Let’s be honest—improving hospital operational efficiency is more than just a line item on a strategic plan. It’s a survival imperative. This is about creating smarter, more resilient systems that genuinely support your staff and lead to better patient outcomes, all without compromising the quality of care. Forget abstract theories; this guide is built on actionable strategies you can implement.
Why Bother With Operational Efficiency Now?
The pressure on healthcare systems has never been more intense. For too long, hospitals have been getting by with outdated manual workflows and siloed technologies, but that approach simply isn't cutting it anymore. We're facing a tough reality of tight budgets, persistent staff shortages, and rising patient demands, which makes operational excellence non-negotiable.
This isn't just a local problem; it's a challenge healthcare leaders are tackling worldwide. A 2024 survey from Deloitte found that over 70% of health system executives have made improving operational efficiency a top priority for 2025. This isn't surprising. It's a direct response to issues like clinician burnout and the urgent need to finally get a handle on digital health tools.
The Three Pillars You Can Actually Control
When you start to unpack this challenge, it really comes down to three core areas where you can make a real difference. Each one is a massive opportunity for meaningful change.
- Your People: An engaged and supported workforce is your most valuable asset, period. We have to address burnout head-on and start involving our frontline staff in the process of making things better.
- Your Processes: Think about all the clunky workflows, from patient discharge to managing the supply chain. These are the bottlenecks that drain your resources and frustrate your team.
- Your Technology: The right technology acts as the connective tissue for a modern hospital. It's what breaks down departmental silos and automates the monotonous tasks that bog everyone down.
The old way of doing things is buckling under the pressure. True hospital operational efficiency isn’t achieved by asking staff to work harder, but by building systems that empower them to work smarter.
This isn't a one-and-done project. It’s about building a culture of continuous improvement where decisions are guided by data, not by gut feelings. By focusing on these three pillars—your people, processes, and technology—you can shift from constantly putting out fires to proactively building a more effective and resilient healthcare environment for everyone. The next sections will show you how.
Finding and Fixing Your Hidden Bottlenecks
You can't improve what you don't measure. The first real step toward a more efficient hospital is hunting down the hidden bottlenecks that are slowing you down. These aren't always the obvious problems; they often lurk in chaotic discharge processes, underused operating rooms, or even wasted supplies. The trick is to stop putting band-aids on the symptoms, like long wait times, and dig deeper to find the root cause.
A 2025 survey shows just how tangled these issues can get. While 39% of hospital leaders named maintaining quality care their top clinical concern, 30% pointed directly to capacity problems like extended patient stays. On the financial side, workforce management was the biggest headache for 34% of executives, with supply costs and OR efficiency also being major pain points. It's worth a look at the full 2025 hospital operations report to see the complete picture.
This visual gives you a great starting point for what to track.
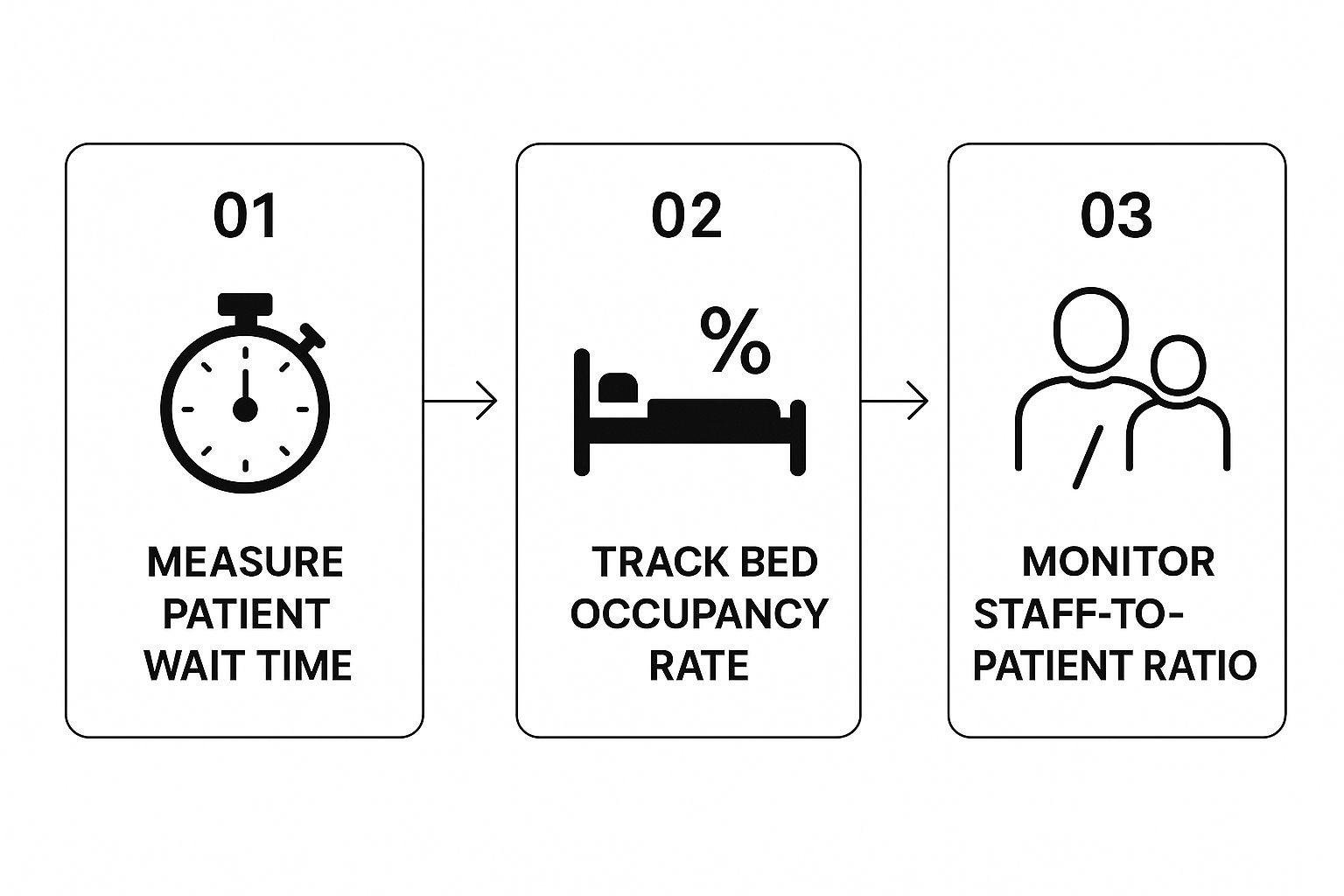
You can see how everything is connected—from wait times to bed occupancy and staff ratios. One small inefficiency can create a domino effect that ripples through the entire hospital.
How to Actually Uncover Inefficiencies
To get started, you need a solid diagnostic plan. It's time to move past guesswork and adopt a data-first mindset. This often begins with something called process mapping, which is basically drawing out every single step a patient takes from the moment they walk in the door to when they leave.
- Map the Patient Journey: Pick a department, like the ER, and literally trace a patient's path. Document every interaction, handoff, and delay you find. Where are they waiting? Who are they waiting for?
- Talk to Your Team on the Floor: Your nurses, techs, and admin staff live with these process hiccups every single day. Their firsthand experience is gold for finding out where things really break down.
- Drill Down into Your Metrics: Take a hard look at your data. What are your bed turnover rates? How about OR utilization and the average length of stay? Look for the outliers and find out which departments are consistently missing their targets.
Finding the true source of a delay—whether it’s a backlog in the lab or a slow room cleaning crew—is the only way to create a targeted fix that actually sticks.
Once you’ve identified a few bottlenecks, a good guide on streamlining medical operations can offer some practical solutions. By combining process mapping with hard data and feedback from your team, you'll have a powerful toolkit for making real, meaningful improvements to your hospital's efficiency.
How to Use Technology to Work Smarter, Not Harder

Adopting new technology is easily the most powerful lever you have for boosting hospital operational efficiency. But here's the catch: smart implementation is everything. The goal isn’t to just pile on more software. It's about carefully choosing digital tools that solve specific, real-world problems for your clinical and administrative teams.
A modern Hospital Information System (HIS) is a perfect example of this principle in action. I like to think of it as the central nervous system for the entire facility. When it's well-integrated, an HIS breaks down the frustrating communication silos between departments. Suddenly, patient data, lab results, and scheduling information flow seamlessly. This connectivity gets rid of redundant data entry and, more importantly, gives clinicians a complete, real-time view of their patients.
The sheer investment in these systems tells you how much value they bring. The global HIS market is on track to explode from $63.80 billion in 2024 to over $116.75 billion by 2030. That growth isn't just about chasing trends; it’s fueled by a clear need to improve everything from clinical decisions to the revenue cycle. You can learn more about the global trends in hospital information systems to see how they're reshaping healthcare.
To illustrate how different technologies work together to drive efficiency, I've put together a table outlining some of the most impactful tools available today.
Key Technologies for Enhancing Hospital Efficiency
This table highlights core technologies, what they actually do to improve hospital operations, and the key performance indicators (KPIs) they help move in the right direction.
| Technology | Primary Function | Impact on KPIs |
|---|---|---|
| Hospital Information System (HIS) | Centralizes patient data, scheduling, and billing into one unified platform. | Reduces administrative errors, improves billing accuracy, shortens patient wait times. |
| Predictive Analytics (AI) | Forecasts patient admissions, staffing needs, and disease outbreaks. | Optimizes staff-to-patient ratios, reduces overtime costs, improves resource allocation. |
| Telehealth Platforms | Enables remote patient consultations, follow-ups, and monitoring. | Lowers readmission rates, increases patient access to care, improves bed turnover. |
| Automated Inventory Management | Tracks supply usage in real time and automates reordering processes. | Prevents stockouts of critical items, reduces waste, cuts supply chain costs. |
Each of these technologies tackles a specific operational bottleneck, leading to a more streamlined and resilient healthcare environment.
Going Beyond the Basics with AI and Telehealth
Once you have a solid HIS foundation, artificial intelligence and automation can deliver some truly impressive results. These aren't futuristic ideas anymore; they are practical tools making a difference today.
- Predicting Patient Surges: AI algorithms can chew through historical admission data, local health trends, and even public events to forecast patient volume. This allows you to staff up before a crisis hits, avoiding burnout and chaos.
- Automating the Supply Closet: Smart systems can track supply usage down to the last bandage and automatically reorder items before they run low. This means no more expensive rush orders and no more hunting for critical supplies during an emergency.
There's a common misconception that technology is here to replace human expertise. From what I've seen, the best technology augments it. It frees up your skilled professionals from tedious, repetitive tasks so they can focus on what they do best: high-value clinical work.
Finally, telehealth is completely reshaping how we deliver care. Offering virtual follow-up appointments isn't just a convenience; it's a strategy. It can dramatically reduce readmissions, ease the pressure on your physical beds, and give patients the flexible care they've come to expect.
Every one of these advancements is a strategic investment in a more efficient and resilient hospital. When you make smart choices here, you'll see a clear and measurable return—not just on the balance sheet, but in higher staff morale and better patient outcomes.
Empowering Your Team to Drive Efficiency

When we talk about hospital operational efficiency, it's easy to get lost in technology and complex processes. But at the end of the day, true efficiency comes down to your people. Your clinical and administrative staff are on the front lines, and they’re the ones who hold the real keys to making lasting improvements.
Too often, though, they’re held back by burnout, bureaucracy, and the frustrating feeling that their expertise isn't being heard.
A human-first approach is the only way forward. This means getting ahead of staffing crises instead of just reacting to them. By using data to better predict patient flow and demand, you can build smarter schedules that align your team's presence with actual patient needs. This simple shift can dramatically reduce the expensive reliance on temporary agency staff, which drains budgets and can disrupt team dynamics.
Tap Into Your Frontline Experts
Some of the most brilliant ideas for improvement won't come from a boardroom—they'll come from the people doing the work every single day. The nurse on the floor knows precisely where patient handoffs break down. The lab technician sees firsthand which workflows create frustrating delays. The real challenge isn't finding problems; it's creating a system that actually listens to these insights and empowers your team to act on them.
Instead of issuing top-down directives, you need to cultivate innovation from the ground up. Here’s how you can start:
- Open up formal feedback channels where staff can suggest process improvements without any fear of pushback.
- Form cross-departmental "strike teams" to zero in on specific issues, like cutting down ER wait times or smoothing out the discharge process.
- Publicly celebrate and reward the individuals and teams whose ideas result in real, measurable gains in efficiency or patient care.
A culture that values frontline expertise does more than just fix problems—it boosts morale, improves staff retention, and shows every employee they have a stake in the hospital's success.
Empowering your team also means giving them the best tools and training available. Think about how interactive video can be a powerful asset for improving surgical decision-making, helping ensure your clinicians walk into procedures feeling confident and fully prepared.
When you genuinely bring your clinical teams into the improvement process, they stop being passive participants and become active drivers of change. This shift gives them more ownership over their work, directly combating burnout and building a more resilient organization that’s ready for whatever comes next.
Weaving Data-Driven Decisions into Your Daily Rhythm

While intuition and experience are invaluable in healthcare, they simply can't guide an entire facility. To really boost your hospital operational efficiency for the long haul, you need to move beyond putting out fires and embrace a culture where data informs your every move. It’s all about turning raw numbers into your most reliable tool for improvement.
The first step is figuring out which key performance indicators (KPIs) genuinely signal your hospital’s health. Forget vanity metrics. You need actionable numbers that shine a light on the real friction points in your daily operations.
Key Operational KPIs to Keep an Eye On
To build a data-first culture, everyone needs to be on the same page, looking at the same core numbers. Here are some of the most critical metrics that give you an honest snapshot of performance:
- Average Length of Stay (ALOS): This classic KPI shows you how quickly patients move through your system, which directly ties into bed availability and overall capacity.
- Bed Turnover Rate: A high turnover rate is a great sign. It means your discharge, cleaning, and admission processes are running like a well-oiled machine, maximizing how many patients you can serve.
- Operating Room Utilization: Your ORs are some of your most expensive assets. This metric tells you if you're making the most of that valuable space and staff time, or if there's room to tighten up surgical scheduling.
- Emergency Department Wait Times: This is a huge factor in patient satisfaction and a clear warning sign of bottlenecks in triage, diagnostics, or your admission workflow.
The real magic happens when this data isn't just collected but is made visible and accessible to the teams on the ground. A real-time dashboard can turn a manager's daily huddle from a guessing game into a focused, strategic planning session.
Think about it this way: a department head who can see admission trends from the last few weeks can accurately forecast staffing needs for an upcoming holiday weekend. That means no more last-minute scrambling, costly overtime, or burned-out staff.
Or, if a dashboard shows the cardiology department consistently has the longest wait times, leadership can dig in to find the root cause. Is it a scheduling snag? A diagnostic machine that’s always booked? A staffing gap? The data points you toward the right questions.
To take this a step further, many hospitals formalize their data collection with specialized tools. Exploring a solution like healthcare survey software can give you the power to gather nuanced feedback, turning abstract numbers into a concrete action plan for making things better.
Answering Your Top Efficiency Questions
Navigating the path to better hospital operational efficiency can feel overwhelming. To help clear things up, we’ve tackled some of the most pressing questions hospital leaders ask when starting this journey. Here are direct answers to guide your strategy.
Where Should Our Hospital Even Start?
The best first step is a thorough operational assessment. Don't guess where the problems are—use data. Begin by mapping the complete patient journey from admission to discharge to identify your most critical bottlenecks. This means analyzing hard metrics like wait times, room turnover, and resource usage in high-traffic areas like the ER and operating rooms.
Most importantly, involve your frontline staff. Their firsthand insights are invaluable for pinpointing the day-to-day workflow frustrations that data alone can't show. They know what truly slows things down.
How Can We Adopt New Technology Without Chaos?
A phased rollout is non-negotiable for success. Start with a pilot program in a single, controlled department. This approach allows you to test the technology, refine the workflow, and fix bugs on a small scale before they impact the entire hospital.
Invest heavily in staff training before you go live and provide dedicated, on-site support during the transition. Constant communication about how the new system benefits both staff and patients is essential for getting everyone on board and ensuring smooth adoption.
The biggest mistake hospitals make is focusing solely on technology while ignoring the people and processes. Buying a new system without redesigning the workflow around it or properly training the staff who use it is a recipe for failure.
True efficiency comes from a holistic approach where technology supports optimized processes and an empowered workforce. Ignoring the human element is the fastest way to ensure your investment doesn't pay off.
How Do We Actually Measure ROI on These Initiatives?
To measure your return on investment, you must track a balanced mix of financial, operational, and clinical KPIs. Comparing these metrics before and after your changes will clearly demonstrate the tangible value of your efforts.
- Financial ROI: Look at reduced overtime costs, lower supply waste, and a faster revenue cycle.
- Operational ROI: Measure direct improvements in patient wait times, bed turnover rates, and OR utilization.
- Clinical ROI: Don't forget to track patient satisfaction scores and improved health outcomes.
This comprehensive view proves that your initiatives are not only saving money but also enhancing the quality of care and staff satisfaction. It creates a powerful case for continued investment in improving hospital operational efficiency.
At PYCAD, we specialize in integrating AI to refine medical imaging processes, directly improving diagnostic accuracy and operational workflows. If you're looking to enhance your medical devices with proven AI solutions, explore how we can help at PYCAD.