Understanding Machine Learning in Medical Imaging: Beyond the Hype

Think of machine learning in medical imaging like having a tireless, always-on medical resident. This resident can analyze thousands of scans while you grab a coffee, learning intricate patterns and sometimes spotting subtleties even seasoned radiologists might miss. It’s this ability to detect faint whispers of disease in X-rays, MRIs, and CT scans, often at the earliest stages, that makes machine learning so compelling in this field.
This isn't just automation; it's about cultivating a powerful diagnostic partner. Imagine an algorithm trained on countless mammograms. Over time, it learns to identify tiny variations in tissue density, possibly signaling a small tumor even before it's clearly visible to us. This early detection can be life-changing, improving treatment success and patient outcomes.
The field is buzzing with activity and investment. The global AI in medical imaging market is booming. By 2025, it's predicted to be worth around USD 1.63 billion, and projected to reach USD 13.04 billion by 2032, growing at a compound annual growth rate (CAGR) of 34.6% between 2025 and 2032. This rapid growth speaks volumes about the recognized potential of machine learning to reshape healthcare. You can learn more about this growing market here.
Supervised Vs. Unsupervised Learning: Two Sides of the Same Coin
Grasping the core principles of machine learning is essential to understanding its influence on medical imaging. Two main approaches are supervised learning and unsupervised learning.
In supervised learning, we guide the algorithm with labeled examples, much like teaching. We show it images, say, of cancerous tumors and healthy tissue, clearly marking each. The algorithm learns the differences based on these labeled examples.
Unsupervised learning, on the other hand, lets the algorithm take the reins. Imagine giving our resident a stack of unlabeled scans and asking them to find any recurring patterns. The algorithm sifts through the data, grouping similar images and revealing hidden relationships we might not readily see.
This approach can be especially valuable for spotting new or unexpected patterns in medical data. The combination of AI with interactive video further expands the possibilities for training and education in medical imaging. You can explore this more at AI Interactive Video. Both supervised and unsupervised learning bring distinct advantages, and are often used together to get the best results in medical imaging.
Key Machine Learning Techniques That Are Changing Everything
Imagine teaching a child to recognize different types of dogs. You might start with basic shapes ("Look, this one has pointy ears!"), then move to specific features ("This one has spots, that one has stripes"), and eventually, they learn how those features combine into recognizable patterns ("That's a Dalmatian, that's a Beagle"). This process mirrors how Convolutional Neural Networks (CNNs) work in medical imaging. Instead of dog breeds, CNNs learn to identify tumors, fractures, and other anomalies within medical scans, often with impressive accuracy. These networks are like digital detectives, sifting through layers of data to uncover hidden clues.
Convolutional Neural Networks: The Image Recognition Experts
CNNs are particularly adept at analyzing images. Think about how your own eyes work: you perceive edges, shapes, and textures, and your brain assembles this information to recognize objects. CNNs emulate this process. They use filters – kind of like specialized lenses – to detect particular features in images, such as variations in tissue density or the unique outline of a blood vessel. As these filtered images pass through the network's multiple layers, the CNN learns to identify complex patterns that signify different medical conditions.
Beyond CNNs: Other Powerful Algorithms
While CNNs are undoubtedly stars in the medical imaging field, other machine learning techniques play vital roles. Support Vector Machines (SVMs) are like expert categorizers, drawing precise boundaries between different types of images, such as distinguishing between benign and malignant tumors. Random Forests, on the other hand, work like a team of specialists, each analyzing the image from a different angle and then pooling their insights for a more robust and accurate diagnosis.
Let's look at the following infographic to visualize how these algorithms fit into the broader machine learning landscape for medical imaging.
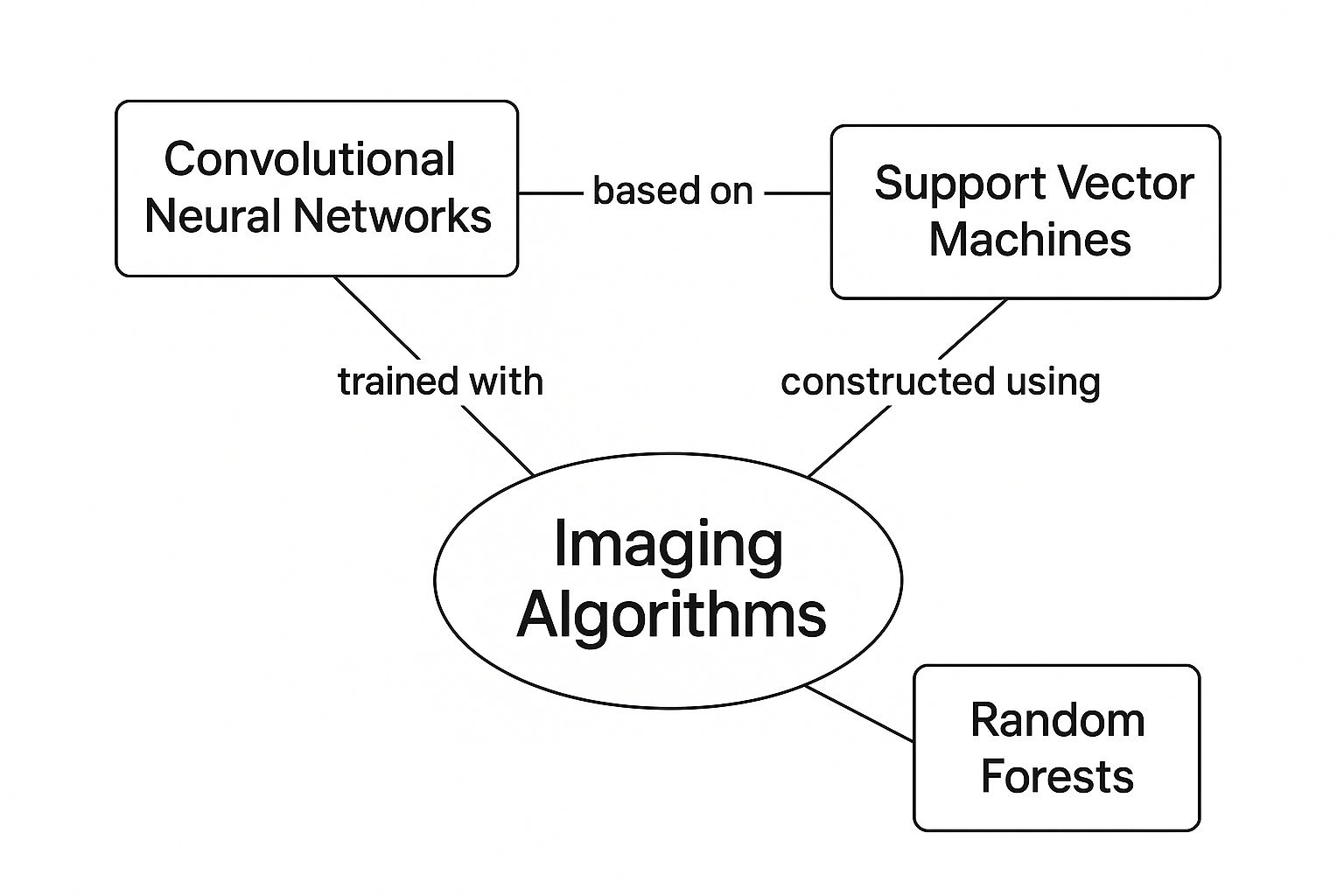
As the infographic shows, imaging algorithms are central to this process. The three techniques we've discussed – CNNs, SVMs, and Random Forests – are highlighted, showcasing their importance in medical image analysis. It’s worth noting that these algorithms aren’t mutually exclusive; they often work together in practical applications, complementing each other’s strengths.
Transfer Learning: Leveraging Existing Knowledge
Imagine you’ve taught your dog to fetch a tennis ball. You then introduce a baseball, and, to your delight, your dog quickly understands the new game. This adaptability is similar to transfer learning in machine learning. Models trained on vast datasets of general images (like those used for image recognition in everyday photos) can be fine-tuned for specific medical applications. This approach saves valuable time and resources by leveraging pre-existing knowledge. For instance, a model already proficient at identifying objects in photos could be adapted to recognize anatomical structures or pinpoint anomalies in medical scans.
Ensemble Methods: The Power of Collaboration
Think about a complex medical case where multiple specialists come together for a consultation. This collaborative approach often leads to a more accurate diagnosis than any single doctor could provide. Similarly, ensemble methods in machine learning combine the predictions of several AI models. This collaboration improves diagnostic accuracy by mitigating the biases of individual models and leveraging the unique strengths of different algorithms. By comparing and contrasting their findings, these combined models offer a more complete and trustworthy assessment, ultimately enhancing patient care. Through these innovative techniques, machine learning continues to revolutionize medical imaging, offering the potential for earlier and more accurate disease detection.
To provide a clearer picture of how these techniques are applied, let's take a look at a comparison table:
Machine Learning Techniques: Real-World Medical Applications
A practical comparison of different ML approaches, their diagnostic accuracy, and specific clinical applications that matter to healthcare providers.
| Technique | Primary Medical Use | Diagnostic Accuracy | Implementation Requirements | Clinical Success Stories |
|---|---|---|---|---|
| Convolutional Neural Networks (CNNs) | Image recognition and classification (e.g., detecting tumors, classifying skin lesions) | High, often exceeding human performance in specific tasks | Large datasets for training, significant computational resources | Successful detection of diabetic retinopathy, lung cancer screening |
| Support Vector Machines (SVMs) | Classification of medical images (e.g., differentiating benign from malignant tumors) | Generally high, depends on data quality and feature selection | Careful feature engineering and selection, appropriate kernel selection | Effective in breast cancer diagnosis, distinguishing between different types of heart conditions |
| Random Forests | Classification and prediction based on medical data (e.g., predicting patient outcomes, identifying risk factors) | High, robust to noisy data and outliers | Large datasets are beneficial, parameter tuning important | Used for predicting patient survival rates, identifying individuals at risk for certain diseases |
| Transfer Learning | Adapting pre-trained models to specific medical tasks (e.g., fine-tuning an image recognition model for detecting specific anatomical features) | High, depends on the quality of the pre-trained model and the target dataset | Access to pre-trained models, some fine-tuning required | Used for adapting general image recognition models for detecting specific conditions in medical images |
| Ensemble Methods | Combining predictions from multiple models to improve diagnostic accuracy (e.g., integrating results from CNNs, SVMs, and other algorithms) | Potentially higher than individual models, improves robustness and reduces bias | Requires training and managing multiple models, increased computational complexity | Used for improving the accuracy of cancer diagnosis, enhancing the reliability of medical image analysis |
This table summarizes key applications and considerations for each technique. It highlights the potential for high diagnostic accuracy across various methods and underscores the importance of data quality and computational resources. Choosing the right technique often depends on the specific medical task and the available resources.
Where AI Meets Patient Care: Real Stories From the Front Lines

Step into any modern hospital today, and you’ll see how machine learning is quietly reshaping medical imaging and patient care. In bustling emergency rooms, AI helps doctors rapidly identify strokes, saving precious minutes when every second counts. Oncology departments are using it to spot cancers earlier than ever before, leading to better patient outcomes. These technologies aren’t replacing doctors; they’re empowering them. Think of it as giving doctors a superpower.
AI-Powered Diagnosis: A Second Pair of Eyes
Radiologists, often burdened with heavy workloads, are finding AI to be an invaluable partner. Imagine scrutinizing hundreds of medical images every single day—a task that demands intense focus. AI can pre-screen these images, highlighting potential problems and prioritizing urgent cases.
This not only helps manage the sheer volume of scans but also improves diagnostic accuracy by reducing the chance of human error caused by fatigue. This frees up radiologists to focus their expertise where it’s needed most: on the complex cases that require their in-depth knowledge and experience, ultimately ensuring patients receive the best possible care.
Additionally, AI is showing a remarkable ability to predict disease progression. Take a patient with multiple sclerosis (MS), for example. Analyzing MRI scans over time can reveal subtle shifts that signal disease activity. Machine learning models have shown remarkable accuracy in predicting the progression of MS – up to 86% – by analyzing these temporal patterns. This predictive power has huge implications for patient care, opening doors for earlier interventions and highlighting AI’s potential for medical research and personalized medicine. Want to explore this further? Explore this insightful article on the future of medical imaging.
Transforming Treatment: From Routine Screenings to Surgical Planning
The use of machine learning in medical imaging extends far beyond simply making a diagnosis. AI is also assisting with surgical planning, creating 3D models from medical scans that allow surgeons to visualize complex procedures before they even make an incision. This allows for more precise, less invasive surgeries, shorter recovery times, and fewer complications.
AI is also making a significant impact on routine screenings. Consider mammograms: AI can analyze these images, picking up on subtle patterns that could indicate early signs of breast cancer, often before they are even visible to the human eye. This early detection can be truly life-saving, offering patients a much greater chance of successful treatment.
Real-World Impact: Stories of Success
The benefits of machine learning aren't just theoretical; they're being seen in hospitals around the world. One powerful example is the use of AI to detect diabetic retinopathy, a leading cause of blindness. AI systems can analyze retinal images, identifying early warning signs of the disease with remarkable accuracy. This allows for prompt treatment, preventing vision loss and preserving patients' quality of life. Interested in learning more about AI’s broad range of applications? Check out this Ultimate Guide To AI.
Another compelling example comes from cardiology. AI is being used to analyze heart scans, identifying subtle shifts in heart function that could indicate an impending heart attack. This early warning system empowers doctors to take proactive steps, potentially saving lives. These are just a few of the many ways machine learning in medical imaging is transforming healthcare, making it more efficient, more accurate, and more patient-centered. These advancements are happening now, improving outcomes for patients worldwide.
Solving Healthcare's Crisis: Why This Matters More Than Ever

Healthcare systems around the world are facing some serious challenges. Think about it: growing patient numbers combined with a shortage of doctors creates a perfect storm. Resources are stretched thin, and the pressure is on for faster, more accurate diagnoses. This is where machine learning in medical imaging comes in, not just as a cool new technology, but as a vital tool.
Imagine the average radiologist, swamped with countless imaging studies every day. Some departments are seeing a 30% increase in scan volumes year over year, but the number of radiologists isn't keeping up. This leads to an overwhelming workload, increasing the chance of burnout and potentially impacting how accurately they can diagnose patients. Machine learning systems are helping to ease this burden.
These systems aren't meant to replace human experts. They're more like intelligent assistants, pre-screening images, highlighting potential problems, and making sure urgent cases get seen first. This lets radiologists concentrate their expertise on the more complex diagnoses and tricky cases, boosting efficiency and making it less likely that something important gets missed. For a real-world example, consider how AI Customer Support in Dental Practices is changing things.
Economic Impact: Beyond the Immediate Benefits
Machine learning in medical imaging has a real economic impact, too. Fewer diagnostic errors mean fewer unnecessary procedures and treatments, saving money for both patients and healthcare providers. Quicker results mean happier patients and faster intervention, potentially stopping diseases from getting worse.
Machine learning also helps healthcare providers use their resources more effectively. By automating routine tasks, it frees up valuable staff time so healthcare professionals can concentrate on patient care and those more complex cases. This optimized workflow boosts overall system efficiency and reduces healthcare costs. In 2025, we're seeing a growing trend towards using AI solutions that can automate tasks, improve image analysis, and support patient-focused care. The adoption of machine learning in medical imaging is being driven by the need to address workforce shortages and improve efficiency in radiology departments. Discover more insights about the AI in medical imaging market here.
Bridging the Gap: Access to Specialized Care
Machine learning is also key to bringing advanced diagnostics to underserved communities, especially in rural areas where access to specialists might be limited. Picture a small clinic in a remote area with an AI-powered imaging system. This system could analyze scans and offer preliminary diagnoses, even without a specialist on-site.
This quick access to diagnostic information can be life-changing for patients, particularly when dealing with time-sensitive conditions. It also means patients don’t have to travel long distances to see a specialist, making healthcare more accessible for everyone. This ability to bridge the geographical gap is a big step toward making healthcare more equitable, ensuring that everyone, no matter where they live, has access to quality diagnostic services. This increased access, fueled by machine learning, highlights its potential to solve some of the biggest challenges facing healthcare today. Machine learning in medical imaging doesn't just address the immediate needs of our stressed healthcare systems; it helps build a more sustainable and equitable future for how we deliver healthcare.
Navigating Real-World Implementation Challenges
Bringing the power of machine learning to medical imaging sounds straightforward, but it's anything but. It's not just about installing new software. Healthcare organizations face real-world hurdles that can make or break these projects. Let's explore some of the key challenges together.
Data Privacy and Security: Walking a Tightrope
Data privacy is paramount, especially when dealing with the sensitive information contained in medical images. Think about it – these images reveal deeply personal details about a patient's health. Protecting this information is not just a best practice, it's a legal and ethical imperative. Regulations like HIPAA in the US and GDPR in Europe add layers of complexity, and these rules can even differ between hospitals and countries. Getting proper informed consent from patients to use their data for machine learning models is essential, and robust security measures are crucial to prevent breaches and maintain compliance.
Integration Headaches: Bridging the Gap
Integrating these cutting-edge machine learning systems with existing hospital infrastructure can feel like fitting a square peg in a round hole. Many hospitals rely on older systems that weren't built for the data demands of AI. This incompatibility can cause major technical headaches and frustrating project delays. Imagine trying to connect a sleek, modern AI platform to a legacy PACS system—a common scenario that requires careful planning and often involves custom integration work.
Staff Training and Workflow Changes: The Human Element
Implementing new technology isn't just about teaching staff how to click buttons. It requires changing established workflows, and that can be tough for medical professionals accustomed to traditional methods. Imagine asking a radiologist who's spent years interpreting scans to suddenly rely on an AI assistant. This shift requires more than just software training; it also means addressing potential anxieties about evolving roles and responsibilities.
Addressing Concerns: Liability, Accuracy, and the Role of Humans
The introduction of AI in healthcare raises important questions about liability if a misdiagnosis occurs. Who's responsible if an AI-powered system makes an error? Maintaining human oversight is key. While AI can be an incredibly powerful tool, experienced medical professionals must remain in the loop, ensuring that critical decisions aren't solely based on algorithms.
Technical Hurdles: Image Variability and Algorithm Fairness
Medical images come from different manufacturers and can vary in quality, posing a significant technical challenge. An AI model trained on images from one type of scanner might not perform as well on images from another. Ensuring that AI systems work fairly for all patients is equally critical. Algorithms trained mainly on data from one demographic group could be less accurate for others.
Let's take a closer look at some of the specific implementation challenges healthcare leaders face with the following table. It outlines not only the business impact of these challenges but also proven solutions and how to measure success.
Implementation Challenges: What Healthcare Leaders Actually Face
A comprehensive overview of real obstacles healthcare organizations encounter when implementing ML systems and proven solutions that work.
| Challenge Category | Business Impact | Proven Solutions | Implementation Timeline | Success Indicators |
|---|---|---|---|---|
| Data Privacy and Security | Potential fines for non-compliance, reputational damage, erosion of patient trust | Data encryption, robust access controls, de-identification techniques, strict adherence to HIPAA and GDPR | Ongoing | Low incidence of data breaches, high rates of patient consent, successful audits |
| Integration with Existing Systems | Project delays, increased costs, interoperability issues | API development, custom integration solutions, cloud-based platforms | 6-12 months | Seamless data exchange between systems, minimal disruption to existing workflows |
| Staff Training and Workflow Changes | Resistance to adoption, decreased productivity, potential errors | Comprehensive training programs, change management strategies, ongoing support | 3-6 months | Increased staff proficiency with new systems, improved efficiency in diagnostic processes |
| Liability and Accuracy Concerns | Legal challenges, patient safety risks, reluctance to adopt AI tools | Human oversight of AI-generated results, rigorous validation of algorithms, transparent decision-making processes | Ongoing | Low rate of AI-related errors, high levels of physician confidence in AI tools |
| Image Variability and Algorithm Fairness | Inconsistent performance across different datasets, potential bias in diagnoses | Diverse training datasets, rigorous testing and validation across different demographics, ongoing monitoring for bias | Ongoing | Consistent performance across different imaging modalities and patient populations |
As you can see, addressing these challenges requires a multi-pronged approach. Stronger security measures are crucial, as are training programs for staff. Perhaps most importantly, continuous monitoring of AI performance and fairness helps ensure these systems are truly beneficial for all patients.
Overcoming these challenges requires careful planning, collaboration between IT specialists and medical professionals, and a commitment to addressing both technical and human factors.
Building a Successful AI Program: Lessons From the Trenches
Rolling out machine learning in medical imaging isn't simply a matter of purchasing software. It requires a fundamental shift in how your organization approaches diagnosis and patient care. This section offers practical insights gleaned from healthcare systems that have successfully navigated this transition.
Starting Small, Thinking Big: The Power of Pilot Programs
Imagine trying to overhaul an entire airplane mid-flight. Daunting, right? Launching a full-scale AI program can feel similarly overwhelming. Pilot programs offer a safer, more controlled environment, like a flight simulator for your AI initiative. These smaller projects allow you to test different AI solutions, identify integration challenges, and refine workflows without disrupting daily operations. Think of it as a test drive before committing to the whole car.
Pilots also offer a vital opportunity to build confidence within your organization. By demonstrating early successes and addressing any unexpected bumps in the road during a pilot phase, you pave the way for smoother, wider adoption down the line.
The Importance of Clinical Champions: Bridging the Gap
Now, imagine having enthusiastic physicians within your organization who are excited about the potential of AI. These clinical champions become internal ambassadors, bridging the gap between the technology and its practical application in patient care. They can help their colleagues understand the benefits of machine learning, address any concerns, and ease the transition to new workflows. They're like translators, helping everyone speak the same language.
Evaluating AI Vendors: Looking Beyond the Demo
Choosing the right AI vendor is a critical decision. Don't be swayed by a dazzling sales pitch. Look beyond the initial demo, much like kicking the tires and checking under the hood before buying a car. Focus on key factors like regulatory compliance, integration capabilities, and long-term support. Can the vendor's solution integrate smoothly with your existing PACS and EHR systems? Do they offer robust training and ongoing assistance? These questions are crucial for long-term success.
This screenshot from the FDA website underscores the importance of regulatory factors for AI-powered medical devices:
The FDA emphasizes the unique characteristics of AI/ML-based medical devices, especially their adaptability and the need for continuous monitoring and validation. Your vendor should demonstrate a deep understanding of these evolving standards.
Quality Assurance, Measurement, and Scaling: Keys to Long-Term Success
Once your pilots prove their worth, the next step is establishing solid quality assurance. How will you monitor the AI's performance and ensure its accuracy and fairness, much like regular check-ups ensure a car stays in top shape? How will you measure its impact on diagnostic accuracy, patient outcomes, and operational efficiency? These are your benchmarks for success.
Developing clear metrics and tracking systems is like keeping a detailed logbook of your AI's performance. This data helps demonstrate the value of your program and pinpoint areas for improvement. Finally, with positive pilot results and robust quality assurance in place, you can begin scaling your program across the health system. Think of it as expanding your fleet of well-maintained, high-performing vehicles. This requires careful planning, open communication with staff, and a commitment to continuous refinement.
Building a successful AI program is a journey, not a destination. It demands a strategic approach, strong leadership, and a thorough understanding of the challenges and opportunities that machine learning presents for medical imaging. By following these principles, healthcare organizations can build AI programs that deliver real value to both providers and the patients they serve.
The Next Frontier: Where Medical AI Is Heading
The future of machine learning in medical imaging is bigger than just looking at individual scans. We're moving towards a world of comprehensive patient intelligence. This means integrating imaging data with a patient's medical history, genetic predispositions, and even lifestyle factors to create a complete picture of their health. Imagine AI that not only spots diseases but predicts them before any symptoms even show up. Think of algorithms suggesting personalized treatment plans based on how similar patients responded to different therapies.
Federated Learning: Global Insights, Local Privacy
One exciting development is federated learning. This approach allows AI systems to learn from huge global datasets without sharing sensitive patient data. Think of it like an international team of researchers working together on a project. Each team contributes their findings without ever revealing their raw data. Similarly, federated learning allows AI models to train on data from many hospitals without directly exchanging patient information. This keeps data safe and private while still allowing the AI to learn from a much larger and more diverse dataset.
Quantum Leap: Revolutionizing Image Processing
Quantum computing has the potential to completely change medical imaging. Imagine being able to analyze images at the molecular level – a level of detail we can only dream of today. Quantum computers, with their enormous processing power, might make this possible, letting us see diseases at their earliest stages and understand how they work with incredible clarity. Though still in its early stages, the combination of quantum computing and medical imaging promises to unlock entirely new diagnostic and treatment options.
Partnerships That Push Boundaries: Collaboration and Innovation
The advancement of AI in medical imaging depends heavily on collaborations between tech companies and medical institutions. These partnerships bring together the tech skills of companies like Google and NVIDIA with the clinical experience of top hospitals and research centers. This speeds up the development and testing of new AI tools, making sure they meet the high standards of the medical field and ultimately benefit patients. These collaborations are pushing the limits of what's possible, combining different skills and resources to solve some of the biggest challenges in healthcare.
From Diagnosis to Prevention: A New Era of Healthcare
The ultimate aim of machine learning in medical imaging isn't just better diagnosis; it's about prevention. Imagine an AI system that understands your individual health profile so well that it can identify potential risks years in advance. This could allow for early interventions, lifestyle changes, and personalized preventative measures, drastically lowering the number of serious diseases. This shift from reacting to illness to preventing it has the potential to remake healthcare, making it more personalized, precise, and more effective. This future isn't just about finding illness – it's about actively promoting wellness and giving people control over their own health.
PYCAD: Your Partner in AI-Driven Medical Imaging
PYCAD is a company specializing in integrating artificial intelligence into medical imaging. With a history of successful projects since 2023, PYCAD provides comprehensive AI services, including data handling, model training, and deployment. Their solutions help medical device manufacturers and healthcare providers improve diagnostic accuracy, work more efficiently, and improve patient outcomes. From anonymizing and annotating data to deploying trained models as APIs or creating user-friendly interfaces, PYCAD works with clients to meet their specific needs. Learn how PYCAD can help you use the power of AI in medical imaging by visiting their website.