglobin steps in. Hemoglobin is the protein inside red blood cells that grabs onto oxygen molecules and carries them along for the ride.
Without enough hemoglobin, your delivery trucks are essentially traveling empty. Even with perfect heart function and blood pressure, a low hemoglobin count (anemia) means the fundamental goal of tissue perfusion fails because the oxygen never makes it to its final destination.
This whole engine—the heart's pumping action, the condition of the vascular roadways, and the oxygen-carrying capacity of hemoglobin—has to work together seamlessly. When any single part of this system breaks down, that final, critical delivery is compromised, leading to the serious problems associated with poor perfusion.
When the Body's Delivery Network Fails

A perfectly designed delivery system is useless if nothing is moving. When that constant, life-giving flow of blood to your tissues falters—slowing down or stopping entirely—the body is thrown into a state of crisis. We call this hypoperfusion. It's the clinical term for poor tissue perfusion, and it signals a catastrophic failure in your internal logistics.
This failure isn't always dramatic. Have you ever had your foot "fall asleep" after sitting cross-legged for too long? That familiar pins-and-needles feeling is actually a minor, temporary case of hypoperfusion. You've simply pinched off the blood vessels, created a tiny traffic jam, and your nerves are sending up a protest signal.
When this breakdown happens on a larger scale, however, it's a full-blown medical emergency. The fallout from poor tissue perfusion depends entirely on how bad the breakdown is and where it’s happening.
Common Causes of Circulatory Breakdown
Hypoperfusion usually traces back to a few core problems within the circulatory network, each one throwing a wrench into the works in its own unique way. The root cause typically falls into one of these buckets:
- Low Blood Volume (Hypovolemia): Think of this as a "truck shortage." If you've lost a lot of blood from an injury or are severely dehydrated, there just aren't enough delivery vehicles to get oxygen and nutrients where they need to go.
- Vessel Blockage (Ischemia): This is a complete road closure. A blood clot gets stuck in an artery—the classic mechanism of a heart attack or ischemic stroke—creating an impassable barrier. Everything downstream is starved of oxygen.
- Pump Failure (Cardiogenic Shock): The main distribution center is down. If the heart muscle is damaged and can no longer pump effectively, the entire delivery network slows to a crawl, if not a complete halt.
These are just a few high-level examples. Conditions like peripheral artery disease (PAD) cause chronic traffic jams by slowly narrowing the arteries over years. In contrast, something like sepsis can trigger widespread vessel dilation, causing blood pressure to plummet and bringing the whole system crashing down.
The Cellular Cry for Help
So what actually happens at the microscopic level when the oxygen stops arriving? Your cells are forced to abandon their normal, highly efficient energy production method (aerobic metabolism) and switch to a desperate, last-ditch survival mode (anaerobic metabolism).
This emergency backup plan is incredibly inefficient and, worse, it produces a toxic byproduct: lactic acid.
The buildup of lactic acid in the bloodstream is a critical distress signal. For clinicians, elevated lactate levels are a clear and measurable sign that tissues somewhere in the body are oxygen-starved and fighting to survive, pointing directly to a failure in tissue perfusion.
This switch is a temporary fix at best. If blood flow isn't restored quickly, this cellular crisis escalates, leading to tissue damage, organ failure, and life-threatening shock. That's why restoring adequate tissue perfusion is one of the most urgent priorities in all of emergency medicine.
How Do We Measure Tissue Perfusion?
Think of a doctor checking for poor perfusion like a master plumber trying to find a blockage in a complex network of pipes. They start with the most obvious, hands-on checks before bringing in the high-tech cameras and sensors. This systematic approach allows them to quickly figure out if there’s a local issue, a system-wide failure, or something in between.
The first step is almost always a physical exam. It’s quick, non-invasive, and can give a surprisingly accurate snapshot of what’s happening at the body’s periphery.
The Hands-On Evaluation
A clinician can tell a lot just by looking at and touching a patient's skin. Is it warm and pink? That’s a good sign that warm, oxygen-rich blood is reaching the surface. Or is it cool, clammy, and pale? This immediately suggests that blood flow is being restricted.
One of the classic bedside tests is checking the capillary refill time. By gently pressing on a fingernail until it turns white and then releasing it, a doctor can time how long it takes for the normal pink color to return. In a healthy person, it's almost instant. A refill time dragging on for more than three seconds is a well-known warning sign of poor perfusion in the limbs.
These simple clues are the first pieces of the puzzle, guiding the doctor on whether they need to dig deeper.
A Look Inside with Advanced Tools
When the initial exam raises red flags, it’s time to bring in more powerful tools to see exactly what’s happening inside the circulatory system. This is like moving from a visual inspection of the pipes to using specialized diagnostic equipment.
Here are a few of the go-to methods:
- Blood Tests: Lab work gives us a window into the body's chemical reality. When it comes to perfusion, the gold standard is often a serum lactate test. High lactate levels are a major distress signal, telling us that cells aren't getting enough oxygen and have resorted to an inefficient, anaerobic "emergency backup" mode for energy. You can read more about the clinical importance of lactate levels in critical care.
- Doppler Ultrasound: This amazing tool uses sound waves to create a real-time map of blood moving through your arteries and veins. It allows doctors to literally see and hear the flow, making it invaluable for spotting physical blockages, dangerous clots, or narrowed vessels that are choking off circulation.
- Blood Pressure Monitoring: While a standard cuff reading is useful, critically ill patients often need more. An arterial line—a thin catheter placed directly into an artery—provides a continuous, beat-to-beat measurement of blood pressure. This gives a much more dynamic and accurate picture of the force pushing blood through the body.
Combining the art of the physical exam with the hard data from these advanced tools is what gives clinicians a complete picture. It's this holistic view that allows them to pinpoint not just that there's a problem, but why it's happening.
Comparison of Tissue Perfusion Monitoring Methods
To put it all together, here’s a quick comparison of the different ways clinicians monitor perfusion, from the simplest exam to more complex lab and tech-based assessments.
| Method | What It Measures | Invasiveness | Common Use Case |
|---|---|---|---|
| Physical Exam | Skin color, temperature, capillary refill time | Non-invasive | Initial bedside assessment, rapid triage |
| Blood Pressure Cuff | Systemic arterial pressure (intermittent) | Non-invasive | Routine check-ups, initial vital signs |
| Serum Lactate Test | A biomarker for anaerobic metabolism (cellular oxygen debt) | Minimally invasive (blood draw) | Sepsis, shock, and critical illness monitoring |
| Arterial Line | Continuous, real-time blood pressure | Invasive | Intensive care units, major surgery |
| Doppler Ultrasound | Blood flow velocity and vessel blockages | Non-invasive | Detecting deep vein thrombosis (DVT), assessing arterial disease |
Each method offers a unique piece of information. Ultimately, whether it's a simple touch or a sophisticated blood analysis, every test is designed to answer one crucial question: are the body's cells getting the life-sustaining oxygen and nutrients they need to function? Figuring out where that delivery system has failed is the critical first step to fixing it.
The Slow Damage of Poor Perfusion in Chronic Disease

While a sudden cutoff of blood flow is a clear medical emergency, a slow, creeping decline in tissue perfusion can be just as destructive. It acts like a silent accomplice to many chronic diseases, gradually starving tissues of the oxygen and nutrients they need to function and repair themselves.
This slow-motion crisis doesn’t set off immediate alarms. Instead, it’s like a vital supply line that gets more and more congested over months or years. Eventually, the areas at the very end of the line—often the feet, hands, and eyes—start to show the devastating effects of the chronic shortage.
Diabetes and Its Toll on Tiny Vessels
Diabetes is a classic example of a disease that wages war on perfusion at the microscopic level. Persistently high blood sugar is toxic to the delicate inner lining of the body's smallest blood vessels, the capillaries. This ongoing damage causes the vessels to become stiff and narrow, a process known as microangiopathy, which chokes off blood flow.
As a result, the tissues that depend on this intricate network are slowly suffocated. This is the root cause of many well-known diabetic complications:
- Neuropathy: Nerves, particularly in the feet, can’t get the oxygen they need. They begin to misfire or die off, leading to numbness, tingling, or severe pain.
- Non-Healing Wounds: A simple cut on the foot can escalate into a dangerous ulcer because the damaged tissue doesn't have the blood supply required for healing.
- Retinopathy: The retina, the light-sensitive tissue at the back of the eye, has a dense network of tiny vessels. When their perfusion is compromised, it can lead to vision loss and even blindness.
Studies consistently show that people with type 2 diabetes struggle with tissue oxygenation. One recent analysis found that even when standard circulation tests appeared normal, diabetic participants had a mean tissue oxygen saturation of just 58.7%, compared to 62.1% in healthy individuals. This reveals a hidden oxygen debt at the cellular level. You can read more in the full study on diabetes and tissue oxygenation.
Peripheral Artery Disease: The Clogged Highways
Peripheral artery disease (PAD) is another condition centered on poor perfusion, but this time it affects the larger "highways" of the circulatory system. In PAD, fatty plaques build up inside the arteries that supply blood to your limbs, especially the legs. This narrowing, known as atherosclerosis, essentially creates chronic traffic jams in your body's major roadways.
The tell-tale sign of PAD is claudication—a cramping pain in the legs that flares up with activity, like walking, and subsides with rest. This happens because your muscles are screaming for more oxygen during exercise, but the narrowed arteries just can't deliver it fast enough.
This constant state of poor blood flow puts tissues in a state of borderline crisis. Over time, it can progress to pain even while resting, sores that won't heal, and in the most severe cases, may even lead to amputation.
Both diabetes and PAD drive home a critical point: understanding and maintaining good tissue perfusion is vital not just for surviving emergencies, but for managing long-term health and preserving the quality of life for millions of people.
Still Have Questions About Tissue Perfusion?
We’ve covered a lot of ground, from the nuts and bolts of how tissue perfusion works to its critical role in keeping us healthy. But as with any complex medical topic, a few common questions always seem to pop up. Let's tackle them head-on.
Think of this as a quick FAQ to clear up any lingering confusion.
What's the Real Difference Between Perfusion and Circulation?
This is easily the most common point of confusion, but a simple analogy makes it crystal clear.
Imagine circulation is the entire national highway system. It’s the network of major arteries and veins that carry blood on its long, round-trip journey from the heart to the body and back again. It's the big-picture, coast-to-coast transportation grid.
Perfusion, on the other hand, is the last-mile delivery. It’s what happens when blood exits the highway and turns onto the small neighborhood streets—the tiny capillaries—to drop off vital packages of oxygen and nutrients directly at the front door of every single cell.
Here’s the key takeaway: you can have a perfectly functioning highway system (good circulation) but still have a problem with a local delivery route. A single blocked-off street can prevent an entire neighborhood from getting its supplies, even if traffic is flowing smoothly everywhere else in the country. That's poor perfusion.
Can I Actually Improve My Tissue Perfusion with Lifestyle Changes?
Absolutely. In fact, your daily habits have a massive impact on the health of your body’s intricate delivery network. Great perfusion depends on a strong heart, clean and flexible blood vessels, and the right amount of blood—all things you can directly influence.
Here are some of the most powerful changes you can make:
- Get Moving: Regular aerobic exercise is like a workout for your entire cardiovascular system. It strengthens your heart so it can pump more blood with less effort and keeps your blood vessels pliable.
- Eat for Your Arteries: A diet low in saturated fats and highly processed foods helps prevent the buildup of gunk (arterial plaque) that narrows your blood vessels and chokes off blood flow.
- Ditch the Cigarettes: This is non-negotiable. Smoking is incredibly destructive to the delicate inner lining of your blood vessels, makes your blood stickier, and slashes the amount of oxygen it can carry.
- Stay Hydrated: Your blood is mostly water. When you're dehydrated, your blood volume drops, making your heart work much harder to push thicker blood through your system.
What Are the First Red Flags of Poor Tissue Perfusion?
The early warning signs really depend on where the problem is. Because perfusion is a local event, the symptoms often show up in the specific area that’s being starved of blood.
If it's in your arms or legs (what doctors call poor peripheral perfusion), you might notice:
- Hands or feet that are constantly cold, even when you're otherwise warm.
- Skin that looks unusually pale or even has a slight bluish tinge (cyanosis).
- A persistent "pins and needles" feeling, numbness, or tingling.
- Sharp, cramping pain in your calves or thighs when you walk, which disappears when you stop.
When a major organ is affected, the signs are more serious. For example, poor perfusion to the brain can cause sudden dizziness and confusion. In the heart, it can trigger the chest pain known as angina.
Important: Any of these symptoms, especially if they’re new or getting worse, are your body's alarm system. They're a signal that a critical supply line might be in trouble and should always be checked out by a doctor.
What Exactly Is a Reperfusion Injury?
This one sounds like a paradox, but it's a very real and serious medical challenge.
A reperfusion injury is damage that happens to tissue after blood flow is restored to an area that was deprived of it. It’s like a rescue crew arriving on the scene only to accidentally cause more problems.
Here’s what happens: When oxygen-starved tissue is suddenly flooded with oxygen-rich blood, it can trigger a massive inflammatory reaction. This chemical storm creates a flood of destructive molecules called free radicals, which can attack and kill the already-weakened cells.
Clinicians are acutely aware of this danger, especially when treating heart attacks or strokes where the main goal is to unblock an artery as fast as possible. They use specialized medical protocols to manage the reintroduction of blood flow, aiming to minimize this secondary damage and give the tissue the best possible shot at a full recovery.
At PYCAD, we're focused on the future of medical imaging. We develop AI-powered software that gives clinicians and researchers a clearer, more detailed view of physiological processes like tissue perfusion. Our tools are designed to help analyze medical images with greater speed and precision. To see how our expertise in AI can support your medical device or research project, learn more about our work.