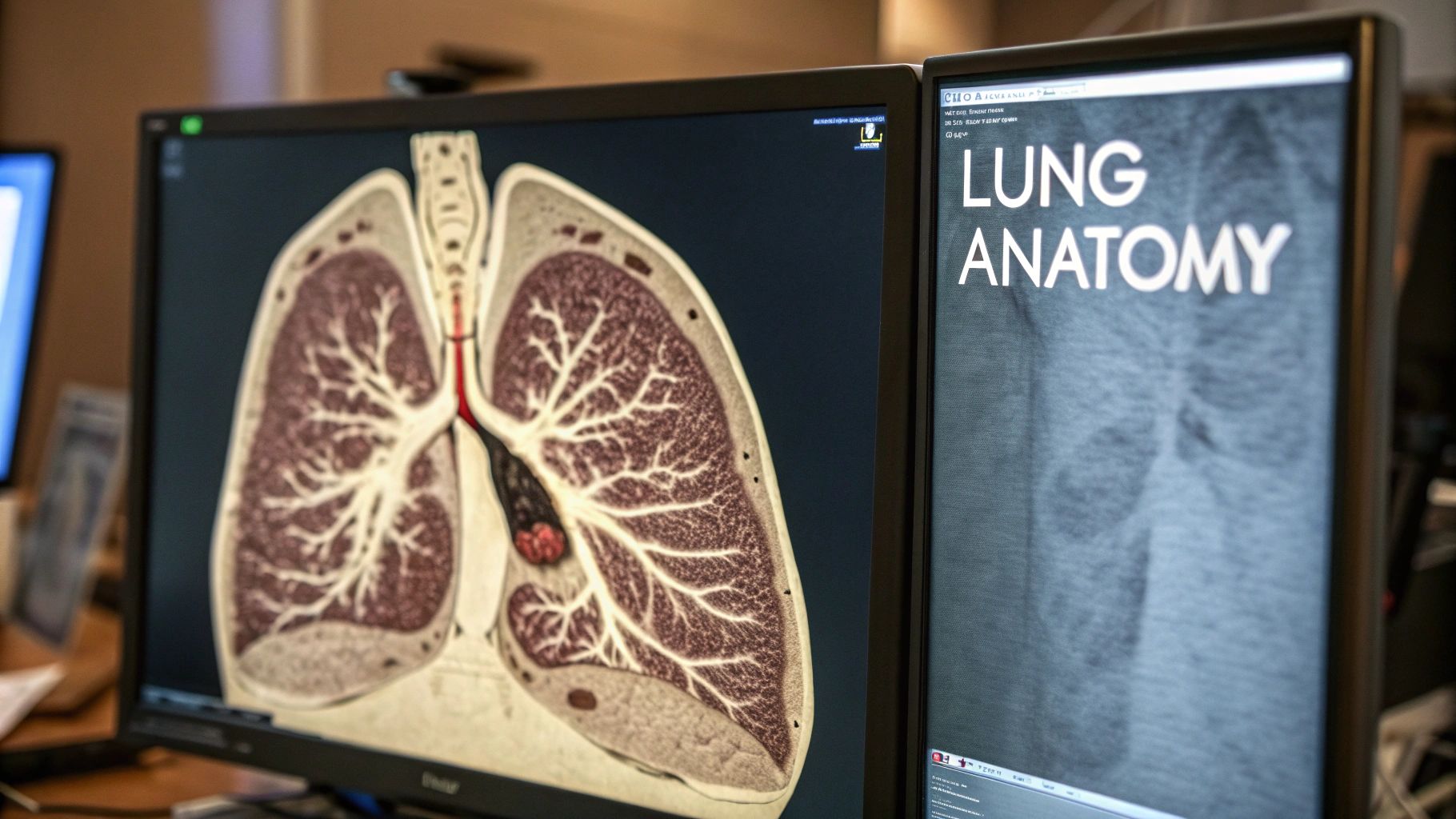
Decoding Lung Segments on CT: Foundational Anatomy
Understanding lung segments on CT scans begins with a firm grasp of bronchopulmonary anatomy. Imagine the lungs as an inverted tree: the trachea, the trunk, branches into the right and left main bronchi. These bronchi divide into progressively smaller airways, ultimately reaching the bronchopulmonary segments. These segments, the "leaves" of our tree, are the fundamental units we strive to identify on CT.
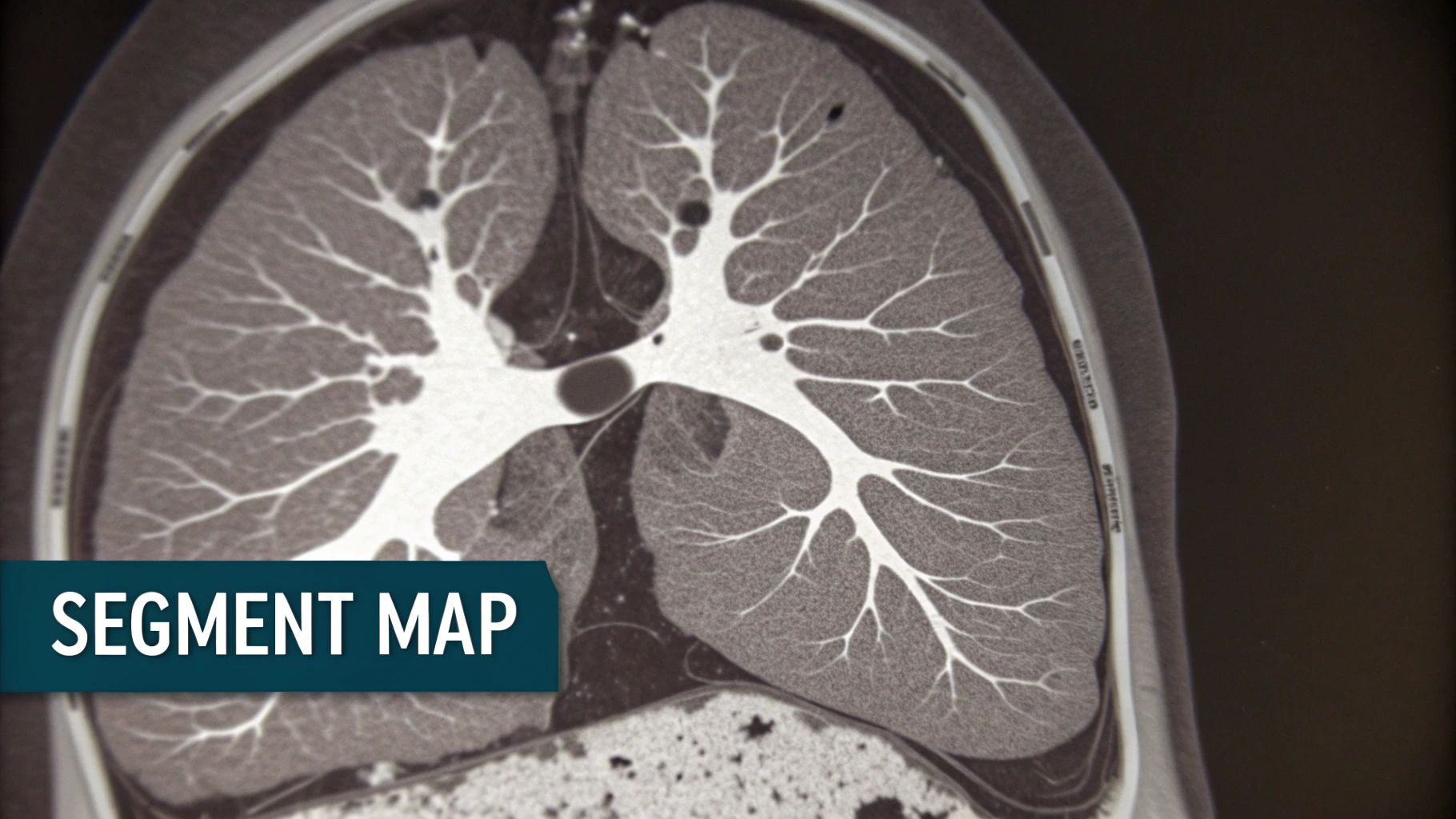
Visualizing Segments in Different Planes
Analyzing lung segments requires navigating different anatomical planes. The axial plane, a view from above, provides a cross-section. This is ideal for pinpointing segmental bronchi and vessels.
The coronal plane, like viewing the lungs from the front, shows the superior and inferior relationships between segments, revealing how they stack.
The sagittal plane, a side view, illustrates anterior-posterior relationships, distinguishing segments in close proximity.
Anatomical Landmarks and Visual Cues
Identifying segments relies on recognizing subtle visual cues. Fissures, thin walls of connective tissue, partially separate lobes, serving as key landmarks. However, incomplete or absent fissures can complicate identification.
Variations in branching patterns and segmental anatomy further add to the complexity. This variability highlights the importance of experience and keen observation when interpreting CT scans.
Identifying lung segments hinges on their bronchial divisions. CT scans excel at visualizing segmental bronchi, essential for understanding lung anatomy and pathology. A study documented 665 individual segmental bronchi across patients, demonstrating the variability and visualization completeness. Read the full research here.
This detailed visualization is invaluable for diagnosing and managing lung diseases, particularly when segmental involvement is crucial. Advancements in CT technology and image analysis have greatly improved segment identification, leading to more accurate diagnoses and treatment plans.
In the right lung, some segments like RB4 and RB5 are visualized in roughly 60% of cases, while others, such as RB1, RB2, and RB6, are seen in up to 80% of cases. This granularity improves our understanding of lung diseases and facilitates targeted interventions.
To provide a clearer overview of visibility rates, let's look at the following table:
Visibility Rates of Bronchopulmonary Segments on CT
This table compares the visibility rates of different bronchopulmonary segments on standard CT imaging.
| Lung Segment | Visibility Rate (%) | Key Identifying Features |
|---|---|---|
| RB1 | ~80% | Posterior, adjacent to trachea |
| RB2 | ~80% | Posterior, superior to RB1 |
| RB3 | ~70% | Anterior, adjacent to right atrium |
| RB4 | ~60% | Lateral, adjacent to right middle lobe |
| RB5 | ~60% | Medial, adjacent to RB4 |
| RB6 | ~80% | Inferior, near diaphragm |
| LB1+2 | ~75% | Apicoposterior, combined segment |
| LB3 | ~70% | Anterior, adjacent to left ventricle |
| LB4 | ~65% | Superior lingular segment |
| LB5 | ~65% | Inferior lingular segment |
| LB6 | ~75% | Inferior, near diaphragm |
| (These are approximate values and can vary based on individual anatomy and imaging technique) |
This table summarizes the approximate visibility rates for several bronchopulmonary segments. Note the variability in visibility, especially for segments like RB4 and RB5 compared to RB1 and RB2. Understanding these differences is critical for accurate interpretation.
Visualization Strategies Used by Radiologists
Radiologists employ a combination of techniques. They trace bronchi and vessels from the hilum outward, carefully observing branching patterns. They analyze the shape and location of each segment, comparing it to adjacent segments. This comparative analysis, combined with knowledge of anatomical variations, increases accuracy. These skills are particularly important when pathology distorts normal anatomy. This understanding lays the groundwork for applying anatomical knowledge to diagnose and manage lung diseases.
Why Lung Segments on CT Matter in Clinical Practice
Understanding lung segment anatomy is crucial for effective clinical decision-making. Accurate identification of these segments on CT scans plays a vital role in patient outcomes, impacting both diagnosis and treatment planning.
Guiding Treatment Decisions
Precise segment identification on a CT scan allows for more targeted therapies. For instance, pinpointing the exact location of an infection within a specific segment enables more focused antibiotic treatment. This reduces the need for broad-spectrum antibiotics, minimizing the risk of antibiotic resistance and mitigating potential side effects. In cases of bronchial obstruction, understanding which segment is affected guides pulmonologists in selecting the most appropriate bronchoscopic interventions.
Surgical planning also benefits greatly from segmental analysis. This is especially important in lung cancer cases. Thoracic surgeons rely on this detailed information from CT scans to plan tissue-sparing resections. By precisely targeting the affected area, they can preserve as much healthy lung tissue as possible. This approach leads to improved recovery times and fewer complications. Segmentectomy, the surgical removal of a single lung segment, exemplifies this precision.
Furthermore, evaluating individual lung segments on CT scans dramatically improves the accuracy of treatment response assessment. By monitoring changes within specific segments on follow-up scans, physicians can accurately track how well treatments like chemotherapy or radiation therapy are working. This allows for timely adjustments to the treatment plan, optimizing its effectiveness and minimizing unnecessary interventions.
The Language of Precision
Clear communication between radiologists and other healthcare professionals is essential. Radiologists utilize precise anatomical language when describing segmental involvement in their reports, accurately conveying the location and extent of the pathology. A report might state, for example, "consolidation within the apical segment of the right upper lobe (RB1)," offering a clear and concise description for the pulmonologist or thoracic surgeon.
This precise information is critical for the interdisciplinary team's decision-making process. It facilitates targeted interventions and allows the team to develop the most effective and least invasive treatment strategies for each patient.
Precise segmentation is also fundamental for monitoring disease progression and planning interventions, particularly in conditions like lung cancer. The Lung CT Segmentation Challenge, held in conjunction with the AAPM 2017 Annual Meeting, investigated the use of auto-segmentation algorithms for defining organs at risk. This challenge, involving 60 lung cancer patients, focused on accurate segmentation of lungs and tumors. You can learn more about this at The Cancer Imaging Archive. The challenge highlighted the importance of precise segmentation in a variety of clinical settings.
Impact on Patient Care
Ultimately, accurate lung segment identification on CT scans leads to tangible improvements in patient care. It enables more effective treatment planning, minimizes surgical complications, and promotes faster recovery times. The increased precision also reduces the need for unnecessary interventions, lessening the overall burden of treatment. Therefore, a deep understanding of lung segments on CT scans is not just a technical skill, but a cornerstone of high-quality patient care.
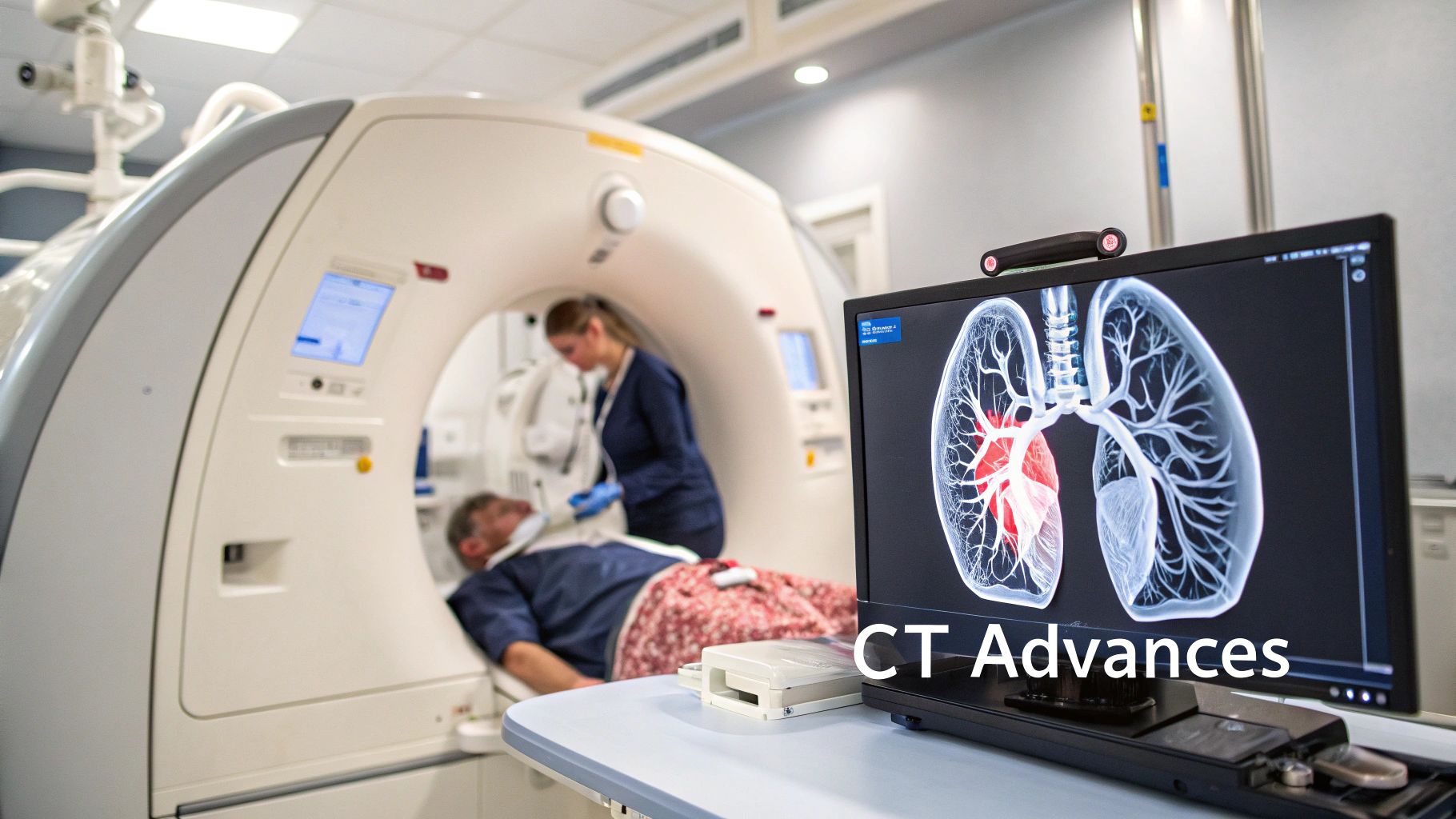
Breaking Down Advanced Segmentation Techniques for Lung CT
Accurately identifying lung segments on CT scans is crucial for diagnosis, treatment planning, and tracking disease. This requires specialized segmentation techniques, each with its own set of advantages and disadvantages. Let's explore these methods and their practical uses.
Traditional Segmentation Approaches
Traditional methods often involve manual segmentation. This is where a trained radiologist carefully outlines each lung segment on the CT scan. This method is highly accurate but can be very time-consuming, particularly with large numbers of scans or complex medical cases.
For example, segmenting lungs affected by severe emphysema, with its challenging fine details, can be particularly difficult. Another traditional approach is thresholding, which classifies image pixels based on their intensity.
This is computationally efficient but struggles with variations in image quality and the presence of diseases that affect tissue density. Thresholding might incorrectly classify inflamed areas or fluid buildup as lung tissue, leading to inaccurate segmentation.
The Rise of Automated Segmentation
The demand for faster and more efficient methods has led to the development of automated segmentation techniques. These methods use computer algorithms to analyze CT images and automatically identify lung segments. This automation significantly reduces processing time, freeing up radiologists for more complex analysis.
One such technique is region-based segmentation, which groups neighboring pixels with similar characteristics. While effective for identifying uniform areas, this method struggles with unclear boundaries or subtle differences in tissue texture. This is particularly noticeable in cases of interstitial lung disease, where fibrotic changes create a varied appearance within the lung segments.
Harnessing the Power of AI
Advancements in artificial intelligence and machine learning have revolutionized lung segmentation on CT scans. Techniques like the U-Net architecture use deep learning algorithms to analyze complex patterns and identify lung segments, even with significant disease present.
The need to efficiently analyze diverse lung conditions on CT scans has fueled the development of these techniques, including thresholding-based, region-based, shape-based, neighboring anatomy-guided, and machine learning-based approaches. Learn more about lung segmentation in this National Institutes of Health article.
Even AI-powered methods have their limitations. Segmenting complex patterns, such as cavities or consolidation, can be problematic and may lead to distorted results. This highlights the continuing need for refinement and improvement, especially when distinguishing subtle fibrotic changes from healthy lung tissue.
Choosing the Right Technique
Choosing the right segmentation approach depends on several factors. The specific clinical question plays a key role. If precise measurements of segmental volumes are required, manual segmentation might be preferred. For a quick assessment of lung involvement in pneumonia, an automated technique might be sufficient.
Image quality and time constraints are also important considerations. Automated methods are often preferred in busy medical centers that prioritize efficiency. In difficult cases with poor image quality or complex diseases, manual or AI-assisted segmentation may be necessary for accuracy.
The following table summarizes the strengths and limitations of various lung segmentation techniques:
Comparison of Lung Segmentation Methods on CT
This table compares different segmentation techniques for lung CT images based on accuracy, speed, and applicability to various pathologies
| Segmentation Method | Accuracy | Processing Time | Best Use Cases | Limitations |
|---|---|---|---|---|
| Manual Segmentation | High | Slow | Precise measurements, complex pathologies | Time-consuming, subjective |
| Thresholding | Low | Fast | Simple cases, homogenous regions | Sensitive to noise and artifacts |
| Region-Based | Moderate | Moderate | Identifying homogenous regions | Struggles with blurred boundaries |
| AI-Based (e.g., U-Net) | High | Fast | Complex pathologies, large datasets | Challenges with specific patterns (cavities, consolidation) |
This comparison highlights the trade-offs between precision, speed, and suitability of each method. Understanding these trade-offs is essential for radiologists and researchers to select the best approach for their needs. The ongoing development of segmentation techniques promises continued progress in the accuracy and efficiency of lung segment analysis on CT scans.
AI in Lung Segment Analysis on CT: Beyond the Hype

The field of medical imaging is rapidly advancing, with Artificial Intelligence (AI) playing an increasingly important role. But what practical impact is AI having on lung segment analysis from CT scans? Beyond the hype, AI, particularly deep learning, is demonstrating tangible benefits. This section explores the real-world applications, advantages, and current challenges of AI-driven lung segment analysis.
Where AI Excels
AI algorithms are particularly adept at automating tasks that are traditionally time-consuming. Manual segmentation, where radiologists meticulously delineate each lung segment, is a prime example. This process, while precise, is labor-intensive. AI algorithms can automate this, dramatically reducing analysis time. This increased efficiency allows radiologists to dedicate more time to complex diagnoses and personalized patient care.
AI algorithms also offer remarkable consistency. Unlike human assessment, which can vary due to fatigue or experience, AI delivers standardized analysis. This minimizes variability between image readings. Such consistency proves especially valuable in large studies or when comparing scans over time to monitor disease progression.
The Challenges AI Faces
Despite the progress, AI still faces challenges. One key hurdle lies in the diversity of lung pathologies. Conditions like ARDS or COVID-19, characterized by consolidated lung regions with complex boundaries, can prove challenging even for sophisticated AI algorithms to segment accurately. The indistinct lines between healthy and diseased tissue make precise demarcation difficult.
The performance of AI algorithms is directly tied to the data they are trained on. The quality and representativeness of this training data are crucial. If the data lacks diversity in terms of patient demographics or scanner types, the algorithm's performance in real-world clinical settings may be limited.
Performance Metrics and Practical Considerations
Lung segmentation on CT images relies on machine learning and deep learning techniques. The Jaccard Index (JI), a common metric for assessing segmentation quality, quantifies the overlap between the algorithm's output and manual segmentation. While models like U-Net can achieve high JI values, performance varies based on the specific pathology. Learn more about this research. For example, algorithms tend to perform better with COPD due to the increased contrast from emphysema, but struggle with conditions like ARDS or COVID-19.
Integrating AI into Clinical Workflows
Leading institutions are cautiously incorporating AI tools into their clinical practices. The focus is on using AI as a supportive tool, not a replacement for trained radiologists. AI can pre-segment images, highlighting potential areas of concern for the radiologist to review. This combined approach leverages both the efficiency of AI and the diagnostic expertise of medical professionals.
Careful interpretation of AI confidence scores is also essential. In difficult cases, when the algorithm expresses low confidence in its segmentation, radiologists must rely on their own knowledge and experience to make the final diagnostic decision. This collaboration between AI and human intelligence optimizes the benefits of both.
The Future of AI in Lung Segment Analysis
The field of AI in lung segment analysis is constantly advancing. With more refined algorithms and more diverse training datasets, AI holds significant potential for increasing diagnostic accuracy, enabling personalized treatment plans, and ultimately, improving patient outcomes. The future lies in striking the optimal balance between the power of AI and the invaluable expertise of humans in medical image interpretation.
Overcoming Challenges in Lung Segments on CT
Pinpointing lung segments on CT scans can be tricky. Several factors can obscure the typical anatomical landmarks, making it difficult to distinguish between segments. This can lead to diagnostic challenges. This section explores these challenges and offers strategies used by experienced radiologists to navigate them.
Anatomical Variations and Their Impact
One common challenge stems from anatomical variations. Incomplete fissures, the thin walls of tissue separating lung lobes, can be partially or completely absent. This makes it difficult to define segment boundaries that rely on these fissures. Similarly, accessory fissures, extra fissures beyond the normal anatomy, can complicate segment identification by adding unexpected boundaries.
Experienced radiologists adapt to these variations by relying on secondary landmarks, such as the branching patterns of the segmental bronchi and pulmonary vessels. By tracing these structures from the hilum outward, they can often deduce segmental boundaries even when fissures are incomplete or unclear.
Pathological Processes and Distortion of Anatomy
Various pathologies can significantly distort normal lung anatomy, making segment identification difficult. For example, fibrosis, the thickening and scarring of lung tissue, can obscure normal segmental boundaries. Emphysema, marked by the destruction of alveolar walls, can also lead to substantial anatomical alterations. These changes can make it difficult to recognize traditional landmarks.
When faced with such pathologies, radiologists use a combination of techniques. They might compare the affected lung to the contralateral, healthier lung, looking for subtle differences. They also correlate CT findings with clinical history and other diagnostic tests to arrive at the most accurate segmental localization.
Troubleshooting Techniques When Landmarks Disappear
In difficult cases where standard landmarks are obscured, experienced radiologists use specific troubleshooting techniques. One technique is adjusting the window and level settings on the CT images. This optimizes the visualization of varying tissue densities, which can help delineate subtle boundaries obscured by disease.
Multiplanar reformatting, viewing CT data in different anatomical planes (axial, coronal, and sagittal), is also essential. Analyzing the lung segments from multiple perspectives provides a more comprehensive view, even when individual views are limited. To learn more about the potential of AI in similar applications, explore the benefits of AI writing tools and their use in generating reports or educational materials.
Utilizing Advanced Imaging Modalities
When conventional CT is insufficient, advanced imaging modalities can be helpful. High-resolution CT (HRCT) offers greater detail, enabling better visualization of subtle anatomical structures. Functional imaging techniques, such as perfusion CT or ventilation/perfusion scintigraphy, can also supplement anatomical data, providing further clues to segmental localization.
By mastering these techniques, radiologists can confidently interpret lung segments on CT, even in the most challenging cases. This expertise leads to improved diagnostic accuracy and, ultimately, better patient care.
The Future of Lung Segments on CT: Emerging Applications
Lung segmentation on CT scans is no longer just for traditional diagnosis. It's now a cornerstone of personalized medicine, offering exciting new possibilities for patient care. This evolution is driven by advancements in imaging technology, sophisticated analysis techniques, and the integration of diverse data sources.
Radiomics and Texture Analysis: Unlocking Hidden Patterns
Researchers are using radiomics and texture analysis to delve deeper into segmented lung regions. These techniques extract quantitative features from medical images, uncovering subtle patterns invisible to the naked eye. This means potential disease signatures could be detected even before visible changes appear on standard CT scans.
For example, subtle shifts in tissue density or texture within a specific lung segment might indicate early signs of fibrosis or inflammation before noticeable lesions develop. This allows for earlier intervention and the potential to slow disease progression.
Fusion Imaging: Creating a More Complete Picture
Combining lung segment analysis with functional imaging is transforming treatment planning. Integrating anatomical data from CT scans with functional data from modalities like Positron Emission Tomography (PET) or Single-Photon Emission Computed Tomography (SPECT) provides clinicians with a more holistic view of the disease.
This comprehensive approach enables treatments tailored to the specific metabolic activity of diseased tissue within individual lung segments. This level of precision optimizes treatment efficacy and minimizes potential side effects.
Quantitative Assessment: Transforming Patient Monitoring
Quantitative assessment of lung segments is revolutionizing patient monitoring. By precisely measuring segmental volumes, densities, and other key parameters, clinicians can track a patient's response to therapy with unprecedented accuracy.
This allows for an objective evaluation of treatment effectiveness, enabling timely adjustments to therapy as needed. It also provides more precise monitoring of disease progression, empowering proactive management strategies.
Integrating With Genetic and Molecular Data: The Path to Personalized Treatment
Leading institutions are integrating advanced segmentation techniques with genetic and molecular data. This approach fosters a deeper understanding of the underlying mechanisms driving disease within individual lung segments.
By correlating imaging findings with genetic profiles, researchers can identify specific biomarkers linked to disease subtypes and treatment response. This integration is essential for developing truly personalized treatment strategies for complex pulmonary conditions.
Visit PYCAD to learn how their AI solutions can optimize medical devices, improve diagnostic accuracy, and enhance patient care.






