The Evolution of Medical Image Processing: From Pixels to Precision
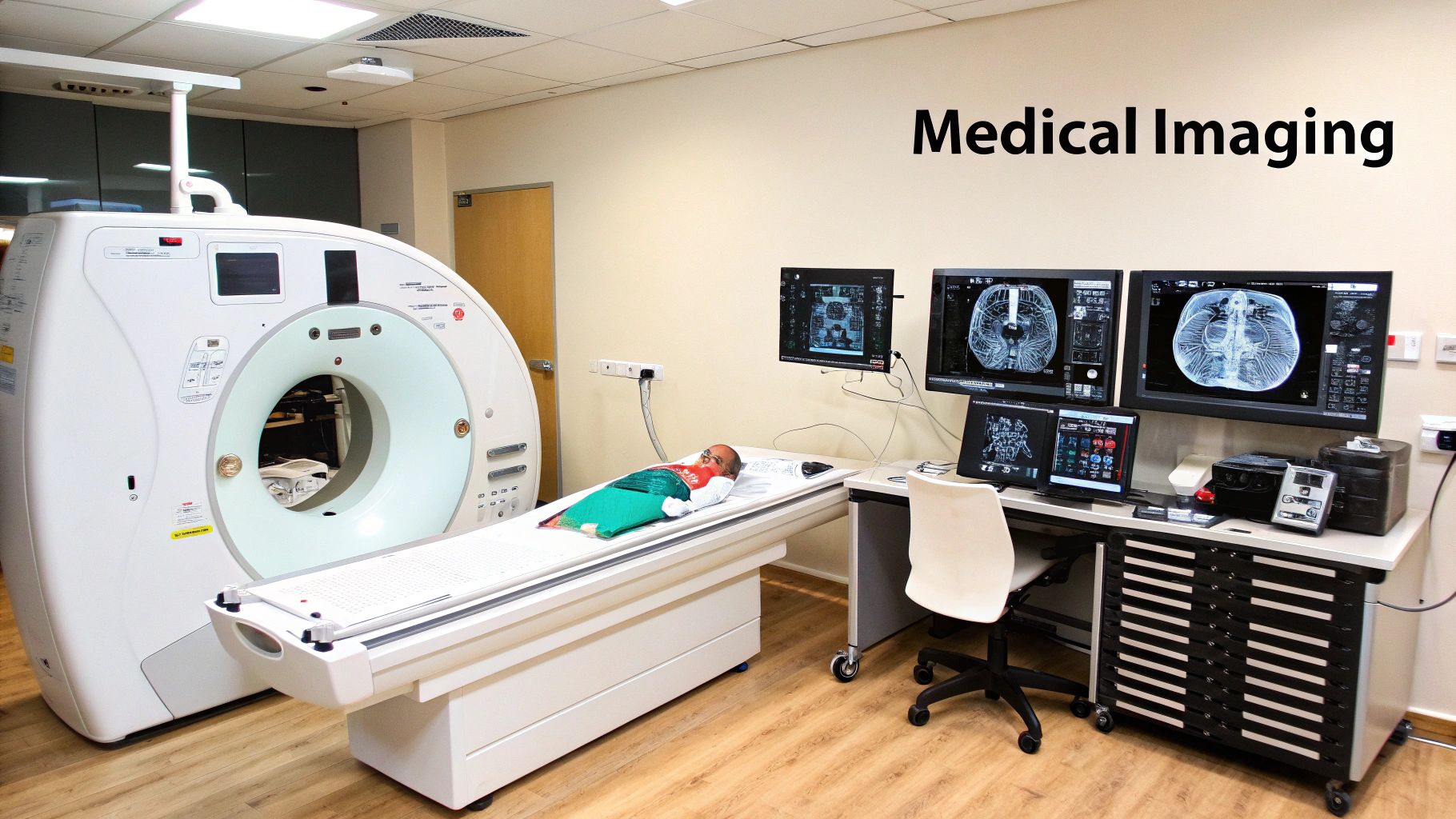
Medical image processing has dramatically changed how we diagnose and treat illnesses. What began with basic film processing now involves complex computational analysis, revealing insights previously impossible to see. This represents a significant advancement in healthcare technology. Early X-rays offered a static view inside the body. The arrival of digital imaging, however, opened up the possibility of computational manipulation and analysis – the true beginning of medical image processing.
This progress wasn't a sudden revolution but a series of steps forward by researchers and innovators. Medical image processing has a long history connected to the very beginnings of medical imaging itself. The SPIE Medical Imaging conference series, for example, has played a crucial role since 1971. Early conferences, like the one on ‘Quantitative Imagery in the Biomedical Sciences,’ laid the foundation for future developments in image processing.
By the 1990s, the field focused on interpreting medical images using techniques like registration, segmentation, classification, and reliable measurements. This evolution led to significant progress, marked by a rise in publications on these techniques. For example, publications related to segmentation jumped from 64 between 1981-1990 to 1191 between 2011-2021. This highlights the increasing importance of image processing in medical diagnostics. As technology continues to progress, integrating these techniques into clinical workflows is vital for better patient outcomes. You can find more detailed statistics here: https://pmc.ncbi.nlm.nih.gov/articles/PMC9400549/
Early Challenges and Breakthroughs
Early innovators faced significant hurdles due to limited computing power and storage. Imagine analyzing a detailed 3D image on a computer much less powerful than a modern smartphone. This constraint meant algorithms needed to be incredibly efficient to extract useful information. Processing times could be lengthy, sometimes delaying diagnoses and treatment decisions. This challenge encouraged research into faster, more effective algorithms.
From Academic Curiosity to Clinical Necessity
Initially, many viewed medical image processing as a purely academic pursuit. However, as computing power grew and algorithms advanced, its clinical value became clear. Veteran radiologists and biomedical engineers witnessed this firsthand. They saw these technologies transition from research projects into essential daily tools. This shift was driven by the clear benefits of medical image processing, enabling more precise diagnoses, earlier disease detection, and improved treatment planning.
The Rise of 3D Imaging and Beyond
The arrival of 3D imaging techniques like CT and MRI presented new challenges and opportunities. Instead of analyzing single 2D images, algorithms now had to handle large volumes of data. This spurred the development of new methods for visualizing, analyzing, and interpreting 3D images. The increase in data also drove the creation of more advanced algorithms for efficient information management and processing. The field continues to evolve, with new research and technologies constantly expanding possibilities. This ongoing progress promises even more precise and personalized healthcare for the future.
Core Techniques Reshaping Medical Diagnosis

Understanding medical documentation guidelines provides valuable context when exploring core medical imaging techniques. Medical image processing transforms raw data from various imaging modalities into visually insightful representations. These visualizations empower medical professionals to make more informed diagnostic decisions. These techniques are fundamental to modern medical diagnosis, contributing significantly to more accurate and efficient patient care.
Image Enhancement: Unveiling Hidden Details
Image enhancement techniques improve the visual quality of medical images. They achieve this by highlighting key features and suppressing unwanted noise. This process is similar to adjusting the contrast and brightness settings on a television screen for a clearer picture.
Histogram equalization, for instance, redistributes pixel intensity values. This makes subtle differences in tissue density more visible. This is particularly helpful in X-rays and CT scans for improved visualization of bone and soft tissue.
Noise reduction filters smooth out image graininess, improving the clarity of fine details. This clarity is crucial for identifying small lesions or other abnormalities, increasing diagnostic confidence.
Image Segmentation: Defining Anatomical Structures
Image segmentation isolates specific anatomical structures within a medical image. It's like outlining different objects in a drawing to understand their individual shapes and sizes. This technique facilitates precise measurements and detailed analysis of targeted organs or tissues.
Segmenting the heart in an MRI image, for example, allows cardiologists to accurately assess its volume, wall thickness, and ejection fraction. This is vital for diagnosing heart conditions and planning appropriate treatment strategies. Similarly, in oncology, segmenting tumors helps determine their size, shape, and location, which is crucial for cancer staging and monitoring treatment response.
Image Registration: Aligning Multiple Perspectives
Image registration aligns multiple images of the same anatomical area. These images might be taken at different times or using different imaging modalities. The process resembles overlaying two slightly different maps of the same region to understand how they correspond.
This creates a combined view that incorporates information from each image. Registering a CT scan with an MRI scan, for instance, allows doctors to simultaneously visualize both bone structure and soft tissue details. This comprehensive perspective enhances diagnostic accuracy, especially in complex cases where information from a single modality may be insufficient.
This combined view is invaluable for surgical planning and image-guided interventions, enabling greater precision. Moreover, image registration tracks changes over time, such as tumor growth or tissue healing, facilitating more effective monitoring of treatment effectiveness.
To further clarify these techniques, let's examine their applications, strengths, and limitations.
Introducing the following table to compare key medical image processing techniques:
Comparison of Key Medical Image Processing Techniques
This table compares the primary image processing techniques used in medical diagnostics, highlighting their applications, strengths, and limitations.
| Technique | Primary Applications | Key Strengths | Limitations | Typical Imaging Modalities |
|---|---|---|---|---|
| Image Enhancement | Improving visibility of features, noise reduction | Enhances image quality, aids in feature detection | May introduce artifacts, can alter original data | X-ray, CT, MRI, Ultrasound |
| Image Segmentation | Isolating anatomical structures, quantifying tissue properties | Enables precise measurements, facilitates analysis of specific regions | Can be challenging for complex structures, requires robust algorithms | MRI, CT, Ultrasound |
| Image Registration | Combining information from multiple images, tracking changes over time | Improves diagnostic accuracy, facilitates surgical planning | Requires accurate alignment, computationally intensive | CT, MRI, PET |
This table highlights the distinct roles and capabilities of each technique. While image enhancement focuses on improving overall image quality, segmentation isolates specific structures, and registration combines information from multiple images. Each technique contributes uniquely to the diagnostic process.
By understanding these core techniques, we can appreciate the power of medical image processing in transforming raw data into actionable insights for improved patient care.
Multi-Modality Imaging: Where Diverse Data Meets Definitive Diagnosis

Medical image processing has come a long way. We've moved beyond analyzing single images to integrating data from multiple sources. This multi-modality imaging approach combines the strengths of different imaging techniques, like fitting together pieces of a puzzle, to create a more complete picture of a patient's health. This fusion of data leads to more accurate diagnoses and better treatment planning.
Combining Strengths, Overcoming Limitations
Each imaging method has its unique advantages and disadvantages. Computed Tomography (CT) is excellent for visualizing bone structure. Magnetic Resonance Imaging (MRI), on the other hand, provides detailed soft tissue images. Positron Emission Tomography (PET) reveals metabolic activity, while Single-Photon Emission Computed Tomography (SPECT) maps blood flow and other crucial physiological processes.
Multi-modality imaging, such as combining PET with CT (PET-CT), PET with MRI (PET-MRI), or SPECT with CT (SPECT-CT), overcomes these individual limitations. Consider PET-CT, which merges the metabolic insights from PET with the precise anatomical detail of CT. This allows doctors to pinpoint the exact location of metabolically active areas, such as tumors. This combined approach dramatically increases diagnostic accuracy in fields like oncology, neurology, and cardiology.
Computational Challenges and Advanced Algorithms
Integrating data from multiple imaging modalities presents complex computational hurdles. These diverse datasets need to be carefully aligned and processed to generate clear, cohesive visualizations. Think of it like trying to perfectly overlay two semi-transparent images, each revealing a different aspect of the same object. This intricate process requires advanced algorithms to account for differences in image resolution, acquisition parameters, and patient positioning. These sophisticated algorithms are essential for ensuring accurate data fusion and preventing misinterpretations.
These algorithms are designed to uncover subtle disease characteristics that might otherwise remain hidden. This is achieved by combining structural and functional information, providing a more holistic view of the underlying disease process. For example, in neurology, combining MRI with fMRI (functional MRI) can identify the specific brain regions associated with particular cognitive functions, aiding in the diagnosis of neurological disorders.
Additionally, the increasing complexity of medical image processing has driven researchers to explore cutting-edge methods and technologies. The use of advanced computational methods, including multi-modality imaging, model-based image analysis, and virtual reality integration, is rapidly expanding. Learn more about these exciting developments in medical image processing here.
Real-World Clinical Applications
Multi-modality imaging has already significantly improved diagnostic accuracy and patient outcomes. In oncology, PET-CT assists in cancer staging, guiding biopsies, and evaluating treatment response. In cardiology, SPECT-CT helps assess blood flow to the heart, pinpointing areas with reduced perfusion. This is crucial for diagnosing and managing various heart conditions. In neurology, PET-MRI enhances the detection of brain tumors and neurodegenerative diseases. These real-world applications are revolutionizing clinical practice across numerous medical specialties. Ongoing research into new imaging techniques and algorithms promises even further advancements in medical image processing and its profound impact on patient care.
AI Revolution in Medical Image Analysis: Beyond Human Vision

Artificial intelligence (AI) is rapidly transforming medical image processing. This technology surpasses human visual capabilities, identifying subtle patterns and anomalies often undetectable by the naked eye. This is particularly important for early disease detection and diagnosis.
The Power of Deep Learning Algorithms
Deep learning algorithms, a subset of AI, are driving this progress. Modeled after the human brain, these algorithms analyze vast amounts of data to identify complex patterns. They offer exceptional accuracy in tasks such as early cancer detection, predicting disease progression, and quantifying minute anatomical changes.
Convolutional Neural Networks (CNNs) are especially adept at image processing. These networks are ideally suited for medical image analysis because they learn hierarchical representations of image features. They identify basic patterns, such as edges and textures, in early layers, combining them to recognize complex structures like organs and lesions in subsequent layers.
Adapting AI For Diverse Clinical Needs
CNNs are not a universal solution. Researchers are adapting these algorithms to address the unique requirements of different imaging modalities. They are tailoring CNN architectures to work with a variety of imaging methods, including X-rays, CT scans, MRI, and ultrasound images. This ensures the algorithms can extract meaningful information from various imaging techniques.
This adaptability improves diagnostic abilities across diverse clinical applications. From characterizing tumors in oncology to assessing cardiac function in cardiology, AI is proving invaluable. AI-powered systems are being tested in real-world clinical settings, showcasing their potential for seamless integration into current healthcare workflows.
AI Augmenting Human Expertise
Critically, this AI revolution augments, not replaces, the expertise of radiologists and other medical professionals. AI algorithms rapidly process large datasets, highlighting potential issues for review by a human expert. This speeds up diagnoses and allows professionals to focus on critical areas. This collaboration ensures both efficiency and accuracy. The market for medical image analysis is rapidly expanding, driven by these advancements. Learn more about this field at Medical Image Computing. Projections estimate a CAGR of 7.8% by 2029, with AI and machine learning playing a central role in this growth.
Case Studies and Future Directions
The impact of AI in medical image processing is visible in case studies across multiple specialties, from pathology and radiology to cardiology, where AI is improving diagnostic accuracy. Early intervention facilitated by AI also has the potential to lower healthcare costs by improving treatment strategies, leading to more targeted interventions and reducing unnecessary procedures. This promises to improve patient outcomes and overall healthcare system efficiency.
The following table provides further insights into the applications of AI in medical imaging:
AI Applications in Medical Image Processing: This table presents key applications of artificial intelligence in various medical imaging specialties, including the specific technologies used and their clinical impact.
| Medical Specialty | AI Technology | Clinical Application | Reported Accuracy | Implementation Status |
|---|---|---|---|---|
| Radiology | CNNs | Lung nodule detection in CT scans | >95% | Clinical trials and initial deployment |
| Pathology | Deep learning | Cancer diagnosis in tissue biopsies | Varies, but comparable to or exceeding human pathologists | Research and development, some clinical use |
| Cardiology | CNNs, RNNs | Cardiac function assessment from echocardiograms | >90% for certain metrics | Research and clinical trials |
| Ophthalmology | Deep learning | Diabetic retinopathy detection in retinal images | >90% | Clinical use in some areas |
| Neurology | CNNs | Brain tumor segmentation in MRI scans | High accuracy, enabling better treatment planning | Research and clinical trials |
This table demonstrates the varied applications of AI across medical specialties, with reported accuracy often exceeding or matching human capabilities. While implementation stages vary, the potential for widespread clinical use is clear, promising improved diagnostic accuracy and patient care.
Real-World Clinical Impact: Where Processing Meets Patient Care
Medical image processing is more than just technological progress; it's reshaping patient care. These technologies directly influence patient outcomes across various medical specialties, creating more effective and efficient healthcare systems.
Earlier and More Accurate Diagnoses
One of the most significant impacts is the ability to diagnose diseases earlier. In oncology, medical image processing aids in identifying cancerous growths at earlier stages, sometimes even before they're visible to the naked eye. This early detection is critical for effective treatment and substantially improves a patient's chances of survival. Advanced AI can also analyze medical images stored within PDFs. Sophisticated algorithms can detect minute changes in tissue density in lung scans, allowing for earlier detection of lung cancer, even when the nodules are incredibly small.
In cardiology, medical image processing allows for more precise cardiac assessments. By analyzing images of the heart, physicians can accurately measure heart function, identify arterial blockages, and detect other heart abnormalities. This detailed analysis informs treatment decisions, helping prevent serious cardiac events.
Stroke diagnosis has also seen significant improvement. Medical image processing enables faster identification of stroke-affected areas in the brain. This rapid diagnosis is crucial for timely intervention, minimizing brain damage, and maximizing the patient's chances of recovery. Quickly analyzing brain scans allows doctors to pinpoint the affected regions and administer appropriate treatments, significantly reducing the risk of long-term disability.
Targeted Interventions and Improved Treatment Planning
Beyond diagnosis, medical image processing enhances treatment planning. In orthopedics, processed images facilitate better surgical planning by providing surgeons with precise 3D models of bones and joints. This allows for more accurate pre-operative planning, leading to less invasive surgeries and faster recovery times. Surgeons can use these models to simulate procedures and determine the optimal approach, minimizing the risk of complications.
Medical image processing has also contributed to a reduction in unnecessary procedures. By providing detailed and accurate information, it helps avoid exploratory surgeries or other invasive tests previously performed due to diagnostic uncertainty. This not only reduces healthcare costs but also minimizes patient discomfort and risk.
Transforming Workflows and Patient Experiences
Medical image processing is not only improving clinical outcomes but also transforming the way radiologists and clinicians work. These tools are being integrated into daily workflows, enabling more confident decisions and more effective communication of findings to patients. Furthermore, they reduce the time spent on tedious manual tasks. This enhanced efficiency improves diagnostic accuracy and allows medical professionals to dedicate more time to direct patient care.
This integration directly improves patient experiences. Shorter diagnostic timelines mean patients receive answers faster and can begin treatment sooner. More targeted interventions result in less invasive procedures, leading to faster recovery and reduced pain. By streamlining the healthcare process, medical image processing reduces patient stress and improves their overall experience. Case studies from leading medical centers have demonstrated substantial improvements in diagnostic accuracy, treatment success rates, and operational efficiency. These quantifiable benefits highlight the transformative potential of medical image processing in providing high-quality patient care.
Future Frontiers: Breaking Barriers in Medical Image Processing
Medical image processing has seen remarkable advancements. However, several challenges still need to be addressed before its full potential can be realized. These include persistent technical hurdles and non-technical barriers that hinder wider clinical adoption. Thankfully, exciting innovations are on the horizon, promising to reshape the future of this field.
Technical Hurdles on the Path to Progress
One significant challenge is developing robust algorithms that perform consistently across diverse patient populations. Just as human populations vary in physical characteristics, so do medical images. This diversity can influence algorithm performance, making it crucial to develop algorithms capable of effectively analyzing images from various groups. For example, an algorithm trained mainly on images from one ethnic group might not be as accurate when analyzing images from another. Addressing these variations is essential for building reliable and equitable medical image processing tools.
Another hurdle is standardizing image quality across different imaging equipment. Variations in equipment and settings can introduce inconsistencies into medical images, much like comparing photographs taken with different cameras under different lighting conditions. These inconsistencies can complicate the analysis and comparison of images across healthcare facilities. Establishing standardized protocols and image acquisition parameters can help mitigate this challenge and ensure consistency.
Finally, the computational demands of real-time processing present a significant obstacle. Advanced medical image processing techniques often require substantial computing power, which can be expensive and time-consuming. This is especially challenging for real-time applications, such as image-guided surgery, where rapid processing is essential. Developing more efficient algorithms and exploring new computing paradigms, such as quantum computing, offer potential solutions to these limitations.
Non-Technical Barriers to Wider Adoption
Beyond technical challenges, non-technical factors can also impede the implementation of medical image processing technologies in clinical settings. These include regulatory approvals, ethical considerations, and clinical workflow integration. Working with regulatory agencies to ensure compliance with safety and efficacy standards is crucial. Open discussions about ethical implications, particularly regarding data privacy and algorithmic bias, are also essential. Finally, seamlessly integrating these new tools into existing clinical workflows is critical, requiring careful consideration of user interfaces, training, and data management systems.
Emerging Technologies Reshaping the Future
Despite these challenges, several exciting innovations promise to transform the future of medical image processing. Federated learning, for example, addresses data privacy concerns. This approach allows algorithms to learn from decentralized datasets without directly sharing sensitive patient information. Think of it like multiple chefs perfecting parts of a recipe without revealing their full ingredient lists. Each chef contributes expertise to improve the overall dish while keeping individual recipes secret.
Explainable AI (XAI) is another promising area. XAI aims to create transparent AI systems that provide insights into their decision-making processes. This transparency is vital for building trust and confidence in medical diagnoses, especially in critical situations, by allowing physicians to understand the reasoning behind an AI's diagnosis.
Quantum computing may also revolutionize medical image processing. Though still in its early stages, its potential to dramatically accelerate processing speeds could unlock new possibilities for analyzing complex image data. This increased computing power could lead to faster and more accurate diagnoses, paving the way for personalized medicine and improved patient care.
A Vision for the Future of Medical Image Processing
Industry leaders envision a future where sophisticated image processing becomes integral to routine clinical care, democratizing access to expert-level diagnostic capabilities, even in resource-limited settings. Imagine a world where anyone, regardless of location, has access to the same level of diagnostic expertise through AI-powered medical image analysis. This future is not only technologically exciting, but also holds the potential for a more equitable and accessible healthcare system.
Ready to unlock the full potential of your medical images? PYCAD offers comprehensive AI solutions for medical imaging, from data handling and model training to deployment. Visit PYCAD today to learn more.






