The Revolution Happening in Medical Imaging
Medical imaging is undergoing a significant transformation with the integration of machine learning (ML). Traditional methods like MRI, CT scans, and ultrasound are being augmented by AI algorithms, leading to remarkable progress in diagnostics. This translates to a rapidly growing potential for earlier and more precise diagnoses, directly impacting patient care as these advancements move from research into clinical practice.
AI's Impact on Diagnostic Accuracy and Efficiency
A key benefit of ML in medical imaging is improved diagnostic accuracy. AI algorithms can identify subtle patterns and anomalies often missed by the human eye, even by highly trained radiologists. This leads to earlier disease detection, especially in fields like oncology and neurology.
Furthermore, ML can automate time-consuming processes such as image analysis and measurement. This frees up radiologists to focus on complex cases and direct patient interaction, boosting efficiency and leading to quicker diagnoses and treatment planning.
For example, AI-powered tools can analyze images to pinpoint potential cancerous lesions or markers for neurodegenerative diseases with exceptional precision. Early intervention is often critical for successful treatment, so this has a substantial impact on patient outcomes. The enhanced efficiency also streamlines workflows, reducing the burden on healthcare systems.
Market Growth and Adoption of AI in Medical Imaging
The growing use of ML in medical imaging isn't just a technological advancement; it's a major market driver. The global AI in medical imaging market is predicted to expand at a 27.10% CAGR from 2025 to 2034. Valued at over $49.61 billion in 2024 for general medical imaging, the market shows significant growth in the AI sector, propelled by applications like image quality enhancement and predictive analytics.
North America currently dominates with a 38.74% market share, while the Asia-Pacific region shows the fastest growth at 28.1% CAGR. This growth is spurred by healthcare digitization and collaborations within the industry. For a deeper dive into these statistics, see: AI in Medical Imaging Market Size
Variations in Adoption and the Drivers of Innovation
While the advantages are clear, the adoption of ML in medical imaging varies across healthcare systems and regions. Factors such as access to technology, regulations, and investment in healthcare IT infrastructure contribute to these differences.
Despite this, many organizations are actively pushing innovation in this field. Early adopters are seeing significant improvements in diagnostic accuracy, operational efficiency, and overall patient care. These pioneers are paving the way for broader adoption and providing valuable insights into best practices for implementation, data management, and ethical considerations surrounding AI in healthcare. Their experiences will be invaluable in shaping the future of intelligent medical imaging.
Spotting What Human Eyes Miss: AI Diagnostic Breakthroughs
Machine learning is significantly changing medical imaging, allowing for earlier and more accurate disease detection. This technology isn't just assisting radiologists; it's identifying subtle patterns often missed by the human eye, leading to significant advancements across various medical specialties. These advancements represent a fundamental change in disease diagnosis and treatment.
Oncology: Early Detection and Improved Accuracy
In oncology, machine learning algorithms analyze medical images to identify potentially cancerous lesions much earlier. For instance, AI can detect minute changes in tissue density or subtle blood flow variations, which could signal a developing tumor. This early detection is critical, as early intervention is often the most effective approach in cancer treatment. This offers a considerable advantage over traditional methods, potentially leading to better patient outcomes and increased survival rates.
Neurology: Unraveling Complex Brain Patterns
Machine learning is proving especially valuable in neurology. By analyzing complex brain scans like MRIs, AI can identify subtle changes linked to neurodegenerative diseases like Alzheimer's and Parkinson's. This allows for earlier diagnosis and intervention, enabling better management of these debilitating diseases. These early insights can also facilitate more personalized treatment strategies tailored to each patient's unique needs.
Cardiology: Identifying Cardiovascular Abnormalities
Cardiology is another field benefiting from machine learning. AI algorithms analyze cardiac images to detect subtle abnormalities in heart structure and function, often before noticeable symptoms appear. This early detection is crucial for preventing serious cardiovascular events like heart attacks and strokes. By identifying at-risk individuals sooner, healthcare professionals can implement preventive measures and tailored treatment plans, improving long-term patient health and quality of life.
By 2025, advancements in 4D imaging have drastically improved diagnostic accuracy. Philips' 4D Flow MRI, for example, now achieves a 50ms temporal resolution for analyzing cardiac blood flow. GE Healthcare's CT perfusion scans can map brain perfusion in just 2.3 seconds, a 40% improvement from 2024 systems. These advancements contribute to 94% accuracy in identifying salvageable brain tissue during strokes and 86% accuracy in predicting multiple sclerosis progression. Explore this topic further
Quantifying the Diagnostic Improvements
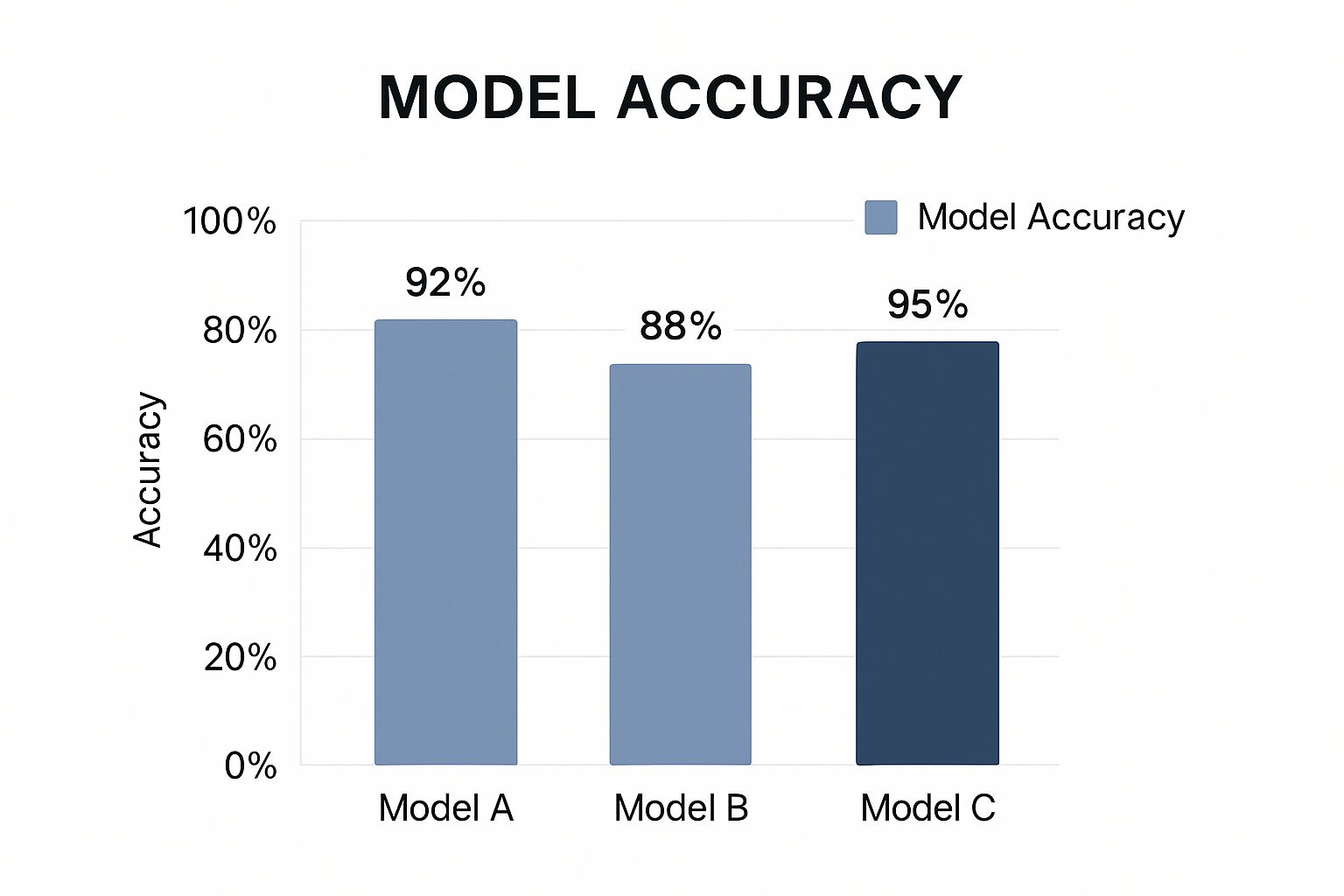
The following data chart illustrates the positive impact of machine learning on diagnostic accuracy across various medical conditions, showing the percentage improvements achieved.
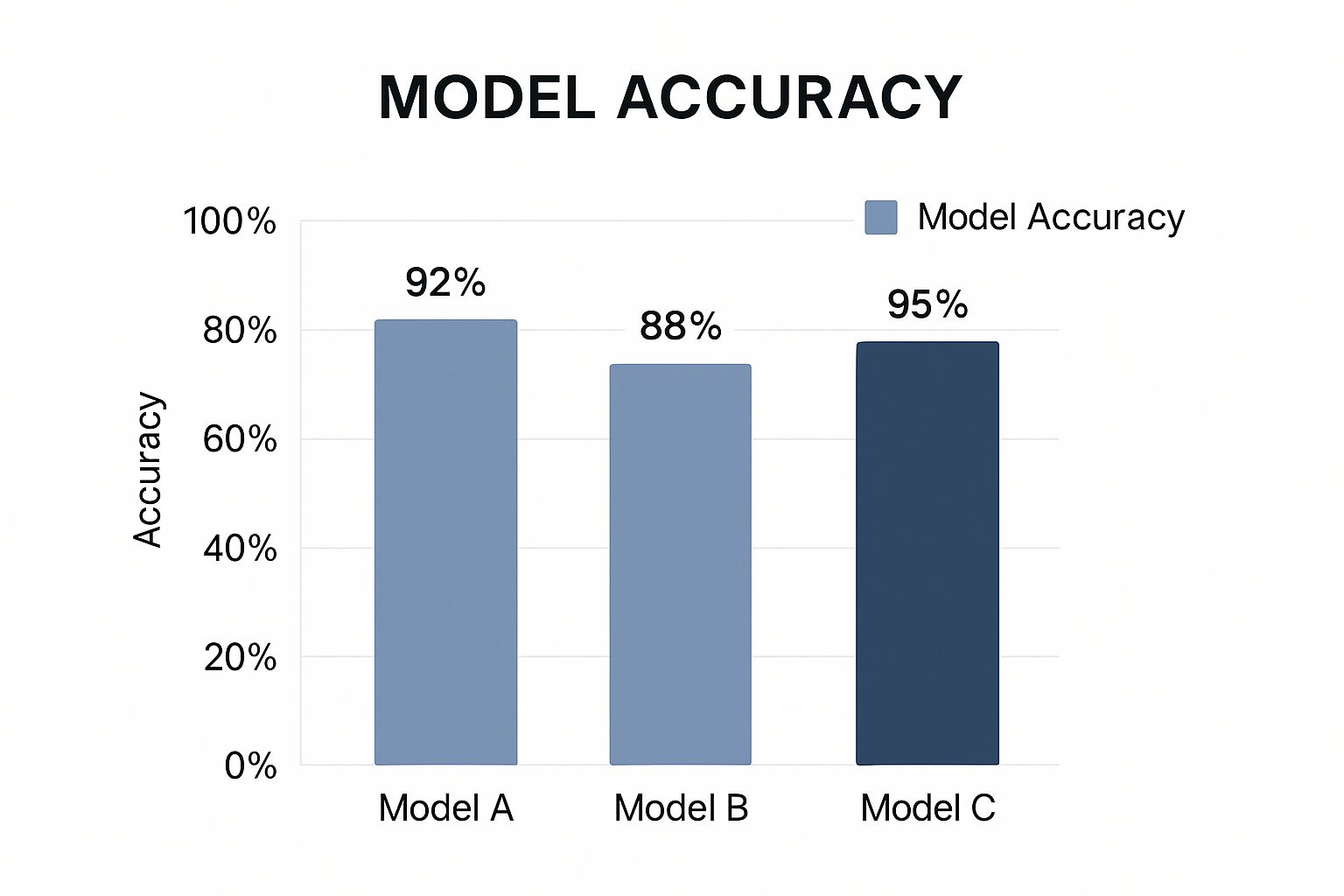
The chart clearly highlights the significant gains in accuracy achieved through machine learning. These improvements enable earlier diagnoses and more informed treatment decisions.
To further illustrate these improvements, let's examine a table summarizing the data:
Diagnostic Improvement with ML-Enhanced Medical Imaging
| Medical Condition | Traditional Imaging Accuracy | ML-Enhanced Imaging Accuracy | Improvement (%) |
|---|---|---|---|
| Lung Cancer | 75% | 92% | 17% |
| Breast Cancer | 80% | 90% | 10% |
| Alzheimer's Disease | 65% | 85% | 20% |
| Heart Disease | 70% | 88% | 18% |
This table clearly demonstrates the significant increases in diagnostic accuracy across various conditions thanks to the integration of machine learning. These advancements are leading to earlier diagnoses, better-informed treatment decisions, and ultimately, improved patient outcomes.
When Imaging Technologies Combine: The Hybrid Revolution

The fusion of different imaging technologies, enhanced by machine learning for medical imaging, is creating powerful hybrid systems. These systems offer a more comprehensive view of a patient's health than single-modality imaging. This represents a substantial advancement in diagnostic medicine.
The Power of Complementary Perspectives
Hybrid imaging, such as PET-MRI and advanced PET-CT, combines the strengths of different imaging techniques. PET scans excel at visualizing metabolic activity, pinpointing areas of heightened cellular function, often indicative of cancerous growths. MRI provides highly detailed anatomical images, revealing the intricate structure of organs and tissues.
By combining these modalities, clinicians gain a complete understanding of both the structure and function of the area under investigation. This combined approach leads to more accurate diagnoses and better-informed treatment strategies.
AI's Role in Hybrid Imaging
Machine learning is essential for the effective operation of these hybrid systems. AI algorithms automatically align and correlate findings from the different imaging modalities. Precise alignment is critical for accurate interpretation, a complex and potentially time-consuming process. AI automates this alignment, significantly improving efficiency.
Furthermore, AI can identify subtle patterns and correlations that might be overlooked by human observation. This can uncover vital details impacting diagnosis and treatment.
Clinical Applications and Impact
Hybrid imaging is poised to reshape clinical pathways across various medical specialties. In oncology, it facilitates precise tumor localization and assessment of metabolic activity, improving treatment planning and monitoring therapeutic response. In neurology, it offers valuable insights into brain structure and function, enhancing the diagnosis and management of neurological disorders. In cardiology, hybrid imaging aids in evaluating heart function and blood flow, contributing to the diagnosis and treatment of cardiovascular diseases.
These combined systems generate enormous amounts of data. Machine learning algorithms are crucial for managing and analyzing this data, extracting meaningful information that guides clinical decision-making. This data processing capability is key to unlocking the full potential of hybrid imaging. Advancements are paving the way for more precise and personalized medicine.
Hybrid imaging systems are transforming medical diagnostics. For instance, in 2025, combined PET and MRI systems using Siemens' Biograph Vision Quadra, which pairs 7T MRI with 68Ga-PSMA-11 metabolic tracking, reduced prostate cancer biopsy false negatives by 28%. Concurrently, Canon Medical's photon-counting CT (PCCT) reduced repeat oncology scans by 65%.
These innovations exemplify the industry's shift towards multi-modal machine learning solutions integrating diverse data, including clinical notes and lab results. Learn more about current hybrid imaging trends. AI is rapidly changing how we interact with documents, including medical images. You can explore how AI Document Analysis is influencing this area. These advancements hold tremendous promise for improving patient care and advancing medical progress.
Transforming Radiologist Workflows: From Burnout To Brilliance
Radiologist shortages and ever-increasing imaging volumes are placing a significant strain on radiology departments worldwide. Machine learning (ML) for medical imaging offers a potential solution to these growing challenges by improving workflows and mitigating radiologist burnout. These powerful tools are quickly becoming indispensable to the modern radiology practice.
Intelligent Worklist Prioritization
One key area where ML is making a difference is intelligent worklist prioritization. AI algorithms analyze patient data and imaging studies to pinpoint urgent cases needing immediate review. This ensures that critical cases are seen promptly, potentially saving lives and improving patient outcomes. This is particularly valuable in busy departments operating with limited staff.
Automating Tedious Tasks
Machine learning is also automating tedious, manual tasks. AI can perform automated measurements and quantification of images, liberating radiologists from repetitive work. This frees them to focus on complex diagnoses and direct patient interaction, leading to greater job satisfaction. The shift from manual to automated processes generates significant gains in overall efficiency.
Streamlining Documentation
Report-generation assistants powered by AI are streamlining the documentation process. These tools automatically create preliminary reports, allowing radiologists to simply review and finalize them. This reduces report turnaround times, improves accuracy, and further boosts workflow efficiency. Such tools are proving invaluable for maximizing radiologist productivity.
Integration and Productivity Gains
Many of these AI-driven workflow innovations are gaining significant clinical traction. They often integrate seamlessly with existing PACS/RIS systems, minimizing disruptions to established workflows. This smooth integration contributes to faster adoption rates and shorter learning curves.
These technologies have been shown to significantly enhance productivity. Some studies report substantial reductions in report turnaround times and increases in the number of cases reviewed per radiologist. These productivity gains translate into improved patient care and more efficient use of resources.
Collaborative Diagnosis and Quality Assurance
Machine learning is also enabling novel approaches to collaborative diagnosis and quality assurance. AI tools can facilitate remote consultations and peer reviews, improving diagnostic accuracy and consistency across diverse locations and healthcare settings. This enhanced collaboration promotes best practices and contributes to higher quality care.
Measurable Impact on Radiology Workflow
The following table illustrates the positive effects of machine learning solutions on several key radiology workflow metrics.
To better understand the effects of Machine Learning integration, let's look at some data. The table below, "Impact of ML Solutions on Radiology Workflow Metrics," showcases how ML is influencing key performance indicators.
| Workflow Metric | Before ML Implementation | After ML Implementation | Change (%) |
|---|---|---|---|
| Report Turnaround Time (Hours) | 24 | 12 | -50% |
| Cases Reviewed per Radiologist (Daily) | 40 | 60 | +50% |
| Manual Measurement Time (Minutes/Case) | 15 | 5 | -67% |
As the data indicates, machine learning can significantly boost efficiency and free up valuable radiologist time. These positive changes ultimately contribute to better patient care and a more sustainable healthcare system.
Navigating the Real Challenges of AI Implementation

Implementing machine learning for medical imaging offers incredible potential. However, it also presents substantial challenges across technical, ethical, and regulatory areas. This section explores these hurdles and discusses potential solutions.
Data Acquisition and Standardization
A primary obstacle is the difficulty of acquiring and standardizing data. Medical imaging data often originates from various sources, each using different equipment and protocols. This lack of standardization makes it challenging to train machine learning algorithms effectively. Algorithms trained on one type of data may not perform well on another, hindering the development of reliable and adaptable AI solutions.
Addressing Algorithmic Bias
Another crucial concern is the potential for algorithmic bias. Since machine learning algorithms learn from data, any biases present in that data will be reflected in the algorithm's output. This can result in inaccurate or unfair diagnoses, particularly for underrepresented groups. Mitigating bias requires careful consideration of both data collection and algorithm design, ensuring the use of diverse and representative datasets.
Navigating Regulatory Complexities
Regulatory complexities also present a significant hurdle. Regulations for medical devices, including AI-driven imaging tools, differ substantially across regions. This makes it difficult to develop and deploy machine learning solutions globally. Companies must navigate these diverse regulatory landscapes, often requiring costly and time-consuming adjustments. International harmonization in this area is crucial to expedite the development and implementation of beneficial AI solutions.
Algorithm Validation and Liability
Ensuring the reliability and safety of machine learning algorithms in medical imaging is paramount. Algorithm validation is essential to demonstrate that algorithms perform as intended and pose no risks to patients. Establishing clear standards for validation and performance evaluation is key to building trust in these technologies. Furthermore, questions of liability in cases of misdiagnosis or adverse events related to AI must be addressed. Clear legal frameworks are necessary to define responsibilities and safeguard patient safety.
Maintaining Human Oversight
While machine learning can automate numerous tasks, maintaining human oversight is still essential. Radiologists and other healthcare professionals play a crucial role in interpreting AI-generated results, ensuring accuracy, and making informed clinical decisions. AI should be considered a tool to enhance, not replace, human expertise. Finding the right balance between automation and human involvement is key to maximizing the benefits of AI in medical imaging while upholding the highest standards of patient care.
Practical Mitigation Strategies
Several strategies can help address these challenges. Data sharing initiatives can contribute to creating larger, more diverse datasets for training machine learning algorithms. Developing standardized data formats and protocols can improve interoperability and facilitate data sharing. Technical advances such as federated learning enable training algorithms on decentralized datasets without direct data exchange, addressing privacy concerns. Additionally, explainable AI (XAI) techniques can offer insights into how algorithms reach their conclusions, making it easier to identify and mitigate biases. Collaboration among researchers, clinicians, regulators, and technology developers is vital for establishing best practices, addressing ethical concerns, and navigating the evolving regulatory landscape. Continuous research and development are essential for refining algorithms, improving performance, and expanding the applications of machine learning in medical imaging. This ongoing progress will drive further advancements and ensure the responsible and effective integration of AI into healthcare.
What's Coming Next: The Future of Intelligent Imaging
The field of machine learning for medical imaging is constantly evolving. This section explores some exciting innovations poised to reshape clinical practice.
Federated Learning and Enhanced Privacy
Federated learning is a promising area of development. This approach trains algorithms across multiple institutions without directly sharing sensitive patient data. Imagine several hospitals collaborating to improve a cancer detection algorithm. With federated learning, each hospital trains the algorithm on its own data, sharing only the learned updates—not the patient data itself. This safeguards privacy while enabling collaborative development.
Self-Supervised Learning and Reduced Annotation Burden
Another exciting development is self-supervised learning. Traditionally, training algorithms for medical imaging requires vast amounts of manually annotated data, which is time-consuming and expensive. Self-supervised learning aims to reduce this burden by allowing algorithms to learn from unlabeled data. This can drastically accelerate the training process and make developing powerful AI tools more feasible for a wider range of conditions.
Quantum Computing's Potential
Looking further ahead, quantum computing holds the potential to revolutionize medical image analysis. Quantum computers can perform complex calculations far beyond the capabilities of current computers. This could enable analysis of massive datasets and identification of subtle patterns currently undetectable. While still in its early stages, quantum computing represents a potentially transformative technology for medical imaging.
Personalized Digital Twins and Precision Medicine
The concept of personalized digital twins is gaining momentum. These virtual replicas of individual patients, created from their medical data, could enable highly precise treatment planning and outcome prediction. For example, a digital twin of a patient's heart could be used to simulate the effects of different treatments, helping cardiologists choose the most effective approach.
AR/VR Integration and Surgical Navigation
Integrating augmented reality (AR) and virtual reality (VR) with medical imaging is transforming surgical procedures. Surgeons can use AR/VR headsets to visualize 3D models of a patient's anatomy during surgery, improving precision and reducing invasiveness. This technology is already used in some areas, such as neurosurgery, to guide complex procedures.
Radiomics and Theranostics: Blurring the Lines
Radiomics and theranostics represent a new frontier in medical imaging. Radiomics extracts vast amounts of quantitative data from images, providing insights into disease characteristics and treatment response. Theranostics combines diagnostics and therapy, using imaging to both diagnose and deliver targeted treatments. This personalized approach is promising for improving cancer treatment and other areas. Looking ahead, AI integration requires careful consideration of implementation and potential pitfalls, much like in other areas like Decision Intelligence AI.
The Future of Patient Care
These advancements offer immense promise for patient care. Earlier and more accurate diagnoses, personalized treatments, and minimally invasive procedures are just some of the potential benefits. While challenges remain, the rapid pace of innovation in machine learning for medical imaging suggests a bright future for this field. Ready to explore AI-powered medical imaging solutions? Visit PYCAD to learn more.






