Getting a medical device from an idea into the hands of a doctor or patient is a long and winding road. That road has a name: the medical device regulatory pathway. This is simply the specific set of steps and documents required by agencies like the FDA in the U.S. or European authorities before you can legally sell your product.
Think of it as the official, government-mandated blueprint you must follow. Its purpose is to ensure you've proven, beyond a doubt, that your device is both safe and effective for its intended use.
Charting Your Course Through Global Regulations
Navigating the global market for medical devices often feels like captaining a ship across a vast ocean. The regulatory pathway is your nautical chart, breaking down what seems like an overwhelming voyage into a series of clear, manageable legs. This guide is here to cut through the bureaucratic fog and show you how a smart regulatory strategy is one of the most powerful tools you have.
The analogy of a ship captain holds true. You wouldn't use the same chart for the Atlantic as you would for the Pacific, and the same goes for medical devices. Each market has its own currents, shoals, and safe harbors. For instance, the US FDA handles most reviews in-house, whereas the European Union delegates this authority to independent third-party organizations called "Notified Bodies."
Understanding the Key Territories
We're going to focus on the major regulatory territories that most device makers will face on their journey. The goal is to give you the practical knowledge to turn what feel like regulatory hurdles into genuine strategic advantages.
We’ll explore:
- The United States FDA: We'll dive into the main approval routes: the 510(k), Premarket Approval (PMA), and De Novo pathways.
- Europe's MDR (Medical Device Regulation): We'll demystify the role of Notified Bodies, explain the heavy emphasis on clinical evidence, and break down the idea of a "living" technical file that requires constant updates.
- Global Considerations: While our primary focus is the US and EU, we'll touch on how mastering these two frameworks gives you a major head start in other markets around the world.
A well-defined regulatory strategy isn't just a compliance checkbox; it's a core pillar of your business plan. It directly impacts your product design, clinical trial budgets, marketing claims, and even your timeline to profitability.
At the end of the day, this guide offers a practical blueprint. It’s based on the real-world frameworks that successful manufacturers use to bring their innovations to the people who need them. By understanding the rules of the road in each major market, you can plan a more direct, predictable, and successful journey from concept to clinic.
Building on a Foundation of Device Classification

Before you can even think about submitting paperwork or scheduling audits, every single regulatory journey starts with one crucial step: correctly classifying your medical device.
Think of it like building a house. You wouldn't use the foundation for a garden shed to support a skyscraper—the whole thing would be doomed from the start. It’s the same with medical devices. If you get the classification wrong, every subsequent step, from testing to documentation, will be built on a faulty premise.
Regulators, whether it's the FDA in the U.S. or authorities in the European Union, all use the same core principle to classify devices: the potential risk they pose to patients and users. This single concept dictates your entire path to market. A low-risk device will have a relatively straightforward path, whereas a high-risk one will face a gauntlet of intense scrutiny, demanding robust clinical data.
While the two major systems—from the US and EU—share this risk-based logic, their structures have some key differences. Let's break them down.
US FDA Device Classification
In the United States, the FDA keeps things fairly direct, sorting devices into three classes using Roman numerals. It's a clear progression from low to high risk.
-
Class I: These are your low-risk devices, the ones with the least potential to cause harm. They make up nearly half of all devices on the market and are subject to what are called "General Controls." Think elastic bandages, tongue depressors, or a standard manual wheelchair.
-
Class II: This is the broad, moderate-risk category where most devices land. General Controls aren't enough here, so they also require "Special Controls," which might mean adhering to specific performance standards or conducting post-market surveillance. The vast majority of these devices need a Premarket Notification (510(k)) submission to prove they are substantially equivalent to a device already on the market. Examples include powered wheelchairs, infusion pumps, and most surgical drapes.
-
Class III: This is the big one. These are the highest-risk devices, often ones that are implanted, sustain life, or carry a significant potential for illness or injury if they fail. They require the most demanding review, a Premarket Approval (PMA). We're talking about devices like pacemakers, artificial heart valves, and automated external defibrillators (AEDs).
European Union MDR Classification
Across the Atlantic, the European Union’s Medical Device Regulation (MDR) gets a bit more granular, expanding the system into four main classes. This allows for more nuance, especially in the middle-risk tiers.
The rulebook for the EU MDR is Annex VIII. It lays out the specific criteria—like duration of use, how invasive it is, and whether it uses a power source—that determine a device's final classification.
Here’s how the EU breaks it down:
- Class I: Low-risk, just like in the US. However, this class has important subcategories for devices that are sold sterile (Is), have a measuring function (Im), or are reusable surgical instruments (Ir).
- Class IIa: Low to medium-risk devices. This is where you’ll find things like hearing aids or surgical clamps.
- Class IIb: Medium to high-risk devices. This category includes more critical products like ventilators and blood bags.
- Class III: The highest-risk devices, much like the US equivalent. These include life-sustaining or implantable products like cardiovascular catheters and prosthetic heart valves.
To give you a clearer picture, here's a side-by-side comparison of how these two major systems stack up.
US FDA vs EU MDR Device Classifications at a Glance
| Risk Level | US FDA Class | Example (US) | EU MDR Class | Example (EU) |
|---|---|---|---|---|
| Lowest | Class I | Elastic Bandage | Class I | Stethoscope |
| Low-Medium | Class II | Infusion Pump | Class IIa | Hearing Aid |
| Medium-High | Class II | Ventilator | Class IIb | Blood Bag |
| Highest | Class III | Pacemaker | Class III | Prosthetic Heart Valve |
As you can see, while the risk levels align, the specific class names and the kinds of devices that fall into them can differ. This is why you can't just assume your FDA class will translate directly to the EU.
Understanding the broader context of how devices are made is also incredibly helpful. For example, learning about the impact of LVDT sensors on medical device manufacturing shows how even a single component's quality can ripple through the entire design, a key point in any regulatory filing.
Ultimately, classification isn't just a box-ticking exercise. It dictates your documentation, your clinical trial requirements, and the very nature of your submission. Nailing it from day one is one of the most effective ways to save time, money, and headaches on your path to market.
Mastering US FDA Regulatory Pathways
Once you've figured out your device's classification, the map to the US market starts to look a lot clearer. The Food and Drug Administration (FDA) has three main highways for getting a medical device cleared or approved. Knowing which route to take is absolutely fundamental to your entire commercialization strategy.
Think of it like getting a building permit. A permit for a backyard shed (low-risk) is pretty straightforward. But for a skyscraper? That's a whole different story, demanding extensive architectural plans, engineering reports, and rigorous safety inspections. The FDA’s system works on the exact same principle: the level of scrutiny must match the level of risk.
The following graphic gives you a bird's-eye view of the universal stages every manufacturer goes through during the pre-market submission process.
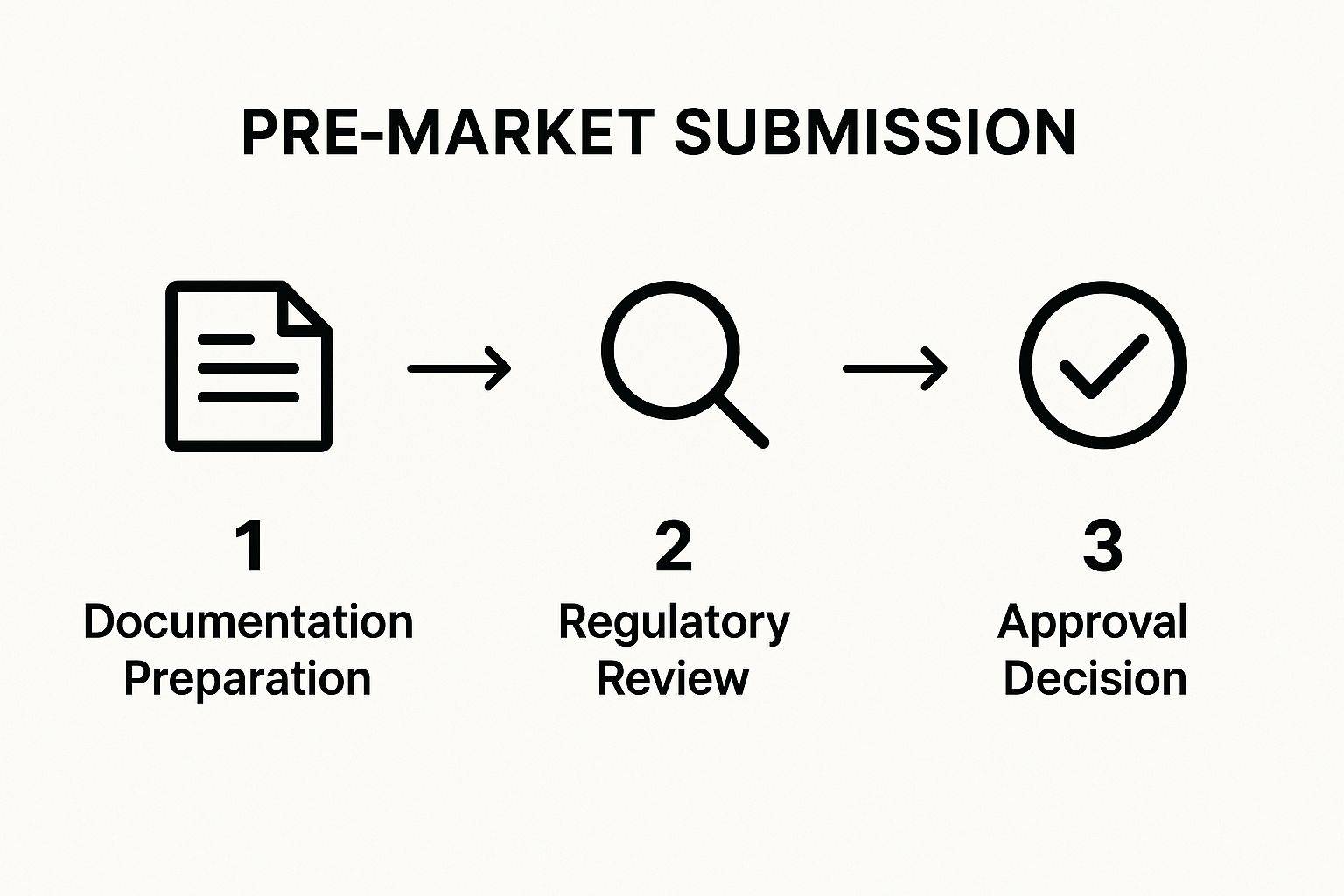
This flow, from initial prep work to the final decision, highlights just how structured the regulatory journey is, no matter which specific path you end up on.
The 510(k) Pathway for Moderate-Risk Devices
By far, the most common route to market is the Premarket Notification, which everyone in the industry simply calls a 510(k). This is the designated path for most Class II devices and even a few Class I devices. It's important to know this isn't an "approval" process; it's a "clearance" process. There's a big difference.
The entire 510(k) submission boils down to one critical concept: substantial equivalence. To get clearance, you have to prove your device is as safe and effective as a legally marketed device that's already out there. We call this existing device a predicate device.
So, what does proving substantial equivalence actually involve? You need to show that your new device:
- Has the same intended use as the predicate.
- Shares similar technological characteristics.
- If the technology differs, you must demonstrate the new device is at least as safe and effective as the predicate.
The Premarket Approval (PMA) Path for High-Risk Devices
For Class III devices—the ones that sustain life, are implanted, or pose a potential unreasonable risk of illness or injury—the 510(k) path is off the table. These devices have to go through Premarket Approval (PMA), which is the most stringent, in-depth review the FDA conducts.
A PMA is a full-blown scientific and regulatory evaluation of your device's safety and effectiveness. Unlike a 510(k), you aren't just comparing your device to something else. You have to generate your own valid scientific evidence, which means extensive lab testing, animal studies, and human clinical trials. You're proving safety and efficacy from scratch, making the PMA process significantly more expensive and time-consuming.
The De Novo Pathway for Novel Devices
So what happens when your device is new and innovative, low-to-moderate risk, but has no predicate on the market to compare it to? This is exactly why the De Novo classification request exists. It carves out a path for new types of devices that would otherwise be automatically lumped into Class III just because there's no precedent.
The De Novo process lets the FDA review the device on its own merits. If the agency finds it to be low-to-moderate risk, it can authorize its marketing and create an entirely new classification. Better yet, this newly classified device can then be used as a predicate for future 510(k) submissions from other companies.
Key Takeaway: The 510(k) is all about comparison to an existing device. The PMA is about proof of safety and efficacy. The De Novo is about creating a new category for a novel, lower-risk device.
Accelerating Access with the Breakthrough Devices Program
To get certain crucial medical technologies to patients faster, the FDA created special programs. The Breakthrough Devices Program (BDP) is a big one, designed for devices that offer a more effective way to treat or diagnose life-threatening or irreversibly debilitating diseases.
This program gives you a prioritized review and much more interaction with the FDA team. Between 2015 and early 2024, the FDA granted this designation to 1,041 devices. But a designation is not a guarantee of approval—only 12.3% of them received marketing authorization in that same period. Still, for those that do, the review times are significantly faster than the standard pathways.
The web of FDA rules can feel complex. For a bit more context on how the agency operates, you can see how their approach differs for other products in this guide to FDA Regulations for Dietary Supplements, which provides a useful comparison.
Succeeding Within the EU MDR Framework

If you're looking to enter the European market, you need to master a completely different playbook than the one used in the United States. The Medical Device Regulation (MDR) is the law of the land here, creating a single, rigorous framework across all EU member states. It’s like learning the specific rules of the road for a new, continent-wide highway system.
Unlike the US FDA, which is a government body that directly reviews submissions, the EU uses a decentralized system. The gatekeepers to the European market are independent, third-party organizations called Notified Bodies. These are state-appointed commercial entities tasked with auditing manufacturers and certifying that a device meets the MDR’s demanding standards. Their stamp of approval is the CE Marking—the mandatory passport your device needs for market access.
This structural difference fundamentally changes the entire medical device regulatory pathway for companies selling in Europe. Your key relationship isn't with a government agency but with a certified private partner whose job is to enforce public safety rules with an exacting eye.
The Core Pillars of MDR Compliance
The MDR didn't just tweak the old rules; it significantly raised the bar for what it means to be compliant. It's built on a foundation of continuous vigilance, shifting the focus away from a one-time approval. Three pillars, in particular, define this modern approach to regulation and patient safety.
These pillars are:
-
Heightened Clinical Evidence: The MDR places a huge emphasis on solid clinical data. You’ll need to put together a Clinical Evaluation Report (CER) that proves, without a doubt, your device's safety and performance for its intended purpose. This isn't a "file it and forget it" report; it must be actively updated throughout the device's entire life on the market.
-
Total Lifecycle Traceability: A comprehensive Unique Device Identification (UDI) system is now non-negotiable. Every single device needs a UDI, making it possible to track it from the manufacturing line all the way to the patient. This creates a powerful layer of transparency and enables swift, precise action if a safety concern ever pops up.
-
Stringent Post-Market Surveillance (PMS): Under the MDR, Post-Market Surveillance is no longer a passive, reactive task. Manufacturers are now mandated to systematically gather and analyze real-world data on how their device performs after it’s sold. This proactive monitoring is designed to catch potential safety issues early.
Your Technical File as a Living Document
Perhaps the biggest mental adjustment the MDR demands is viewing your technical file as a "living" document. In the past, you might have seen the technical dossier as a static binder of paperwork you assembled for that initial approval. Not anymore.
The MDR treats your technical documentation not as a snapshot, but as a continuously updated biography of your device. It must evolve with new clinical data, post-market feedback, and any design modifications, reflecting the device's entire lifecycle.
This means your Quality Management System (QMS) has to be robust enough to handle this dynamic process. For instance, if your PMS work uncovers a previously unknown risk, that new information has to flow back into your risk management file, your clinical evaluation, and maybe even your instructions for use.
These pieces aren't separate silos; they are all interconnected. A change in one document triggers a ripple effect, requiring you to review others to maintain consistency and compliance. To succeed with the EU MDR, you have to embrace this philosophy of sustained vigilance. It's about seeing regulatory compliance as an ongoing commitment to safety and performance, not just a hurdle to clear once. This is what defines the modern European medical device regulatory pathway.
Building Your Submission Dossier: The Blueprint for Approval
Putting together your submission isn't just a data dump. I always tell my clients to think of it like they're building a meticulous legal case for a high-stakes trial. Your goal is to present a bulletproof, evidence-backed argument that proves your device is safe and does exactly what you say it does. A sloppy, disorganized file is one of the quickest ways to get hit with delays or an outright rejection.
This collection of documents—your submission dossier, technical file, or technical documentation—is where all your hard work in engineering, clinical research, and quality control comes together. Regulators don't just skim this; they pore over every detail, searching for a single, logical story where every piece of evidence backs up the next.
The Essential Files in Your Dossier
While the specific document list changes a bit depending on your device class and where you want to sell it (the FDA's requirements aren't identical to the EU's MDR, for instance), a few key files are non-negotiable. And they aren't just separate documents; they’re all interconnected parts of your device's story.
-
Design History File (DHF): This is your device's complete biography. It chronicles every design choice, test, review, and validation step, proving you followed a controlled process to create the final product.
-
Risk Management File (RMF): Guided by the ISO 14971 standard, this file is your deep dive into everything that could possibly go wrong. It shows you've identified every potential risk, analyzed its severity, and implemented controls to bring that risk down to an acceptable level.
-
Clinical Evaluation Report (CER) or Performance Evaluation Report (PER): Here’s where you lay out the clinical proof that your device is safe and performs as intended. For some devices, you can do this by analyzing existing scientific literature, but for higher-risk products, you’ll need to present data from your own clinical investigations.
Crafting a Single, Cohesive Story
The biggest rookie mistake I see is when companies treat these documents like separate items on a checklist. Regulators are trained to spot inconsistencies from a mile away. For example, if your Risk Management File mentions a specific risk of misuse, your Instructions for Use (IFU) and labeling better have clear, explicit warnings about that exact scenario.
A classic red flag is a gap between the risks flagged in the RMF and the evidence presented in the CER. If your risk analysis identifies a potential hazard, your clinical data must directly show that this hazard has been controlled or eliminated.
Everything has to connect. Every single claim you make about performance needs to be supported by your design verification, validated with clinical evidence, and accounted for in your risk assessment. As you put your dossier together, a solid understanding of regulatory compliance in labelling is absolutely critical to getting it right the first time.
The real power of your submission lies in this internal consistency. It should tell one clear, logical story: you understood the clinical need, designed a device to meet it, identified all the risks, proved its safety and effectiveness with solid data, and provided clear instructions to the end-user. Getting this narrative right is the heart of a successful regulatory strategy.
The Strategic Value of Outsourcing Regulatory Affairs
As global regulations get more tangled, medical device companies hit a fork in the road. Do you try to map the complex medical device regulatory pathway on your own, or do you bring in an expert guide? This decision—building an in-house team versus outsourcing—is one of the most important strategic calls a company can make.
The pressure is definitely on. Tougher rules in key markets and the constant push to get products to patients faster have created a huge demand for specialized know-how. This is especially true for companies working on next-generation products, like those using AI, where the regulatory rulebook is often still being written.
You can see this demand reflected in the numbers. The global market for medical device regulatory affairs was valued at roughly USD 6.75 billion in 2024 and is expected to climb to USD 11.66 billion by 2030. That growth, a compound annual growth rate (CAGR) of about 9.5%, is a direct result of these complicated regulations and the need for speed. You can dig deeper into the drivers behind this market expansion to learn more.
The Core Benefits of Partnering with Experts
Bringing on a regulatory affairs consultant isn't just about handing off paperwork. It's about gaining a serious strategic advantage. Think of them as a seasoned captain who has navigated these treacherous waters hundreds of times—they know exactly where the hidden rocks and dangerous currents are.
The primary benefits really boil down to a few key things:
- Deep, Specialized Knowledge: A great partner doesn't just know the regulations; they have hands-on experience with specific device types and global markets, from the FDA's nuances to the EU MDR's complexities. This is the kind of expertise that takes an internal team years to build.
- Catching Problems Early: Experienced consultants are pros at spotting potential regulatory red flags long before they become expensive problems. This foresight can prevent costly redesigns and frustrating submission delays down the line.
- Smarter Use of Time and Money: Yes, there's an investment, but outsourcing can be far more cost-effective than hiring, training, and keeping a senior-level regulatory staff. It also frees up your core R&D and engineering teams to do what they do best: innovate.
When you hire an external expert, you're essentially "renting" years of hard-won experience. They bring immediate value, applying lessons from countless other submissions to make sure yours is as smooth and successful as possible.
Choosing the Right Regulatory Partner
Finding the right guide is critical, because not all regulatory consultants are the same. When you're vetting a partner to help you navigate your medical device regulatory pathway, the first thing you should look for is a proven track record with devices like yours.
Don't be shy about asking for case studies and talking to their past clients. Dig into their specific experience with the agencies you're targeting, whether it's the FDA, a particular EU Notified Body, or another country's health authority. The right partner becomes a true extension of your team, turning regulatory compliance from a barrier into a genuine competitive advantage.
Your Medical Device Pathway Questions Answered
The world of medical device regulations is full of twists and turns, where a tiny misstep can lead to major setbacks. Think of this as your personal Q&A session, where we tackle the tough questions that pop up time and time again for device creators.
Getting through this process smoothly is all about knowing what's coming and being ready for it. So, let's dive into some of the most common queries.
How Long Does the Medical Device Approval Process Take?
This is the million-dollar question, and the honest answer is: it depends. The timeline is almost completely dictated by your device's risk class and the specific regulatory path you take. There's no one-size-fits-all schedule, but we can look at some typical timeframes.
- In the US, a low-risk Class I device might just need a few weeks for basic registration. Simple.
- The standard 510(k) pathway for a Class II device generally takes the FDA anywhere from 3 to 9 months to review and clear.
- For a high-risk Class III device, the intensive PMA pathway is a much longer haul, often taking 1 to 3 years, sometimes more. The extensive clinical trial data required is the main reason for the longer wait.
Over in the European Union, the conformity assessment process under the MDR with a Notified Body can run from 12 to 24 months. This timeframe can stretch depending on how complex your device is and how busy your Notified Body is at the moment.
What Are the Most Common Mistakes That Delay Approval?
It’s frustrating, but many submissions get tripped up by mistakes that could have been avoided. Here are the most common pitfalls that cause long delays or even outright rejections:
- Incorrect Device Classification: This is a classic blunder. Starting on the wrong path from day one means all your subsequent work is built on a faulty foundation.
- Inconsistent Dossier: This happens when different parts of your submission don't tell the same story—for example, your risk analysis doesn't match up with your clinical evaluation. Regulators spot this immediately.
- Insufficient Clinical Evidence: You have to provide solid, convincing data that proves your device does what you claim it does, safely and effectively. Weak evidence is a major red flag.
- Poorly Defined 'Intended Use' Statement: If your core statement about what the device is for is vague or confusing, it creates a cascade of questions from regulators.
A frequent and costly mistake we see is giving incomplete answers to regulators' questions during the review. Every time you send back a partial response, you can add months to your timeline. Being thorough from the start is non-negotiable.
What Is a Predicate Device?
A "predicate device" is a key concept in the US system. It's an existing, legally marketed device—usually one that was cleared through the 510(k) process—that you can use as a point of comparison.
To get your own device cleared via the 510(k) pathway, you have to prove that your new device is "substantially equivalent" to a predicate. This means showing it has the same intended use and very similar technology. If your tech is a bit different, you’ll need to provide performance data to convince the FDA that it's at least as safe and effective as the device you're comparing it to.
At PYCAD, we live at the complex intersection of AI and medical imaging. We help manufacturers generate the powerful, reliable data needed to build a successful regulatory submission. If you're creating an AI-powered medical device, learn how our expertise can speed up your journey to market.






