Understanding the Healthcare AI Revolution (It's Happening Now)
The healthcare AI revolution isn't a distant prospect; it's unfolding right now. Progressive healthcare organizations are actively integrating AI into their daily operations, moving beyond preliminary exploration to practical implementation. This shift is fueled by both growing risk tolerance among healthcare leaders and the continuous advancement of AI technologies, making a compelling argument for adopting AI in healthcare today.
Why the Shift Is Happening Now
AI adoption in healthcare is surging. 80% of hospitals globally are currently utilizing AI to enhance patient care and streamline medical workflows, as reported in Deloitte's 2024 Health Care Outlook. This signifies a substantial increase from just a few years prior when AI was primarily confined to research environments. Furthermore, 46% of U.S. healthcare organizations are in the initial phases of implementing generative AI, indicating widespread acceptance of this technology across the sector. More detailed statistics are available here: Learn more about AI in healthcare statistics. This rapid uptake highlights the growing acknowledgement of AI's potential to transform healthcare.
Tangible Benefits Driving Adoption
The advantages of AI in healthcare extend well beyond theoretical potential. The infographic below visually represents the tangible improvements AI can offer:
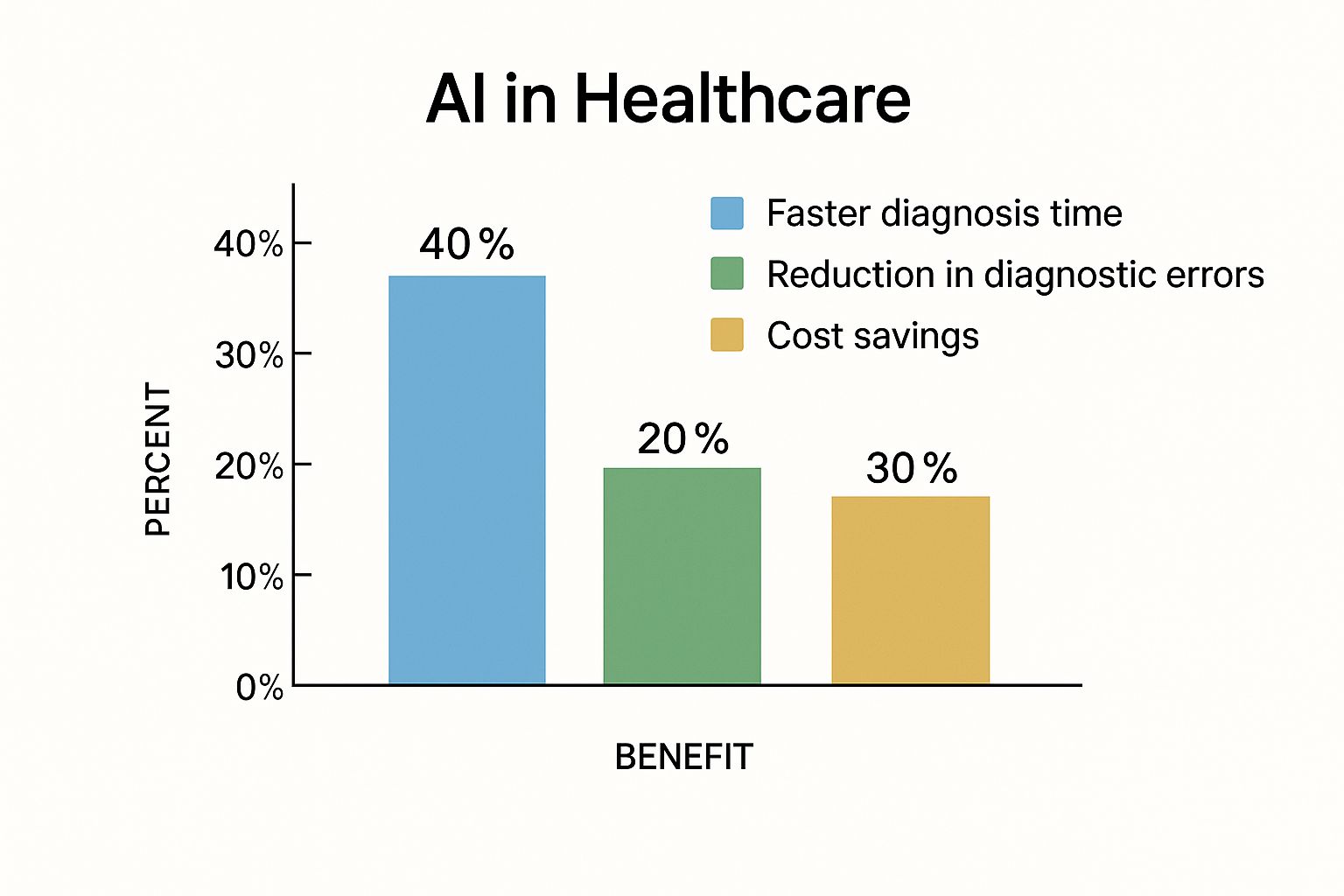
As the infographic shows, AI implementation can result in a 40% reduction in diagnosis time, a 20% decrease in diagnostic errors, and 30% in cost savings. These enhancements not only improve the quality of care provided but also contribute to increased efficiency and resource optimization within healthcare systems. For successful AI scaling, focus on key performance indicators. This article provides valuable insights: measuring productivity in healthcare.
The Competitive Landscape
The widespread integration of AI is reshaping healthcare's competitive landscape. Organizations embracing AI gain a substantial advantage by improving patient outcomes and optimizing operational effectiveness. However, implementing AI is not merely about acquiring the latest technology; it necessitates a strategic approach that considers the unique needs and obstacles of each organization.
To understand how AI adoption varies across the globe, let's look at the following table:
Global Healthcare AI Adoption by Region
| Region | Adoption Rate | Primary Use Cases | Investment Level |
|---|---|---|---|
| North America | High (75-85%) | Drug discovery, diagnostics, personalized medicine | High |
| Europe | Moderate (50-60%) | Imaging analysis, remote patient monitoring, electronic health records | Moderate |
| Asia-Pacific | Moderate (45-55%) | Robotics, telehealth, predictive analytics | High (growing rapidly) |
| Latin America | Low (25-35%) | Telemedicine, public health management | Moderate (increasing) |
| Africa | Low (15-25%) | Disease surveillance, access to care | Low (potential for growth) |
Note: These are estimated ranges based on current market trends and publicly available data.
The table above provides a general overview of AI adoption in different regions. North America currently leads in both adoption and investment, while other regions are showing significant growth potential. The primary use cases also vary based on regional needs and priorities.
Finding Your Optimal Starting Point
Determining the appropriate time to implement AI is critical. This involves evaluating your organization's preparedness, identifying high-impact use cases, and establishing a pragmatic implementation roadmap. While the swift pace of AI adoption may create a sense of urgency, a thoughtful and strategic approach is essential to fully capitalize on the advantages AI offers in healthcare. Careful planning will ensure AI implementation aligns with your organization's broader objectives and contributes to long-term success.
Real Results That Make AI Implementation Worth It
Forget far-off promises. Let's explore the tangible benefits healthcare organizations are experiencing with AI. This isn't science fiction; it's about practical, measurable improvements happening now.
Quantifiable Gains: Beyond Automation
AI in healthcare goes beyond simple automation. It's about fundamentally improving diagnosis, treatment, and patient care management. These improvements lead to real-world results, justifying the investment.
-
Increased Efficiency: AI streamlines workflows, giving healthcare professionals more valuable time. This means more time with patients and less time on administrative tasks.
-
Improved Diagnostic Accuracy: AI-powered diagnostic tools help clinicians make more accurate diagnoses. This leads to better patient outcomes and fewer medical errors, enhancing the quality of care and increasing cost efficiency.
-
Early Disease Detection: AI algorithms analyze patient data to identify early warning signs of diseases. This allows for timely intervention and potentially life-saving treatment, enabling earlier detection of conditions like cancer or Alzheimer's.
Demonstrated Success: Real-World Examples
AI implementation in healthcare has demonstrably improved operational efficiency and patient outcomes. For example, AtlantiCare reports saving 66 minutes per provider daily by automating documentation and reducing paperwork. This increased efficiency reduces staff burnout and prioritizes patient care. AI-driven diagnostic tools are also revolutionizing early disease detection. Conditions like Alzheimer's and diabetes can now be predicted using advanced analytics. Learn more about the impact of AI: Explore this topic further. These examples highlight AI's potential to not just improve care, but transform the healthcare system.
Calculating ROI: Demonstrating Value
Demonstrating a clear return on investment (ROI) is crucial for securing buy-in and justifying AI implementation. Focus on metrics that are most important to your organization.
-
Reduced Operational Costs: Track cost savings from improved efficiency, reduced errors, and optimized resource allocation.
-
Improved Patient Outcomes: Measure improvements in patient satisfaction, reduced readmission rates, and enhanced treatment efficacy.
-
Increased Staff Satisfaction: Evaluate AI's impact on staff workload, burnout levels, and overall job satisfaction.
Setting Benchmarks: Measuring Progress
Establishing realistic benchmarks is essential for tracking progress and demonstrating AI's value. These benchmarks should align with your organizational goals and the specific metrics you want to improve. For instance, if your goal is to reduce patient wait times, set a target reduction percentage and track your progress. This quantifies AI's impact and demonstrates its value to stakeholders.
From Pilot Programs to System-Wide Integration: Scaling Strategically
Successful AI implementation requires a phased approach. Start with targeted pilot programs to demonstrate value and refine processes. Then, strategically scale successful initiatives across departments and facilities. This measured approach allows for continuous improvement and seamless integration with existing infrastructure. Implementing AI in stages maximizes benefits while minimizing disruption and allows for adjustments. Building a strong foundation for AI integration is essential for long-term success and adaptability.

Sustained Success: Continuous Optimization
Implementing AI is an ongoing journey. Continuous monitoring, evaluation, and optimization are key to sustained success. Regularly assess AI system performance, gather user feedback, and identify areas for improvement. This iterative process ensures that AI remains aligned with evolving healthcare needs and delivers maximum value. Regularly evaluating and adapting AI systems maintains their effectiveness and relevance in the ever-changing healthcare landscape, ensuring your investment continues to yield positive returns for your organization and your patients.
Building Your Strategic Foundation (Before You Touch Technology)
Successfully integrating AI into healthcare requires more than just the technology itself; it demands a well-defined strategic plan. Think of it as constructing a building: a visually appealing exterior won't last without a solid foundation. This section details the crucial groundwork needed to distinguish AI success stories from costly failures.
Assessing Your Readiness: An Honest Evaluation
Before starting implementation, a comprehensive readiness assessment is crucial. This involves evaluating your current infrastructure, data capabilities, and organizational culture. Do you have the necessary data storage and processing power? Is your team ready for the changes AI will introduce? A frank self-assessment will highlight areas needing improvement before you begin.
Identifying High-Impact Use Cases: Focusing on Value
Not all AI applications are the same. Prioritize use cases that offer the most significant potential benefits. Consider areas where AI can drastically improve patient care, optimize operations, or lower costs. For instance, AI-powered diagnostic tools can improve accuracy and speed, while predictive analytics can optimize resource allocation and prevent hospital readmissions.
Creating Realistic Timelines: Avoiding Unrealistic Expectations
Implementing AI requires time. Develop a practical timeline that considers potential setbacks and unforeseen difficulties. Divide the project into manageable phases, with clear milestones and deliverables. This approach helps manage expectations and sustain momentum. Organizations with comprehensive strategic planning are 73% more likely to achieve their AI objectives and experience 45% fewer costly setbacks compared to those who rush into technology implementation. Learn more about healthcare AI planning here.
Engaging Stakeholders: Building Consensus and Managing Resistance
Implementing AI affects everyone in a healthcare organization. Engaging all stakeholders, from clinicians to IT staff, is essential. Address concerns, offer training, and communicate the advantages of AI transparently. This fosters support and minimizes resistance to change.
Establishing Governance Frameworks: Ensuring Ethical and Compliant AI
AI in healthcare must be ethical and comply with all regulations. Establish clear governance frameworks that address data privacy, algorithm bias, and responsible AI usage. This builds trust with patients and staff, ensuring the long-term viability of your AI initiatives.
Navigating Change Management: Preparing for the Human Factor
Implementing AI represents substantial change, making change management crucial. Communicate regularly with staff, offer continuous support, and address any concerns proactively. This minimizes disruption, encourages acceptance, and helps individuals adjust to new AI-driven workflows. Effective change management makes the shift to AI-powered systems smooth and efficient for everyone. This section has established the foundation for successful AI implementation. Next, we'll explore selecting technology that genuinely aligns with your organization's specific requirements.
Choosing Technology That Actually Works For Healthcare
The sheer number of AI vendors can feel overwhelming for healthcare organizations. Finding the right technology partner requires a strategic approach, focusing on practical needs and proven results rather than marketing promises. This section provides a framework for evaluating AI vendors, emphasizing key factors for successful implementation.
Key Evaluation Criteria for AI Vendors
When evaluating AI vendors, look beyond the surface-level presentations. Instead, prioritize clinical validation, integration capabilities, and long-term viability. Clinical validation ensures the solution has been rigorously tested and delivers proven outcomes in real-world healthcare settings. Seamless integration with existing systems like Electronic Health Records (EHR) is crucial for efficient workflow and minimizing disruptions. Assessing the vendor's long-term viability guarantees ongoing support and reduces the risk of outdated technology.
Deployment Models: Cloud Vs. On-Premise
Choosing the right deployment model – cloud-based or on-premise – is a crucial decision. Cloud-based solutions offer scalability and cost-effectiveness, while on-premise solutions provide greater control over data and security. Healthcare leaders must weigh these trade-offs carefully, considering organizational needs, resources, and risk tolerance. The optimal approach aligns with your specific circumstances.
Seamless Integration: Connecting With Your Existing Infrastructure
Integrating AI into existing healthcare infrastructure requires meticulous planning and execution. Seamless integration prevents workflow disruptions and maintains data consistency. Collaboration with IT directors and clinical leaders is essential to navigate the intricacies of existing systems, including EHRs, medical devices, and clinical workflows. This collaborative approach ensures the AI solution enhances, not hinders, current processes.
Calculating the True Total Cost of Ownership
Understanding the total cost of ownership (TCO) is vital for successful AI implementation. TCO extends beyond the initial purchase price, encompassing long-term expenses such as training, maintenance, and ongoing support. These hidden costs can significantly impact the budget. Investing in comprehensive staff training ensures effective technology utilization. Regular maintenance keeps the AI system operating at peak performance. Reliable vendor support addresses technical issues and provides essential updates.
Best Practices for Long-Term Success
Several best practices contribute to long-term success with AI in healthcare:
-
Pilot Programs: Begin with small-scale pilot programs to test and refine the technology before widespread deployment.
-
Change Management: Implement a robust change management strategy to address staff concerns and promote smooth adoption.
-
Data Governance: Establish clear data governance protocols to ensure data quality, privacy, and security.
To help illustrate the differences between deployment models, the following table summarizes the key distinctions:
AI Healthcare Solution Comparison Matrix: Feature and capability comparison of different types of AI healthcare solutions including diagnostic tools, workflow automation, and predictive analytics
| Solution Type | Implementation Time | ROI Timeline | Integration Complexity | Use Cases |
|---|---|---|---|---|
| Diagnostic Tools (Cloud-Based) | 3-6 months | 12-18 months | Moderate | Image analysis, disease detection |
| Workflow Automation (On-Premise) | 6-12 months | 18-24 months | High | Appointment scheduling, patient record management |
| Predictive Analytics (Cloud-Based) | 6-9 months | 15-21 months | Moderate | Risk prediction, personalized treatment plans |
This comparison matrix highlights the varied implementation times, ROI timelines, and integration complexities associated with different AI healthcare solutions. Choosing the right solution depends on specific organizational needs and desired outcomes. Carefully considering these factors upfront enables successful implementation and maximizes the benefits of AI in healthcare settings.
Overcoming the Challenges Everyone Faces (But No One Talks About)

Implementing AI in healthcare offers incredible potential. However, it also presents unique challenges. Even with the best planning, obstacles will arise. This section explores these common challenges and offers practical strategies for successfully navigating them. By understanding these difficulties upfront, we can build more robust and effective AI solutions.
Data Quality and Interoperability: The Foundation of Effective AI
AI algorithms rely heavily on high-quality data. Unfortunately, healthcare data is often fragmented, incomplete, and inconsistent. This presents a significant challenge for effective AI implementation. Furthermore, ensuring interoperability between various systems—like electronic health records (EHRs) and medical devices—is crucial for data aggregation and analysis. This requires thorough planning and strong data governance frameworks.
Security and Privacy: Protecting Sensitive Patient Information
Healthcare data is highly sensitive, requiring strict security and privacy measures. AI implementation must not compromise these protections. Balancing functionality with robust security protocols is essential. This includes implementing strong encryption, access controls, and audit trails. Adhering to regulations like the Health Insurance Portability and Accountability Act (HIPAA) is paramount.
Change Management: Addressing Staff Resistance and Building Confidence
One of the biggest hurdles in implementing AI in healthcare is staff resistance. Clinicians may be hesitant about AI-driven recommendations or worried about workflow changes. Research indicates that 68% of healthcare AI implementations encounter significant staff resistance. Organizations with structured change management programs, however, experience significantly improved outcomes, reducing resistance by 84% and increasing user adoption rates by 3.2 times. More detailed statistics can be found here. Effective change management involves clear communication, comprehensive training, and proactively addressing concerns. Building trust and demonstrating AI's value to clinical staff is critical for successful adoption. When selecting AI technology, consider AI tools for ecommerce as a resource for understanding best practices in technology selection and implementation.
Managing Vendor Relationships: Navigating the Complex AI Landscape
The AI vendor landscape can be complicated. Choosing the right vendor and effectively managing the relationship requires careful evaluation. Establish clear expectations, communication channels, and performance metrics. Negotiating service-level agreements (SLAs) for system uptime and support is critical for minimizing disruptions.
Handling System Downtime and Maintaining Business Continuity
System downtime is unavoidable. Contingency plans are essential for maintaining business continuity during critical implementation phases. These plans should include backup systems, disaster recovery procedures, and clear communication protocols. Minimizing disruption during downtime protects patient care and ensures smooth operations.
Practical Approaches for Long-Term Success
Overcoming these challenges requires a proactive and strategic approach. Here are some key takeaways:
- Proactive Planning: Anticipate potential obstacles and develop mitigation strategies.
- Open Communication: Maintain transparent communication with all stakeholders.
- Continuous Monitoring: Regularly evaluate AI system performance and identify areas for improvement.
- Iterative Approach: Implement AI in stages, allowing for adjustments and refinements.
By addressing these challenges directly and adopting these practical approaches, healthcare organizations can unlock AI's full potential. This proactive approach enables efficient adaptation and paves the way for a more efficient and effective future for AI in healthcare.
Measuring What Matters and Scaling Smart
Implementing AI in healthcare is a journey, not a destination. True success depends on continuous measurement, optimization, and smart scaling that goes beyond basic usage statistics. Instead of simply tracking how often an AI tool is used, we need to focus on its real-world impact. This section explores proven frameworks from successful healthcare organizations to help you measure what matters and scale intelligently.
Establishing Meaningful Metrics: Focusing on Real Impact
The first step is establishing Key Performance Indicators (KPIs) that accurately reflect AI's influence on patient outcomes and operational efficiency. These metrics should align with your organization's strategic goals. For example, if reducing hospital readmissions is a primary goal, track how AI-driven predictive models impact those rates. If improving diagnostic accuracy is paramount, measure how AI tools affect the rate of accurate diagnoses. By focusing on outcomes, you demonstrate the true value of your AI investment.
Creating Actionable Dashboards: Visualizing Progress and Identifying Areas for Improvement
Data is only valuable if it's accessible and understandable. This is where effective dashboards become essential. These dashboards should visually represent your chosen KPIs, offering actionable insights for clinical and business decisions. Stakeholders can quickly grasp the impact of AI and identify areas for improvement. A dashboard could, for instance, track the reduction in diagnostic errors achieved through an AI-powered imaging tool. This visual representation of success justifies continued AI investment and highlights areas needing adjustments.
Continuous Improvement: A Cycle of Feedback and Optimization
AI implementation requires a mindset of continuous improvement. Regularly gather user feedback from clinicians, IT staff, and other stakeholders to identify optimization opportunities. This feedback loop is crucial. For example, if clinicians find an AI tool's interface cumbersome, it can hinder adoption. Addressing this feedback through iterative enhancements ensures the system remains user-friendly and effective. Constant refinement maximizes the long-term benefits of AI.
Scaling Strategically: Expanding Success Across the Organization
After establishing a successful AI initiative, the next step is strategic scaling. This involves expanding implementation to other departments, facilities, or use cases while maintaining quality and consistency. This isn't simply replication. It requires careful consideration of each new environment's unique needs and challenges. A successful AI-powered diagnostic tool in cardiology, for instance, may require adaptations before deployment in oncology.
Building Organizational Capabilities: Supporting Long-Term AI Innovation
Sustained success with AI in healthcare requires building robust organizational capabilities. This includes investing in training programs to develop in-house AI expertise, fostering data-driven decision-making, and establishing governance frameworks for ethical and responsible AI usage. This proactive approach creates a resilient and adaptable organization, laying the foundation for ongoing innovation and adaptation to new technologies. It allows you to leverage the full potential of AI now and in the future.
Key Takeaways for Measuring and Scaling AI
- Focus on Outcomes: Measure AI's impact on patient care and operational efficiency, not just usage.
- Visualize Progress: Create dashboards providing actionable insights for clinical and business decisions.
- Embrace Feedback: Continuously gather user feedback to identify optimization opportunities and enhance AI systems.
- Scale Strategically: Expand successful initiatives while maintaining quality and consistency.
- Invest in Capabilities: Build organizational expertise and frameworks to support long-term AI innovation and adaptation.
Ready to transform your medical imaging workflows with AI? PYCAD offers solutions for data handling, model training, and deployment, helping you achieve enhanced diagnostic accuracy and operational efficiency. Visit PYCAD today to learn more.






