Let's get straight to the point: healthcare process improvement isn't just a good idea anymore—it's a critical need. This is all about taking a systematic, data-backed look at how healthcare is delivered and making it better, faster, and more affordable. Think of it like a high-performance racing team constantly tuning their car's engine; small, precise adjustments can lead to huge gains on the track.
Why Process Improvement Has Become So Urgent
The healthcare world is caught in a perfect storm. We're seeing escalating costs, major staff shortages, and a burnout crisis among clinicians. Hospitals and clinics are being pushed to their limits, forcing them to find smarter, more efficient ways to operate. This isn't about asking people to work harder; it's about getting rid of the frustrating bottlenecks and wasteful steps that complicate their daily work.
This sense of urgency is palpable in the C-suite. A recent survey of top executives found that over 70% of them ranked improving operational efficiency and productivity as a top priority. It’s a clear signal that fixing these deep-seated systemic issues is now front and center.
The Forces Driving This Change
So, what’s really pushing this need for change? The pressures are coming from multiple directions, affecting every part of the healthcare journey, from the first phone call to the final follow-up.
-
Skyrocketing Costs: Things like redundant lab tests or messy supply chain management aren't just minor inconveniences; they directly drive up expenses and put a massive strain on budgets.
-
The Staffing Crisis: Burnout is a real and present danger, and many facilities are chronically understaffed. By streamlining processes, we can lift the heavy administrative weight off our clinical teams, freeing them up to do what they do best: care for patients.
-
Evolving Patient Expectations: Patients today expect their healthcare experience to be as smooth and transparent as any other service. A confusing check-in process or a long, anxious wait for test results can completely sour their perception of care.
The fundamental goal here is simple: to ditch outdated, clunky workflows and build a modern, efficient model for delivering care. This isn't just about the bottom line; it's essential for providing higher-quality patient outcomes.
How Better Processes Lead to Better Patient Outcomes
At the end of the day, every single improvement we make comes back to the patient.
When you smooth out an administrative process, you reduce the stress on a person who is already worried about their health. When a diagnostic workflow is made more efficient, a patient gets a faster, more accurate diagnosis, which can make all the difference in their treatment and recovery.
Every bottleneck you eliminate and every potential error you prevent directly benefits the person at the center of it all. It’s why so many proven strategies to increase patient satisfaction are rooted in process improvement. By making the system work better for everyone inside it—staff included—we build a stronger, more compassionate, and more effective healthcare system for all.
Core Methods for Streamlining Healthcare Operations

If you really want to fix operational headaches in healthcare, you need a game plan. Healthcare process improvement isn't about guesswork; it relies on established methods that serve as roadmaps for finding what’s broken and making it right. These aren't just abstract theories from a textbook—they are practical toolkits built for the messy reality of healthcare.
Let's cut through the jargon and look at the most influential frameworks. Think of these as different lenses for viewing and improving your daily operations. Getting a handle on these methods is the first real step toward changing how your organization works, creating a smoother experience for your staff and, most importantly, your patients.
Declutter Your Workflows with Lean
Imagine your most cluttered supply closet. Finding anything is a chore, and you probably have expired items taking up space. The Lean methodology is essentially a systematic way to declutter your entire organization, not just a closet. It’s all about identifying and removing "waste" from every single process.
In healthcare, waste is anything that doesn’t directly contribute value to the patient.
- Wasted Time: Think of patients stuck in the waiting room, staff hunting for a working IV pump, or agonizing delays in getting critical lab results.
- Wasted Motion: A classic example is a nurse crisscrossing a unit multiple times to gather supplies for one patient because of a poorly designed floor plan.
- Wasted Resources: This could be anything from ordering unnecessary diagnostic tests to overstocking supplies that end up expiring on the shelf.
By visually mapping a process—say, from patient admission to discharge—a team can literally see where the bottlenecks and wasteful steps are. From there, you can redesign the workflow to be more direct, logical, and efficient.
Rooting Out Errors with Six Sigma
If Lean is about decluttering, then Six Sigma is about being a world-class detective. This approach is intensely data-driven and obsessed with one primary goal: eliminating defects and reducing variation. In a hospital, a "defect" isn't a faulty product; it's a medication error, a misread scan, or a hospital-acquired infection. The stakes are incredibly high.
Six Sigma uses rigorous statistical tools to dig deep and find the root cause of these errors. The point isn't to place blame on a person but to fix the broken system that allowed the mistake to occur in the first place.
A hospital might use Six Sigma to tackle a stubbornly high rate of post-surgical infections. The team wouldn't just guess; they would collect hard data on everything—from hand-washing compliance and sterilization techniques to operating room airflow. By analyzing this data, they can pinpoint the critical factors and implement targeted changes to drive that infection rate toward zero.
This relentless focus on quality and consistency makes Six Sigma a go-to methodology for high-risk clinical environments where precision is everything.
Testing Changes with PDSA Cycles
Not every improvement needs to be a massive, six-month project. The Plan-Do-Study-Act (PDSA) cycle is a much simpler, faster framework for testing ideas on a small scale. Think of it as running a series of mini-experiments right in your own department.
Here’s the breakdown:
- Plan: Your team identifies a problem and comes up with a small, manageable change. For instance, you believe rewriting a confusing patient intake form could speed up check-in.
- Do: You test the change. Instead of rolling it out everywhere, you try the new form with the next 10 patients.
- Study: Now you analyze the results. Was the new form clearer? Did it actually reduce check-in time or errors?
- Act: Based on what you learned, you can adopt the change permanently, tweak it for another test, or scrap the idea if it didn't help.
This iterative loop empowers frontline staff to solve the problems they face every day. It builds a culture of continuous healthcare process improvement, where everyone is engaged in making things work better. Of course, while these methods are powerful, they often rely on stable digital infrastructure. Foundational elements like optimizing network performance are critical to ensure the underlying technology can support these improvement initiatives without a hitch.
Why Smart Processes Are a Financial Lifeline for Healthcare

While better patient outcomes are always the North Star for any healthcare organization, let's be honest: financial stability is the engine that makes the mission possible. Healthcare process improvement isn't just some operational buzzword; it's a core strategy for survival in an increasingly tough economic climate. Inefficient workflows aren't just minor annoyances—they're a slow, steady, and significant drain on an organization's resources.
Every single day, hidden costs pile up from processes that just don't work. Think about it. What’s the real cost of ordering a redundant lab test simply because the first result got lost in a clunky communication shuffle? Or the expense of a patient staying in the hospital an extra day due to administrative delays in the discharge process? These aren't one-off mistakes; they're symptoms of systemic waste that adds up fast.
And this financial pressure is only getting more intense. Medical costs are on a steep climb. One recent report projects a staggering global average increase of 10.4%. Here in North America, the medical trend rate is expected to hit 8.7%. With costs rising relentlessly, making processes smarter isn't just a good idea—it's essential. You can dig deeper into these numbers and what's behind them in the full 2025 Global Medical Trends Survey.
Finding the High-Cost Bottlenecks
To get a handle on costs, leaders need to know exactly where the money is leaking out. Inefficient processes have a funny way of hiding in plain sight, often disguised as "the way we've always done it." But these are usually where the biggest opportunities for savings are waiting.
Common culprits draining the budget often include:
- Supply Chain Mismanagement: This could be anything from over-ordering supplies that just sit on a shelf until they expire to frantically paying a premium for last-minute items. Both scenarios directly hit the bottom line.
- Billing and Coding Errors: A single mistake in coding can get a claim flat-out rejected. That means hours of administrative rework to fix and resubmit it, which delays revenue and drives up labor costs.
- Suboptimal Staff Scheduling: When schedules are a mess, you're either paying expensive overtime to handle unexpected patient surges or wasting money on staff who are standing around during lulls.
Each of these is a workflow problem with a direct, negative financial impact. This is precisely where a focused healthcare process improvement initiative can deliver a powerful return on investment.
By framing process improvement as a financial necessity, healthcare leaders can build a powerful case for change. This isn't about cutting corners on care. It's about eliminating waste to free up resources that can be put back into what truly matters: the patient.
How Saving Money Translates to Better Care
Ultimately, saving money isn't just about padding the balance sheet. Every dollar saved by fixing a broken process is a dollar that can be redirected to areas that directly impact patient care.
Just imagine what a hospital could do with the money it recovers from stamping out redundant tests and administrative errors. Those funds could buy a new MRI machine, help hire more nurses to improve patient-to-staff ratios, or pay for advanced training to keep clinical teams at the top of their game.
Every minute shaved off operating room turnover time or every error prevented in the pharmacy does more than just cut costs—it strengthens the entire organization's ability to provide safe, effective, and high-quality care. This clear line between operational efficiency and financial health shows that process innovation is a true cornerstone of sustainable, modern healthcare.
How AI Is Revolutionizing Healthcare Workflows
If you think of traditional improvement methods like Lean and Six Sigma as the essential tools in a mechanic's garage, then Artificial Intelligence is the turbocharger you add to get a whole new level of performance. AI isn't here to throw out those proven frameworks for healthcare process improvement; it’s here to make them smarter, faster, and more predictive. It acts like an intelligent partner, spotting patterns in data that are simply invisible to the human eye.
Here’s a practical way to think about it. A hospital team could spend a month manually tracking patient flow to find a bottleneck. That's a classic, valuable technique. But an AI-powered system can chew through years of admissions data in minutes, predicting future patient surges with impressive accuracy. This allows leadership to shift from reacting to problems to proactively adjusting staffing and resources before a crisis hits.
This isn't just a futuristic idea; it's quickly becoming the new reality. A recent survey revealed that 86% of healthcare organizations are already using AI technologies in some capacity. We're seeing it applied everywhere, from automating mountains of administrative paperwork to helping clinicians catch diseases earlier. The global healthcare AI market is even expected to blow past $120 billion by 2028, which tells you just how much momentum is behind this shift. For a closer look, you can see this breakdown of AI adoption in healthcare.
Supercharging Data Analysis and Prediction
One of AI's biggest strengths is its ability to turn raw data into genuinely useful insights. Healthcare systems produce an unbelievable amount of information every single day—electronic health records (EHRs), lab results, imaging scans, and more. Asking a person to sift through all of that is an impossible task.
This is where AI algorithms, especially machine learning models, shine. They can find subtle connections and trends that would otherwise go completely unnoticed.
-
Predictive Staffing: AI can analyze historical data on patient admissions, local flu seasons, and even weather patterns to forecast demand in the emergency room. This leads to smarter scheduling that prevents being caught understaffed during a rush or overstaffed during a lull.
-
Supply Chain Optimization: By predicting the need for specific medical supplies and medications, machine learning can automate orders. This helps prevent stockouts of critical items while cutting down on waste from over-ordering.
-
Risk Stratification: AI models can scan a patient's health record to flag individuals at high risk for serious issues like sepsis or hospital readmission. This gives clinical teams a heads-up to intervene early.
AI fundamentally changes the question from "what just happened?" to "what is likely to happen next?" This predictive power is what unlocks a whole new tier of efficiency and preemptive care.
Comparing Traditional vs AI-Powered Process Improvement
To really grasp the difference, it helps to see the old and new approaches side-by-side. The table below breaks down how AI elevates conventional methods, turning them from manual, reactive processes into automated, predictive ones.
| Aspect | Traditional Methods (e.g., Manual Lean/Six Sigma) | AI-Powered Methods |
|---|---|---|
| Data Analysis | Manual, often limited to small samples and spreadsheets. | Automated, capable of analyzing massive, complex datasets. |
| Timeframe | Slow and labor-intensive; projects can take weeks or months. | Rapid analysis, providing insights in near real-time. |
| Focus | Reactive; identifies and fixes problems after they occur. | Proactive and predictive; forecasts future needs and issues. |
| Scalability | Difficult to scale; heavily reliant on human effort. | Highly scalable; can monitor multiple processes simultaneously. |
| Accuracy | Prone to human error and cognitive biases. | High accuracy, identifying patterns invisible to humans. |
As you can see, AI doesn't just do the same things faster—it enables an entirely new, more intelligent way of managing healthcare operations.
Automating Repetitive and Tedious Tasks
A huge chunk of a clinician's day is eaten up by administrative work—charting, coding, and filling out forms. This is a major driver of burnout, and it pulls them away from actual patient care. AI-driven automation is a direct solution to this problem.
For instance, Natural Language Processing (NLP) tools can listen to a conversation between a doctor and patient and automatically generate clinical notes. Imagine summarizing key details and populating the EHR without all that manual typing. This one application can save a doctor hours every day, freeing them up to focus on what they were trained to do. In the same way, AI can automate parts of medical billing and coding, which cuts down on errors and gets the revenue cycle moving faster.
This infographic shows just how real these benefits are, with significant drops in both wait times and error rates.
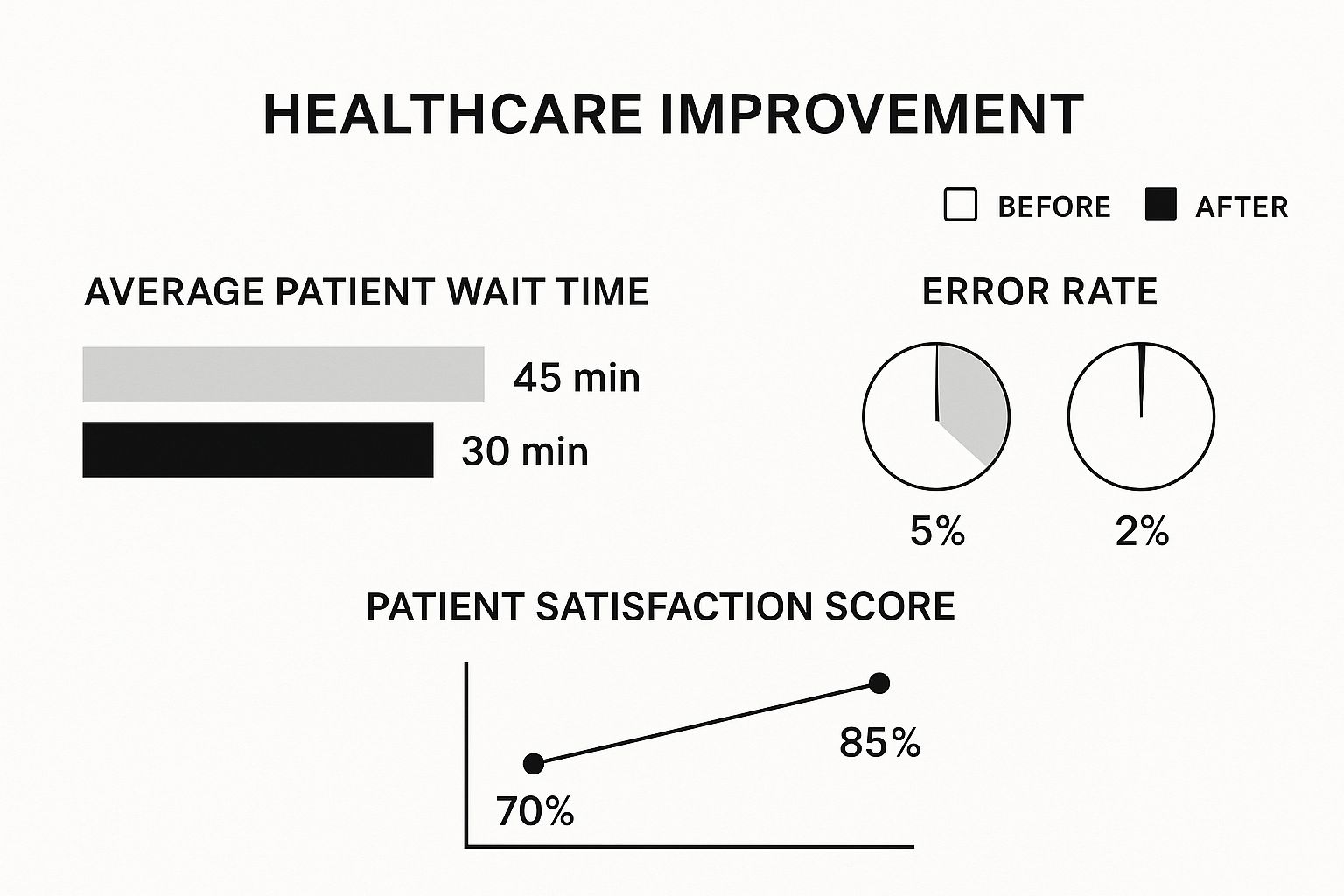
The numbers speak for themselves. Integrating smarter processes delivers clear victories, cutting patient wait times by a third and slashing the error rate by more than half.
Enhancing Clinical Decision Making
Beyond just fixing workflows, AI is also becoming a powerful assistant in making clinical decisions. Take a field like radiology. AI algorithms can scan medical images and highlight potential abnormalities—some so subtle they might be missed by the human eye. This doesn't replace the radiologist; it acts as a tireless, incredibly well-trained second set of eyes, boosting both diagnostic accuracy and speed.
This partnership between human expertise and machine precision is really the heart of modern healthcare process improvement. By taking on the data-heavy, repetitive, and analytical burdens, AI empowers healthcare professionals to work at the top of their game. The result is better patient outcomes and a more resilient, efficient, and caring healthcare system for everyone.
A Real-World Look: Fixing a Broken Medical Imaging Workflow

Theory is one thing, but seeing healthcare process improvement in action is where the lightbulb really goes on. Let’s walk through a case study based on a situation I've seen play out time and again: a mid-sized hospital's radiology department getting bogged down by its own processes. For months, they’ve been stuck, frustrating staff and, more importantly, delaying patient care.
The signs of trouble are impossible to ignore. Referring physicians are complaining about report turnaround times stretching for days, leaving a growing number of patients anxiously waiting for a diagnosis. Internally, scheduling is a nightmare. Expensive MRI and CT scanners sit idle for long stretches, only to be double-booked at peak hours. To top it all off, inconsistent image quality forces patients to return for frustrating—and costly—rescans. The team is dedicated and talented, but they're burning out under the weight of a broken system.
Diagnosing the Ailments in the Workflow
The first, and most critical, step for the department’s leadership is to stop guessing and start measuring. Adopting a Lean mindset, they map out their entire workflow, tracing every step from the moment a physician orders a scan to the final report landing in their hands. This simple act of creating a visual map immediately shines a light on bottlenecks that were previously just considered "part of the job."
A few key problems quickly rise to the surface:
- The Manual Data Burden: Technicians were spending up to 15 minutes per patient just on manual data entry across several disconnected systems. This wasn't just slow; it was a breeding ground for typos and critical errors.
- A Communication Breakdown: Radiologists frequently needed more clinical context from referring doctors, but getting it meant playing a frustrating game of phone tag, putting interpretations on hold.
- Wasted Machine Time: The workflow map exposed a shocking reality: expensive scanners were sitting idle nearly 30% of the time due to inefficient booking and patient no-shows that were never backfilled.
With a clear diagnosis, the team finally had a concrete list of issues to attack. They were no longer just complaining about the symptoms; they were ready to treat the disease.
Implementing a Targeted Treatment Plan
Armed with solid data, the department didn't try to boil the ocean with one massive change. Instead, they rolled out a multi-pronged strategy with specific solutions designed to fix the exact bottlenecks they had identified.
Their new workflow introduced a few key changes:
-
AI-Assisted Diagnostics: The department integrated an AI tool, like those from PYCAD, directly into their PACS system. The AI acts as a "first read" assistant, automatically flagging potential anomalies for the radiologist to review. It doesn't replace the expert; it just helps them get to the crucial parts faster.
-
Automated Scheduling Software: A new system took over the headache of managing scanner appointments. It optimizes the schedule in real-time, sends automated patient reminders to cut down on no-shows, and instantly fills last-minute cancellations from a waitlist.
-
Secure Messaging Platform: A HIPAA-compliant messaging app was launched, creating a direct, secure line between radiologists and referring physicians for those quick, essential consultations.
By focusing on specific, high-impact changes, the department moved from a state of chronic inefficiency to a streamlined, technology-supported workflow. The goal was never to replace human expertise but to augment it, removing friction so skilled professionals could focus on what truly matters: the patient.
The Measurable Results of Improvement
The transformation was clear within six months—not just in feeling, but in hard data. The average report turnaround time plummeted from over 48 hours to just 12 hours. Thanks to the AI-assisted review process, radiologists could increase their daily throughput by 25% without any drop in accuracy.
What's more, the automated scheduling system pushed equipment utilization to over 90%, essentially adding more capacity without the multi-million dollar expense of a new machine.
Perhaps most importantly, staff morale soared. The team was less stressed, felt more in control, and could dedicate their expertise to clinical work instead of being bogged down by administrative quicksand. This is what a systematic approach to healthcare process improvement looks like—marrying proven methodologies with smart technology to create profound, lasting change.
Your Roadmap to Launching an Improvement Initiative
Moving from theory to practice is where the real work—and the real reward—of any healthcare process improvement begins. Real success isn't about launching one big, flashy project. It's about slowly but surely weaving a mindset of continuous improvement into the very culture of your organization. That takes a clear, practical plan that empowers your team from the get-go.
Think of it less like a sprint and more like an expedition. You need the right crew, a good map, and the flexibility to adjust your course along the way. Simply announcing a top-down mandate for change almost never sticks. A successful initiative is built on genuine buy-in and momentum from the ground up.
Step 1: Assemble Your Team and Secure Buy-In
Your first move? Get a sponsor in leadership. This isn't just about getting a signature on a budget request. You need a true champion who will advocate for the project and help clear away the inevitable organizational hurdles. Without that high-level support, even the most brilliant ideas will fizzle out.
With a champion in your corner, it's time to build your team. Make sure it's a cross-functional group that includes not just managers but the frontline staff—the nurses, techs, and admins who live and breathe these processes every single day. Their firsthand experience is gold for spotting what's actually broken and figuring out what a workable fix looks like.
Step 2: Pinpoint the First Problem to Solve
Don't try to boil the ocean. The secret to building real momentum is to score an early, visible win. Let data be your guide. Look at patient wait times, error rates, or even staff satisfaction scores to find a problem area that's both high-impact and high-visibility.
A good place to start is with a process that's a known source of frustration for everyone—staff and patients alike. When you fix that, you send a powerful message: change is possible, and it makes things better. That success makes getting support for the next project a whole lot easier.
The goal is to create a ripple effect. A small, tangible improvement in one area demonstrates value and builds the organizational confidence needed to tackle more complex challenges down the line.
Step 3: Implement and Track Your Changes
Once you've picked your target and a framework to guide you, like Lean or PDSA, it's time to make the change. This is where tracking becomes absolutely critical. You have to measure your key metrics before and after to prove, objectively, that your solution actually worked.
What should you track? It depends on the problem, but some common metrics include:
- Patient-Facing Metrics: Wait times, length of stay, patient satisfaction scores.
- Operational Metrics: Staff overtime hours, supply costs, equipment utilization rates.
- Quality Metrics: Medication error rates, readmission rates, infection rates.
To keep everything on track, it helps to have a digital transformation roadmap that outlines how your tech initiatives support your process goals.
And don't forget to celebrate the wins, no matter how small. Acknowledging your team's hard work shows them their contributions matter. It builds morale and fuels the motivation needed for the next challenge, helping to create a culture of improvement that lasts.
Frequently Asked Questions
When you start digging into healthcare process improvement, a lot of questions pop up. Getting straight, practical answers is the best way to move forward with confidence and sidestep the common traps that can derail a project before it even gets going. Here are a few of the most common questions we hear from healthcare leaders.
Where Should We Start Our Improvement Efforts?
The honest answer? Start small. It's tempting to try and fix a huge, system-wide problem right out of the gate, but that's usually a recipe for frustration. Instead, zero in on a process with visible, high-impact issues that everyone feels—think of things like appointment scheduling or the patient discharge workflow.
Choosing a pain point like this is smart for two reasons. First, it's a problem everyone already recognizes, so any improvement you make will be noticed and appreciated almost immediately. Second, scoring a quick, tangible win builds incredible momentum. It’s far easier to get support for bigger projects when you’ve already proven you can deliver results.
Think of it as a pilot project. When you prove the value of process improvement on a small scale, you turn skeptics into supporters. It’s the first step in building a culture that embraces change.
How Do We Measure the Success of Our Initiatives?
Success isn't about feelings; it's about data. You need to define what you're trying to achieve with clear, specific metrics from the very beginning. You absolutely have to track these metrics before and after you make a change. Without that baseline, you can't prove your efforts made a real difference.
Here are a few metrics that actually tell a story:
- Time: Did you cut down patient wait times? Is the turnaround for diagnostic reports faster? Are you getting patients discharged more quickly?
- Quality & Safety: Have you seen a drop in hospital readmission rates or fewer medication errors? Are patient safety scores on the rise?
- Financials: Have operational costs gone down? Are you wasting fewer supplies? Is the billing cycle time shorter?
- Satisfaction: Are your patient satisfaction scores climbing? Is staff morale better, and are you seeing improved retention?
How Can We Get Our Clinical Staff On Board?
This one is crucial: clinician buy-in is non-negotiable. If you try to force change from the top down, it will fail. The only way to succeed is to involve your clinical team from day one.
Frame the whole project around how it makes their lives and their patients' lives better. The focus has to be on reducing their administrative headaches and improving care quality, not just on boosting the bottom line.
Your best bet is to create a cross-functional team with doctors, nurses, techs, and admin staff working together. When they help design the solution, they take ownership of it. This ensures the changes are practical, solve their actual problems, and will stick around for the long haul.
At PYCAD, we focus on building the AI tools that drive modern healthcare process improvement, especially in medical imaging. Our goal is to help you enhance diagnostic accuracy and simplify workflows to achieve results you can actually measure. To see how we can help with your next initiative, learn more about PYCAD.






