The Evolution of Machine Learning for Medical Imaging
Medical imaging has undergone a dramatic transformation. Traditionally, radiologists meticulously examined images, painstakingly searching for subtle anomalies. This manual process, while often effective, was time-consuming and potentially prone to human error. This is where the power of machine learning for medical imaging comes into play.
This evolution started with simpler computer-aided detection (CAD) systems. These systems highlighted potential areas of concern directly on the images. However, these early CAD systems had their limitations. They frequently generated false positives, requiring extensive manual review by radiologists.
For example, an early CAD system might incorrectly flag a normal anatomical variation as a potential tumor. This would then lead to unnecessary further investigation. Ultimately, radiologists still needed to scrutinize each image, significantly reducing the anticipated time-saving benefits of the technology.
The Rise of Deep Learning
The advent of deep learning, a specialized subfield of machine learning, marked a pivotal advancement in medical imaging. Deep learning algorithms, especially convolutional neural networks (CNNs), are designed for analyzing image data. Convolutional Neural Network algorithms are capable of learning complex patterns and features from massive datasets, exceeding the capabilities of earlier CAD systems.
Moreover, these powerful algorithms can detect subtle anomalies often imperceptible to the human eye. This improved detection ability leads to earlier and more accurate diagnoses, potentially impacting patient outcomes significantly. The sheer volume of medical imaging data available has also fueled the rapid growth in this field.
Modern imaging techniques like CT scans, MRI, and ultrasound generate enormous datasets. This increase in data, while posing storage and management challenges, provides the raw material needed to train highly sophisticated deep learning algorithms. The financial investment in this technology speaks volumes about its potential.
The global AI in medical imaging market reached an estimated value of USD 1.63 billion in 2025. This demonstrates that machine learning in medical imaging isn't just a theoretical research interest. It's a rapidly expanding market with tangible real-world applications. You can explore more detailed statistics on the growth of this market here: AI in Medical Imaging Market.
The increasing availability of data combined with advances in computing power has paved the way for even more advanced applications of machine learning in medical imaging. These advancements promise to further refine diagnostic accuracy, personalize treatment strategies, and ultimately, enhance the quality of patient care.
Breaking Down the Algorithms That Actually Work
Not all AI approaches are equally effective in medical imaging. This section examines the specific machine learning algorithms delivering true clinical value. We'll demystify complex concepts like convolutional neural networks (CNNs) and transfer learning, explaining them in accessible terms with practical examples. This exploration reveals how these technologies address challenges such as limited training data and the need for interpretable AI-driven results.
Convolutional Neural Networks (CNNs): The Engine of Image Recognition
CNNs are particularly well-suited for image analysis. Imagine a CNN as a series of filters applied to an image. Each filter learns to detect specific features, like edges, textures, and shapes. As the image passes through these layers, the network builds a hierarchical representation, recognizing increasingly complex patterns.
For example, in a chest X-ray, early layers might identify lines and curves. Deeper layers then recognize ribcage structures and eventually potential lung nodules. This layered approach allows CNNs to effectively analyze the complex visual information present in medical images.
Transfer Learning: Leveraging Existing Knowledge
Training deep learning models requires substantial datasets. However, acquiring large, labeled medical image datasets can be difficult. Transfer learning offers a solution. This technique takes a pre-trained model, often trained on a large general image dataset like ImageNet, and fine-tunes it on a smaller, specialized medical image dataset.
This allows the model to leverage previously learned features, accelerating training and often improving performance, even with limited medical data. It's analogous to teaching a seasoned artist a new painting style, rather than starting with a novice. This approach makes deep learning more feasible in medical imaging, where large datasets can be scarce.
Addressing Unique Challenges in Medical Imaging
Machine learning for medical imaging faces unique challenges. Medical images are often complex, and subtle differences can have significant clinical implications. The need for explainable AI is also paramount. Clinicians need to understand why an algorithm makes a specific prediction to trust and integrate it into their workflow.
Researchers are actively developing techniques to increase the transparency of AI decisions. These techniques offer insights into the features driving a diagnosis. This transparency helps build trust and ensures that AI augments, rather than replaces, clinical judgment.
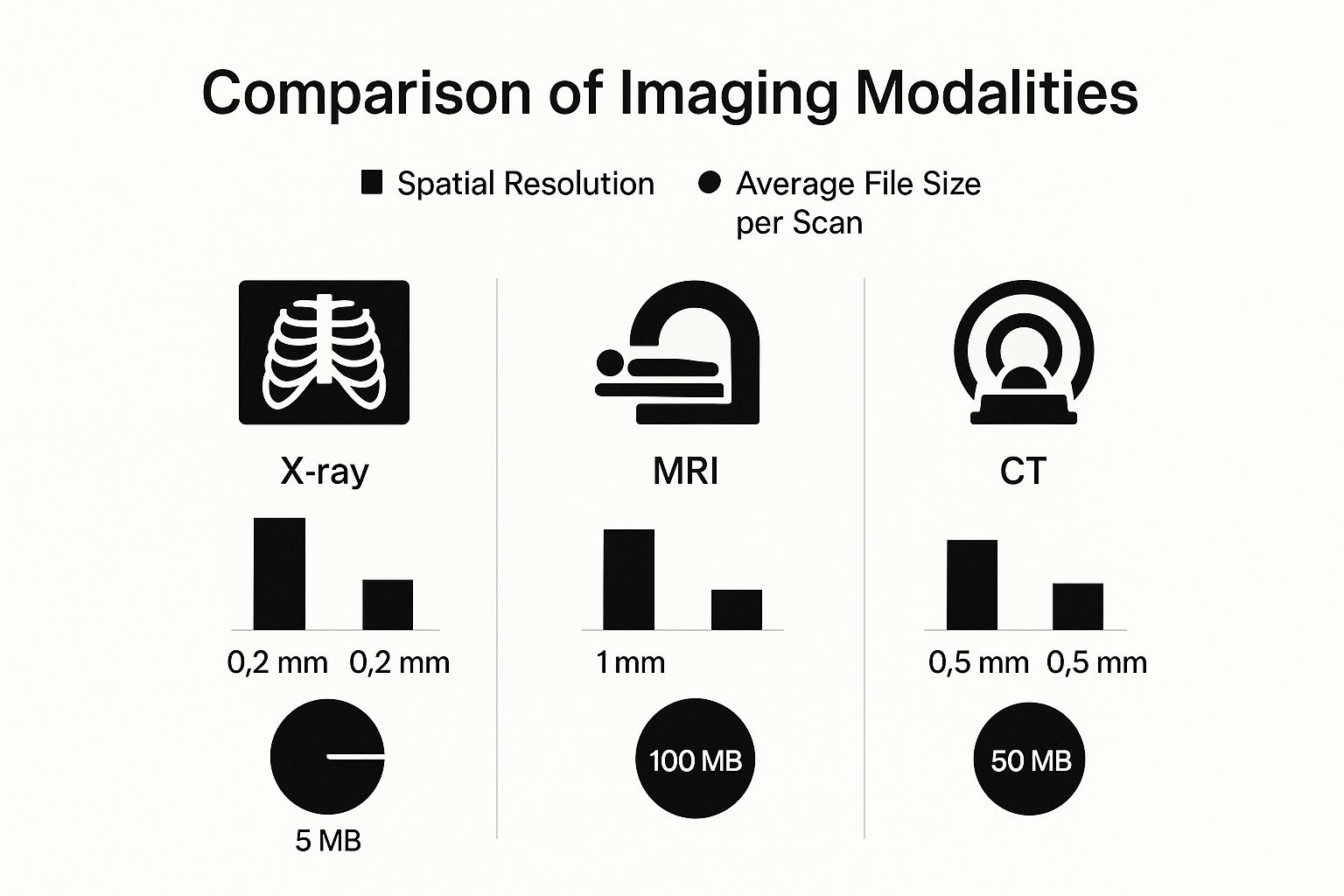
This visualization highlights the trade-off between image detail (spatial resolution) and data storage requirements. CT scans, for example, offer high-resolution images but have larger file sizes compared to X-rays. These factors influence the computational resources and algorithm selection in machine learning for medical imaging.
To further elaborate on the different machine learning approaches used in medical image analysis, let's look at a comparison table:
Comparison of Machine Learning Techniques in Medical Imaging
A side-by-side comparison of popular machine learning approaches for different medical imaging applications.
| ML Technique | Optimal Imaging Modality | Key Advantages | Limitations | Clinical Applications |
|---|---|---|---|---|
| Convolutional Neural Networks (CNNs) | CT, MRI, X-ray | Excellent for image classification and object detection | Requires large datasets for optimal performance | Tumor detection, disease classification |
| Support Vector Machines (SVMs) | Ultrasound, X-ray | Effective for image segmentation | Can be sensitive to parameter tuning | Organ boundary delineation, tissue characterization |
| Transfer Learning | Various | Enables training with limited data | Performance depends on the pre-trained model | Improving model accuracy with scarce medical data |
This table summarizes the key differences and similarities between various machine learning techniques, their suitability for different imaging modalities, and their clinical applications. The choice of technique often depends on the specific task and the available data.
Choosing the Right Algorithm for the Task
Different algorithms excel at different tasks. CNNs are often preferred for image classification and object detection, making them suitable for identifying tumors or other anomalies in medical images. Other algorithms, like support vector machines (SVMs), can be effective for tasks like image segmentation, outlining specific structures within an image.
The field of AI is constantly evolving. For more information on its progression, see this guide on the Evolution of AI. Selecting the appropriate algorithm depends on the specific application, available data, and the desired clinical outcome. This emphasizes the importance of collaboration between AI specialists and medical professionals. Ultimately, the success of machine learning in medical imaging relies on choosing the right algorithm for the specific clinical problem.
Breakthrough Applications Changing Patient Care

Machine learning is rapidly changing the face of medical imaging and patient care. This section explores some real-world applications, demonstrating the impact of this technology across various imaging modalities. We'll see how these tools are being integrated into clinical settings and their positive effects on diagnosis, treatment, and patient outcomes.
Early Detection of Neurodegenerative Diseases
One key application of machine learning lies in the early detection of neurodegenerative diseases. AI-enhanced MRI analysis can identify subtle brain structure changes, often indicative of diseases like Alzheimer's, years before traditional methods. This early detection facilitates timely interventions, potentially slowing disease progression and improving patients' quality of life. This early warning provides a critical window of opportunity for patients and families to plan for the future.
Expanding Access to Care with Automated Screening
Automated chest X-ray screening, powered by machine learning, is expanding healthcare access, particularly in underserved areas. These systems can quickly analyze X-rays, highlighting potential problems for review by a radiologist. This expedites the diagnostic process and extends the reach of qualified radiologists to regions with limited access to specialists. This broader access to screening holds great promise for significantly improving overall public health.
Achieving Superhuman Performance in Cancer Detection
Deep learning algorithms are achieving remarkable results in cancer detection from medical images. In some instances, these algorithms are outperforming human specialists, particularly in identifying small or subtle lesions that might otherwise be missed. This improved accuracy leads to earlier diagnoses and more effective treatment plans, ultimately improving patient survival rates. This translates into tangible, life-saving benefits for patients.
For example, some AI systems can detect tiny cancerous nodules in lung CT scans with remarkable precision. This level of detail is crucial for early intervention and a better prognosis. It also reduces the need for invasive biopsies, minimizing patient discomfort and potential risks.
Integrating AI into Clinical Workflows
Further advancements in imaging technology, such as photon-counting CT, digital SPECT, and whole-body MRI, are also driving progress in the field. Combining AI with these cutting-edge technologies will likely have a dramatic effect on diagnostic capabilities. To learn more about these exciting developments, see Medical Imaging Trends to Watch. The increasing use of AI in interpreting X-ray, CT, and MRI images highlights the growing importance of AI-integrated devices for faster, more precise diagnoses.
These applications demonstrate how machine learning in medical imaging is becoming increasingly integrated into standard clinical practice. By automating tasks, enhancing accuracy, and broadening access to care, these AI-powered tools are not simply assisting clinicians–they are empowering them to provide superior patient care. The continued development and refinement of these technologies hold immense potential for the future of medical imaging.
Overcoming Real-World Implementation Hurdles
While machine learning holds immense potential for medical imaging, its widespread adoption faces real-world challenges. These range from integrating the technology into existing systems to addressing concerns about data privacy and acceptance among medical professionals. This section explores these barriers and offers practical solutions for successful implementation.
Data Privacy and Security: Protecting Patient Information
Medical images contain highly sensitive personal information. This necessitates strict adherence to regulations like HIPAA. Any machine learning system must prioritize robust security measures. These measures should include secure data storage, anonymization techniques, and strict access controls to protect patient data from unauthorized access or breaches. Failure to comply can result in significant penalties and damage patient trust.
Legacy System Integration: Bridging the Technological Gap
Many healthcare institutions still rely on older IT infrastructure, or legacy systems. Integrating new machine learning tools with these systems can be a complex and costly process, often requiring custom interfaces and significant IT resources. Interoperability between different systems within a hospital or clinic also presents a challenge. Successful integration demands careful planning, collaboration between IT staff and clinicians, and a phased implementation approach. This minimizes disruption and ensures a smoother transition.
Professional Resistance: Addressing Clinician Concerns
The introduction of machine learning in medical imaging may be met with resistance from healthcare professionals. Some clinicians might be hesitant to embrace new technologies, fearing job displacement. Others might be skeptical of the accuracy and reliability of these systems. Addressing these concerns requires open communication and comprehensive training programs. These programs should emphasize how machine learning can augment, not replace, clinical expertise. Showcasing real-world examples of how AI improves diagnostic accuracy and efficiency can build trust and encourage wider adoption.
To help illustrate some of these challenges and their potential solutions, the table below provides a more detailed breakdown:
Introduction to Table: The following table outlines common barriers encountered during the implementation of machine learning in medical imaging, along with recommended solutions and key indicators of success.
| Challenge Category | Specific Issues | Recommended Solutions | Success Indicators |
|---|---|---|---|
| Data Privacy and Security | HIPAA compliance, data breaches, anonymization challenges | Secure data storage solutions, robust anonymization techniques, strict access controls, regular audits | Low incidence of data breaches, successful de-identification of patient data, demonstrable compliance with HIPAA regulations |
| Legacy System Integration | Compatibility issues with existing infrastructure, complex integration processes, high implementation costs | Phased implementation approach, custom interface development, collaboration between IT and clinical staff | Seamless data exchange between systems, minimal disruption to existing workflows, reduction in IT support tickets related to integration |
| Professional Resistance | Clinician skepticism, fear of job displacement, lack of training | Comprehensive training programs, clear communication about AI's role, showcasing successful use cases, emphasizing AI as an augmentation tool | Increased clinician comfort with AI tools, improved diagnostic accuracy and efficiency, active participation in AI-related initiatives |
Conclusion of Table: By proactively addressing these challenges with the suggested solutions, healthcare institutions can foster a more conducive environment for the successful implementation of machine learning technologies. Monitoring the success indicators will allow for continuous improvement and adaptation to the evolving needs of the clinical setting.
Strategies for Successful Implementation
Successfully navigating these challenges requires a strategic approach that considers both technical and human factors.
-
Staff Training: Comprehensive training programs are crucial for familiarizing clinicians with the new tools and their capabilities. This builds confidence and promotes effective use.
-
Phased Rollout: A gradual introduction of the technology, starting with pilot programs in specific departments, allows for iterative feedback and refinement before wider deployment.
-
Clear Governance Frameworks: Establishing clear guidelines for data governance, algorithm validation, and ethical considerations builds trust and ensures responsible use of AI.
-
Continuous Monitoring and Evaluation: Regularly assessing system performance and gathering clinician feedback allows for ongoing optimization and adaptation to evolving clinical needs.
Building a sustainable AI program in medical imaging requires meticulous planning, open communication, and a commitment to addressing real-world challenges. By proactively addressing these hurdles, healthcare institutions can unlock the full potential of machine learning to improve patient care and drive operational efficiencies.
Building Trust Through Rigorous Validation
In medical imaging, errors can have significant consequences for patients. Ensuring the safety and accuracy of AI systems is paramount for building trust within the clinical setting. This section explores the essential frameworks and rigorous validation protocols necessary to confirm these systems are ready for real-world clinical use.
Beyond Simple Accuracy: Comprehensive Validation Protocols
Validating machine learning models for medical imaging goes far beyond simply calculating overall accuracy. Leading institutions are developing comprehensive protocols that assess performance across diverse patient populations and realistic clinical scenarios. This involves evaluating a model's sensitivity and specificity – its ability to correctly identify both positive and negative cases.
For example, a model might achieve high overall accuracy yet struggle to detect rare or subtle abnormalities. A comprehensive validation process considers these nuances and evaluates performance across a representative range of cases. This rigorous approach helps fully understand the model's strengths and weaknesses before clinical deployment.
Addressing Algorithmic Bias: Fairness and Equity in AI
Machine learning models can inherit biases present in the training data. This can lead to performance disparities across different demographic groups. For instance, a model trained primarily on images from one ethnic group might be less accurate on images from others.
Emerging techniques are being developed to identify and mitigate these biases, promoting fairness and equity in AI-driven healthcare. This includes careful curation of training data to ensure diverse representation and the development of algorithms less susceptible to bias. These ongoing efforts are vital to ensuring AI benefits all patients equally.
Opening the Black Box: Transparency and Explainability
Many deep learning models are considered "black boxes" because their internal decision-making processes are opaque. This lack of transparency can make it difficult for clinicians to understand why a model makes a specific prediction, hindering trust and adoption. New methods are being explored to make these algorithms more transparent.
Techniques like attention maps can highlight the image regions the model focused on when making its decision. This provides valuable insights into the model's reasoning, allowing clinicians to better interpret its predictions. Increased transparency is crucial for building clinician confidence and facilitating seamless integration into clinical workflows.
Continuous Monitoring: Adapting to Evolving Landscapes
Medical imaging technology and patient demographics are constantly evolving. This means even rigorously validated models require continuous monitoring to ensure optimal performance over time. Monitoring involves tracking key metrics like accuracy and sensitivity on new data and retraining the model as needed.
Additionally, as new imaging techniques emerge and patient populations shift, models must be updated and revalidated to reflect these changes. This ongoing process of adaptation and refinement is crucial for ensuring AI systems remain reliable and effective tools for enhancing patient care. By adhering to these rigorous validation practices, developers can build trust in machine learning for medical imaging and pave the way for its widespread adoption in clinical settings.
The Next Frontier of Medical Imaging Intelligence
Looking ahead at the future of medical imaging intelligence, it's essential to understand the broader impact of Artificial Intelligence (AI). This section explores exciting developments that are set to transform radiology and the wider medical field.
Federated Learning: Collaborative Intelligence, Preserved Privacy
Federated learning is a groundbreaking approach to collaborative AI model training. It allows multiple institutions to work together on improving algorithms without compromising patient privacy. Think of it like this: each hospital trains a small part of the same model using their own data. They then share only the learned parameters, not the sensitive patient data itself. These parameters are combined to create a more robust and accurate overall model. This protects patient data while improving the accuracy of diagnostic algorithms.
Multimodal Imaging: Integrating Data for a Fuller Picture
Multimodal imaging systems represent a significant step forward in diagnostic capabilities. These systems integrate data from different sources like medical images, genomic information, and patient records to provide a comprehensive view of a patient's health. This integrated approach helps identify complex relationships between different data types, leading to earlier and more precise diagnoses, especially in fields like oncology and neurology. It's like having a team of specialists contributing to a single, more informed diagnosis.
Predictive Algorithms: Forecasting Disease Progression
Predictive algorithms analyze sequential scans over time to anticipate the course of a disease. In oncology, for example, these algorithms can forecast tumor growth and treatment response. This allows clinicians to personalize treatment plans and make proactive decisions about patient management, potentially leading to better outcomes. This shift from reactive to proactive care can drastically improve the effectiveness of treatments.
Transforming the Radiologist's Role
These technologies are not designed to replace radiologists. Instead, they empower them by automating routine tasks. This frees up radiologists to concentrate on more complex cases, engage in research, and spend more time interacting directly with patients. This redefined role emphasizes the interpretation of AI-generated findings, patient communication, and collaboration with other specialists, leading to more efficient and personalized care.
These advances in machine learning for medical imaging promise to improve patient care, increase diagnostic accuracy, and potentially lower healthcare costs. By automating time-consuming tasks and providing earlier and more accurate diagnoses, these technologies will significantly reshape the future of medicine.
Are you interested in using the power of AI in your medical imaging applications? Learn more about how PYCAD can help you integrate these advanced solutions.






