Mastering Medical Image Annotation Fundamentals
Medical image annotation is the foundation of modern AI in healthcare. It involves labeling medical images, such as X-rays, MRIs, and CT scans, to create training datasets for machine learning algorithms. This process teaches AI systems to interpret the complexities of medical imagery, aiding in diagnosis and enhancing patient care.
Understanding The Importance of Accurate Annotations
Different medical images require different annotation methods. Bounding boxes might suffice for identifying organs in a CT scan. However, outlining a tumor's precise boundaries necessitates more detailed techniques like polygonal segmentation or landmark annotation. This precision is vital for training algorithms to detect subtle anomalies, providing the accuracy required for effective AI-driven diagnoses.
The importance of this field is reflected in market growth. The global medical image annotation market has expanded significantly, fueled by advancements in artificial intelligence (AI) and machine learning (ML). Reaching $1.2 billion in 2023, it's projected to reach $4.5 billion by 2032. This growth underscores the rising demand for annotated medical images in developing AI diagnostic tools. Learn more about this growth in the medical image annotation market. This demand is driven by the need for high-quality annotated datasets to improve the accuracy of AI models in medical diagnosis and treatment.
Quality Control: The Key To Reliable AI

Maintaining high-quality annotation is paramount, particularly for critical diagnoses. Leading medical institutions implement rigorous quality control. This includes detailed annotation guidelines, comprehensive annotator training, and multiple reviews by expert radiologists. These measures minimize errors and ensure reliable training data.
Annotation Standards and Best Practices
Standardized annotation practices are becoming industry benchmarks. These standards promote consistency across projects and institutions, encouraging collaboration and improving the adaptability of AI models. Adopting these best practices is essential for developing robust and dependable AI solutions in healthcare. This standardization also simplifies the integration of new tools and technologies.
Breakthrough Techniques Transforming Medical Image Annotation
Medical image annotation is no longer a simple process of tagging. Advanced techniques are now propelling advancements in medical AI, turning basic medical images into powerful diagnostic resources. This section will explore several key techniques, including bounding boxes, polygonal segmentation, and landmark annotation, and how they are applied in various medical contexts.
Bounding Boxes: Rapid Annotation for Object Detection
Bounding boxes are simply rectangles drawn around the objects of interest in an image. This technique is highly efficient for quickly identifying and locating important structures like organs or lesions. For example, in radiology, bounding boxes can be instrumental in training algorithms to detect lung nodules. However, it's important to note that this method lacks the precision necessary for detailed boundary delineation.
Polygonal Segmentation: Precise Outlines for Complex Structures
When precise boundaries are critical, polygonal segmentation becomes essential. This method involves carefully tracing the outline of a structure using connected line segments, much like creating a connect-the-dots drawing. This process allows for highly accurate representations of complex shapes. It's particularly valuable in oncology, where accurately defining the margins of a tumor is vital for effective treatment planning. Accurately marking and labeling specific areas in medical images is crucial. For a broader look at annotation, see this guide on how to annotate a PDF.
Landmark Annotation: Pinpointing Key Features for Analysis
Landmark annotation focuses on identifying specific points of interest. It's similar to placing pins on a map to mark important locations. In dermatology, this technique can precisely pinpoint the location of skin lesions and track their development over time. Landmark annotation is also extremely valuable in the analysis of facial features and bone structures.
Combining Techniques for Enhanced Accuracy
Annotation teams often combine multiple techniques to maximize effectiveness. For example, bounding boxes might be used for initial object localization, followed by polygonal segmentation for a more precise boundary definition. This layered approach improves both efficiency and accuracy, creating higher-quality datasets for AI training.
Semi-Automated and Automated Approaches: Boosting Efficiency
Semi-automated tools assist annotators by suggesting initial annotations, which are then reviewed and refined by human experts. Fully automated methods, on the other hand, rely on pre-trained algorithms to perform the annotation process entirely without human intervention. The infographic below compares manual, semi-automated, and automated annotation techniques, highlighting their differences in average annotation time and accuracy rates.
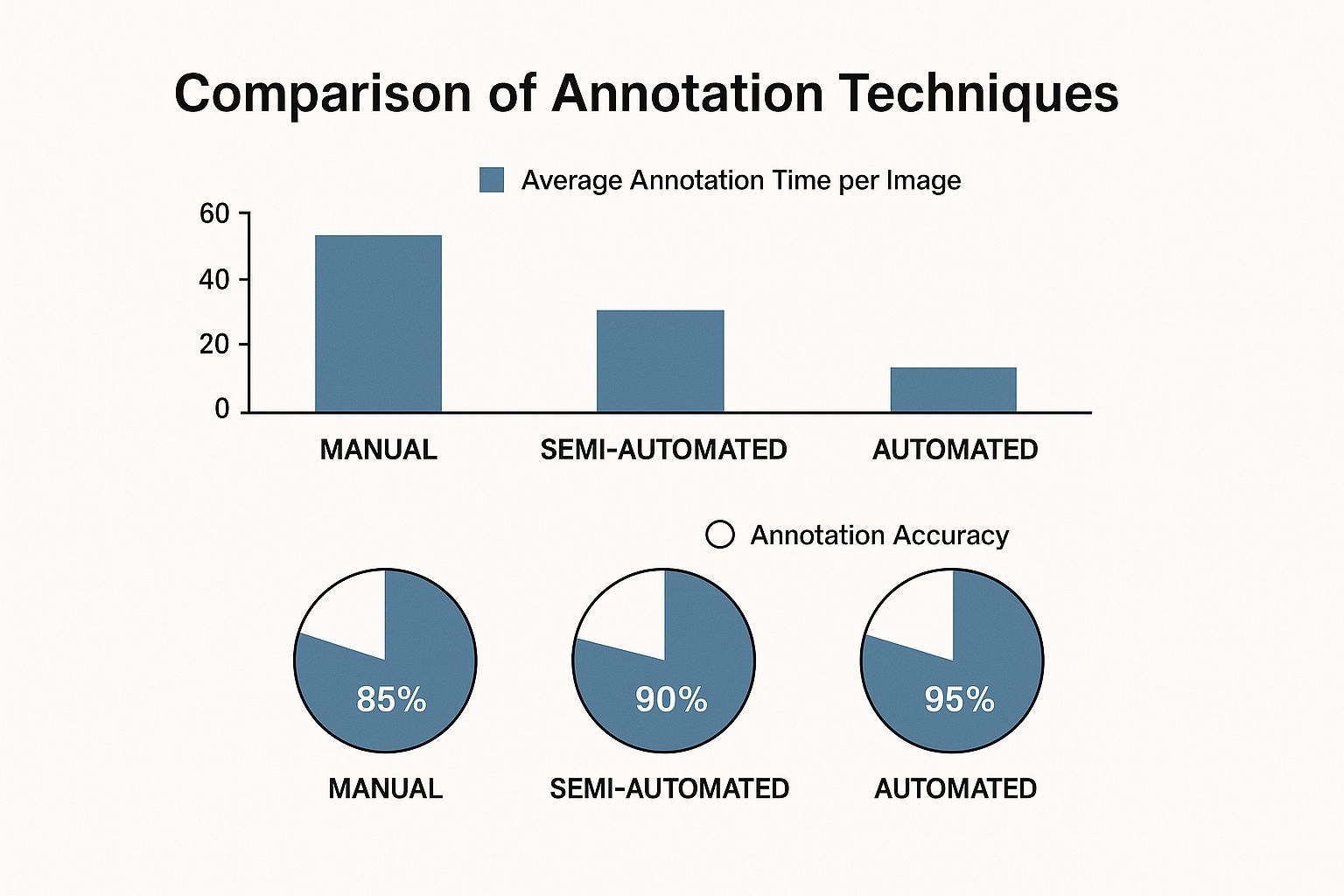
The infographic demonstrates that while automated annotation is the fastest, it often sacrifices accuracy compared to manual or semi-automated methods. This underscores the continued importance of human oversight, particularly in critical diagnostic applications where accuracy is paramount. Semi-automated techniques offer a valuable balance between speed and precision, potentially streamlining annotation workflows without compromising quality. Ongoing research and development efforts remain focused on creating robust and accurate automated annotation methods.
To further understand the nuances of these techniques, let's examine a comparison table.
The following table, "Comparison of Medical Image Annotation Techniques," provides a more detailed overview of the strengths, weaknesses, and ideal use cases for each method.
| Annotation Technique | Best Use Cases | Accuracy Level | Time Investment | AI Compatibility |
|---|---|---|---|---|
| Bounding Boxes | Identifying and locating large structures (e.g., organs, tumors) | Moderate | Low | High |
| Polygonal Segmentation | Delineating complex shapes and boundaries (e.g., tumor margins, organ contours) | High | Medium | High |
| Landmark Annotation | Pinpointing specific features (e.g., lesion location, facial features) | High | Medium | High |
| Semi-Automated Annotation | Combining speed and accuracy for various applications | High | Medium | High |
| Automated Annotation | High-volume annotation tasks, initial object detection | Moderate | Low | High |
This table summarizes the key differences between the annotation techniques, showing how each method offers specific advantages depending on the particular application. The choice of technique depends on the balance between the required level of accuracy and the available time and resources. While automated solutions are rapidly improving, human expertise remains crucial for achieving the highest levels of accuracy in medical image annotation.
Selecting Powerful Tools for Medical Image Annotation
Choosing the right medical image annotation tool is crucial for the success of any AI project in healthcare. The decision requires careful evaluation of several factors, including project-specific needs, team expertise, and available resources. This section explores the key considerations when selecting annotation software.
Balancing Open-Source and Commercial Platforms
Many institutions face the decision of choosing between open-source and commercial annotation platforms. Open-source options offer flexibility and cost-effectiveness. Commercial platforms often provide greater reliability, dedicated support, and advanced features. Top research hospitals sometimes strike a balance. They may use open-source tools for simpler tasks and commercial platforms for complex projects needing specialized functionalities.
Healthcare-Specific Requirements: DICOM and HIPAA
Medical image annotation tools must adhere to healthcare regulations. DICOM compatibility is essential for handling medical image formats, ensuring seamless integration with hospital systems. HIPAA compliance is mandatory for protecting patient privacy and data security. Choosing tools that meet these standards is paramount for any project involving patient data.
Integration Challenges and Solutions
Integrating annotation platforms with existing hospital systems can present challenges. Data formats, security protocols, and workflow compatibility can create hurdles. Successful teams overcome these by carefully planning and collaborating between IT and medical professionals. They select platforms with strong integration capabilities. This collaborative approach is essential for smooth data flow and efficient project execution.
Security and Privacy in Cloud vs. On-Premise Deployments
Security and privacy are critical. Cloud-based platforms offer accessibility and scalability, but raise data breach concerns. On-premise deployments offer greater control over data security but may require investment in infrastructure and maintenance. Medical informaticists are increasingly addressing these concerns through encryption, access controls, and data governance frameworks.
The market for healthcare data annotation tools is growing rapidly. In 2023, the market was valued at USD 167.40 million. It's projected to reach USD 719.15 million by 2030, with a CAGR of 27.5%. This growth is driven by increasing AI adoption in healthcare and the demand for quality annotated datasets. Find more statistics here.

Practical Frameworks for Tool Selection
The best tool depends on various factors. The task complexity, team expertise, and project scale are key considerations. Simple bounding boxes might suffice for basic projects, while complex segmentation requires specialized tools. Teams with limited expertise might prefer user-friendly platforms. Expert annotators might want more flexibility and customization. Large projects benefit from platforms offering automation, collaboration features, and robust project management capabilities. Careful consideration of these elements ensures an informed decision and sets the stage for a successful project.
To help you navigate the options, we've compiled a comparison of some leading platforms:
The following table offers a comparison of several leading medical image annotation platforms:
Top Medical Image Annotation Platforms Comparison
A comprehensive comparison of leading medical image annotation platforms highlighting their key features, pricing, and specialized capabilities.
| Platform Name | Specialized Features | Supported Image Types | Pricing Model | Regulatory Compliance | User Rating |
|---|---|---|---|---|---|
| Labelbox | AI-assisted labeling, workflow automation, quality control features | DICOM, NIfTI, JPEG, PNG | Tiered subscription, enterprise options | HIPAA, GDPR | 4.5/5 |
| MD.ai | Collaboration tools, annotation review workflow, integration with PACS systems | DICOM, NIfTI, JPEG, PNG | Free tier, paid subscriptions for advanced features | HIPAA, GDPR | 4.2/5 |
| Encord | Active learning, automated quality assurance, SDK for custom integrations | DICOM, NIfTI, JPEG, PNG | Tiered subscription based on annotation volume | HIPAA, SOC 2 | 4.0/5 |
| SuperAnnotate | Project management tools, team collaboration features, advanced annotation tools for segmentation | DICOM, NIfTI, JPEG, PNG | Pay-as-you-go, custom enterprise plans | HIPAA, GDPR | 4.6/5 |
This table summarizes key information regarding several popular medical image annotation platforms, helping you begin your selection process. Be sure to research each platform further to determine the best fit for your needs.
Overcoming Critical Challenges in Medical Image Annotation
Medical image annotation plays a vital role in the advancement of AI in healthcare. However, it also presents a unique set of challenges that require careful attention and innovative solutions to ensure the creation of high-quality datasets. Let's explore some of these key challenges and how they are being addressed.
The Complexity of Medical Data
Medical data is inherently complex. Factors such as inconsistent image quality, variations in imaging protocols across different institutions, and the often subtle nature of various pathologies make accurate annotation a difficult task. For example, MRI images from different hospitals might have different contrast settings, hindering the development of a robust and generalizable AI model. To address this, teams are working on standardizing image acquisition protocols where possible and training annotators to recognize and account for these variations.
The Expert-Time Bottleneck
The expertise of radiologists is essential for accurate medical image annotation. However, their time is often limited, creating a bottleneck in the process. Innovative solutions are emerging to address this challenge. One approach involves using trained non-expert annotators to perform initial annotations, which are then reviewed and validated by radiologists. This tiered system maximizes efficiency while upholding the required quality standards. Another method utilizes AI-assisted annotation tools, like Labelbox, to pre-annotate images, significantly reducing the workload on human annotators.
Managing Inter-Annotator Disagreement
Even expert radiologists can have differing interpretations of subtle findings in medical images. This inter-annotator variability can significantly impact the quality of the training data. Successful projects mitigate this challenge through structured consensus-building workflows. For example, if there's disagreement among annotators on the boundaries of a lesion, a senior radiologist can review the annotations and make the final determination. This process helps ensure consistency and improves the overall reliability of the dataset.
Ethical and Regulatory Considerations
Medical data is subject to strict ethical and regulatory requirements, such as HIPAA, which governs patient health information. Protecting patient privacy is paramount when creating datasets for diagnostic innovation. Teams are implementing robust data anonymization procedures to safeguard patient information. This includes removing identifying information from images and implementing secure data storage and access protocols.
Building Scalable Annotation Workflows
The demand for annotated data is growing rapidly alongside the expansion of AI in healthcare. Building scalable annotation workflows is essential to meet this demand. This involves developing standardized annotation guidelines, implementing robust quality control processes, and leveraging technology to streamline the process. Cloud-based annotation platforms, like Amazon SageMaker Ground Truth, can facilitate collaboration and enhance efficiency. By tackling these challenges head-on and embracing innovative solutions, we can unlock the full potential of medical image annotation and pave the way for AI models that improve diagnostic accuracy and, ultimately, enhance patient care.
Capitalizing on Medical Image Annotation Market Growth
The medical image annotation market is expanding rapidly, creating exciting opportunities. This growth is fueled by the increasing use of AI in healthcare and the demand for accurately annotated datasets. Navigating this evolving market requires a strategic approach to business models, partnerships, and regional differences.
Business Models and Market Trends
Different business models are emerging in the medical image annotation market. Some companies provide comprehensive, full-service annotation solutions, managing the entire process. Others offer specialized services, focusing on particular image types like X-rays or MRIs. Still others concentrate on specific techniques such as polygonal segmentation or landmark annotation to meet niche requirements. Understanding these trends is crucial for success.
Integrating Annotation Services into the Healthcare AI Ecosystem
Medical image annotation is integral to the broader healthcare AI ecosystem. This integration fosters partnerships between technology providers and medical institutions. For example, annotation services can integrate with AI model development platforms, streamlining workflows for training and deploying AI diagnostic tools. These partnerships enable medical institutions to access annotation expertise while focusing on patient care.
Geographic Market Development and Regulatory Frameworks
Growth in the medical image annotation market varies geographically. Some regions experience faster growth due to factors like increased investment in healthcare technology and favorable regulations. Data privacy regulations, such as HIPAA in the US and GDPR in Europe, influence how annotation projects are managed. Understanding these regional nuances is essential for international expansion.
Investment Trends and Acquisition Activity
Investment in the medical image annotation sector is significant, accelerating market growth. Specialized annotation areas, such as those focusing on rare diseases or using advanced techniques, are attracting more funding. Larger healthcare technology companies are acquiring smaller annotation providers to strengthen their capabilities. This highlights the strategic value of medical image annotation within the broader healthcare landscape. Medical image annotation plays a key role in the healthcare data annotation market. The global data annotation market was valued at $629.5 million in 2021 and is projected to grow at a CAGR of 26.6% from 2022 to 2030. This growth underscores the increasing importance of data annotation in healthcare. Find more detailed statistics here. Annotated data improves the performance of AI diagnostic tools, crucial for developing effective treatments.
Positioning Your Organization for Success
Success in this complex market requires a focused strategy. Building a skilled team of annotators, using advanced annotation tools, and prioritizing quality control are essential. Adapting to the evolving needs of medical institutions and new technologies is critical for long-term success. By combining technical excellence with a deep understanding of the healthcare landscape, businesses can capitalize on the market's growth.
Building Successful Medical Image Annotation Projects

Building a successful medical image annotation project requires a structured approach. This includes building a skilled team, implementing thorough training, ensuring robust quality control, and understanding the inherent complexities of medical data. This section provides a practical framework for achieving these objectives.
Assembling Effective Annotation Teams
The foundation of any successful project lies in its team. Leading healthcare organizations prioritize assembling teams with a diverse range of expertise. This often involves a combination of experienced medical professionals, such as radiologists or pathologists, for quality control, and trained annotators to handle the detailed labeling tasks. This combination maximizes efficiency and ensures accuracy.
For example, a project focused on annotating cardiac MRI images would ideally include a cardiologist to oversee the annotation process and trained annotators to precisely delineate the heart's structures.
Developing Comprehensive Training Protocols
Thorough training is crucial for generating high-quality annotations. Comprehensive training programs should familiarize annotators with the specific annotation tools being used, the project's guidelines, and the intricacies of medical image interpretation. This approach minimizes variability among annotators and ensures dataset consistency. Regular refresher training sessions can also address evolving project requirements or new diagnostic criteria.
Establishing Quality Assurance Workflows
Maintaining diagnostic accuracy necessitates rigorous quality assurance. Successful projects implement multi-layered quality control. This could involve an initial review by senior annotators, followed by validation from expert radiologists or pathologists. This layered approach minimizes errors and ensures data reliability. Tools that facilitate collaboration and streamlined review, revision, and feedback processes are crucial for efficient quality control.
Creating Effective Annotation Guidelines
Clear and comprehensive annotation guidelines are the backbone of consistent results. These guidelines should meticulously detail specific annotation criteria, clearly outlining how different anatomical structures or pathologies should be marked and labeled. They act as a consistent reference point for all annotators, reducing ambiguity and promoting uniform interpretation across the entire team. These guidelines should be regularly reviewed and updated to reflect current best practices and evolving project needs.
Handling Edge Cases and Rare Conditions
Medical image annotation frequently presents challenges related to unusual or rare medical conditions. Effective approaches to these scenarios often involve leveraging the expertise of specialized medical professionals. For instance, a particularly challenging case might require consultation with a sub-specialist to ensure the accurate identification and annotation of a rare anatomical variant. This collaborative approach ensures data accuracy, even in complex situations.
Realistic Timelines, Budget Considerations, and ROI
Medical image annotation projects demand realistic planning regarding timelines and budgets. Effective resource allocation strategies should consider the complexity of the annotation task, the desired level of quality, and the project's overall scope. The return on investment (ROI) in medical AI is measured by improved patient outcomes. This requires carefully tracking the impact of the annotated data on diagnostic accuracy and treatment efficacy. Accurate timelines and budgets contribute significantly to a project's overall success. This ensures the efficient use of resources and maximizes the potential for positive patient impact. By adhering to these practices and adapting to evolving needs, organizations can build medical image annotation projects that generate high-quality data, accelerate AI development, and contribute to more effective healthcare solutions.
The Future of Medical Image Annotation
Medical image annotation is constantly evolving, fueled by advancements in artificial intelligence (AI) and a growing need for high-quality medical datasets. This evolution promises to further enhance AI's capabilities in healthcare, leading to more accurate diagnoses and better patient outcomes.
Active Learning and Federated Approaches
Active learning is transforming how we annotate images. Traditional methods often require annotating every single image, a process that is both time-consuming and expensive. Active learning algorithms cleverly select the most informative images for annotation, significantly reducing the workload while maximizing the value of the annotated data. This focused approach optimizes resource use and speeds up the training process.
Federated learning addresses important privacy concerns. It allows multiple institutions to collaborate on training a shared AI model without directly exchanging sensitive data. Each institution trains the model locally, using its own data, and only the model's parameters are shared. This protects patient privacy while enabling the development of more robust and generalizable AI models, a critical benefit in medical settings with strict regulations like HIPAA.
Continuous Learning Systems and the Blurring of Clinical Workflows
Continuous learning systems are pushing the boundaries of medical image annotation. These systems constantly learn and adapt as new data becomes available, blurring the lines between the annotation process and clinical workflows. Imagine an AI system assisting radiologists with image interpretation while simultaneously learning from their feedback. This creates a cycle of continuous improvement, benefiting both the AI's performance and the radiologist's diagnostic abilities.
Synthetic Data Generation and Transfer Learning
Synthetic data generation holds immense potential. Creating artificial medical images can augment existing datasets and address the challenge of data scarcity, particularly for rare diseases. However, limitations in generating realistic synthetic data currently necessitate careful validation and quality control to ensure reliable results.
Transfer learning offers a valuable complementary approach. By using pre-trained models, like those trained on ImageNet, and fine-tuning them for specific medical image annotation tasks, we can reduce the need for extensive annotation from scratch. This approach accelerates development and improves efficiency, especially when working with limited datasets.
Multimodal Integration: Challenges and Opportunities
The future of medical image annotation is undeniably multimodal. Integrating imaging data with genomic and clinical data presents exciting new possibilities for personalized medicine. However, this integration also introduces new challenges. Combining diverse data types requires standardized formats and reliable data fusion methods. Forward-thinking organizations are actively developing strategies to address these complexities. Multimodal integration promises more precise and personalized diagnostic tools that consider a patient's complete medical history, leading to improved treatment decisions and better patient care.
Looking for a partner in medical image annotation? PYCAD offers comprehensive AI solutions for medical imaging, from data handling and model training to deployment. Explore how PYCAD can help your organization.






