Segmentation Advances in Medical Imaging: A Closer Look
Medical imaging plays a vital role in modern healthcare, helping doctors understand what’s happening inside their patients’ bodies. However, raw data from scans like CT, MRI, and ultrasound can be complex to analyze effectively. This is where image segmentation makes a critical difference by converting raw scans into clear, usable information. By identifying and isolating specific areas of interest – such as organs, tumors, or lesions – segmentation helps medical professionals make more accurate diagnoses, create precise treatment plans, and guide surgical procedures in real-time.
The field has come a long way from its early days of manual tracing. Today’s advanced computing and artificial intelligence capabilities have transformed what was once a slow, manual process into a largely automated and highly accurate system. Modern segmentation methods carefully balance three key factors: accuracy, speed, and reliability. This allows for consistent results across many different types of medical images and patient cases.
This article examines eight fundamental techniques used in medical image segmentation, from basic approaches to the latest developments in deep learning. We’ll explore how each method works, look at their pros and cons, and see how they’re used in real medical settings. Whether you work in medical device development, research AI applications in healthcare, or manage medical imaging systems, understanding these core segmentation approaches will give you valuable insights into this essential technology. Our goal is to help you grasp both the current capabilities and future potential of medical image segmentation.
Key Concepts We’ll Cover:
- Traditional vs AI-based segmentation methods
- Essential technical principles and workflows
- Real-world applications and case studies
- Strengths and limitations of different approaches
- Future developments and opportunities
1. Thresholding-Based Segmentation
Thresholding-based segmentation is a key technique for analyzing medical images. This method divides images into distinct regions by setting pixel intensity thresholds. The process creates either binary segmentation (two segments) or multi-level segmentation (multiple segments) based on whether pixels fall above or below defined threshold values.

How it Works
The main goal is finding the right threshold value to separate objects from background. This can be done through several methods:
- Global Thresholding: Uses one threshold across the entire image, working best when objects and background have clear intensity differences
- Local Thresholding: Calculates different thresholds for image regions to handle varying lighting and contrast
- Otsu’s Method: An automated approach that finds optimal thresholds by analyzing pixel intensity distributions
Features and Benefits
- Choice of global or local thresholding approaches
- Automated threshold selection with Otsu’s method
- Works well with standard grayscale medical images
- Can segment multiple distinct regions
- Fast processing speed for real-time use
- Simple implementation and integration
- Reliable results for high-contrast images
Advantages and Limitations
Benefits:
- Quick processing suitable for real-time applications
- Easy to understand and implement
- Works very well on high-contrast images
Limitations:
- Results affected by image noise and intensity changes
- May not handle complex anatomical structures well
- Less effective for low-contrast images
- Often needs manual threshold adjustment
Real-World Medical Applications
- Finding bone fractures and measuring density in X-rays
- Marking tumor boundaries in brain MRI scans
- Detecting and measuring lung nodules in CT images
Implementation Tips
- Study image histograms to identify good threshold values
- Use adaptive thresholding for uneven lighting
- Apply noise reduction filters before segmentation
- Have medical experts verify segmentation accuracy
Historical Development
The field advanced significantly in 1979 when Nobuyuki Otsu created his automated thresholding method. This provided an objective way to find optimal thresholds, leading to wider use of thresholding techniques in medical imaging.
Enduring Value
Despite its limitations, thresholding remains valuable due to its simplicity and speed. It serves as a foundation for more advanced segmentation and provides quick initial results that can be refined further. Its efficiency makes it especially useful in time-sensitive and resource-limited settings.
2. Deep Learning-Based Segmentation (CNNs)
Medical image segmentation has been fundamentally improved by Convolutional Neural Networks (CNNs) and deep learning approaches. These methods automatically detect important image features, allowing precise identification of anatomical structures, lesions, and other areas of interest. Due to their accuracy and automation capabilities, CNNs have become essential tools in medical imaging for diagnosis, treatment planning, and research.
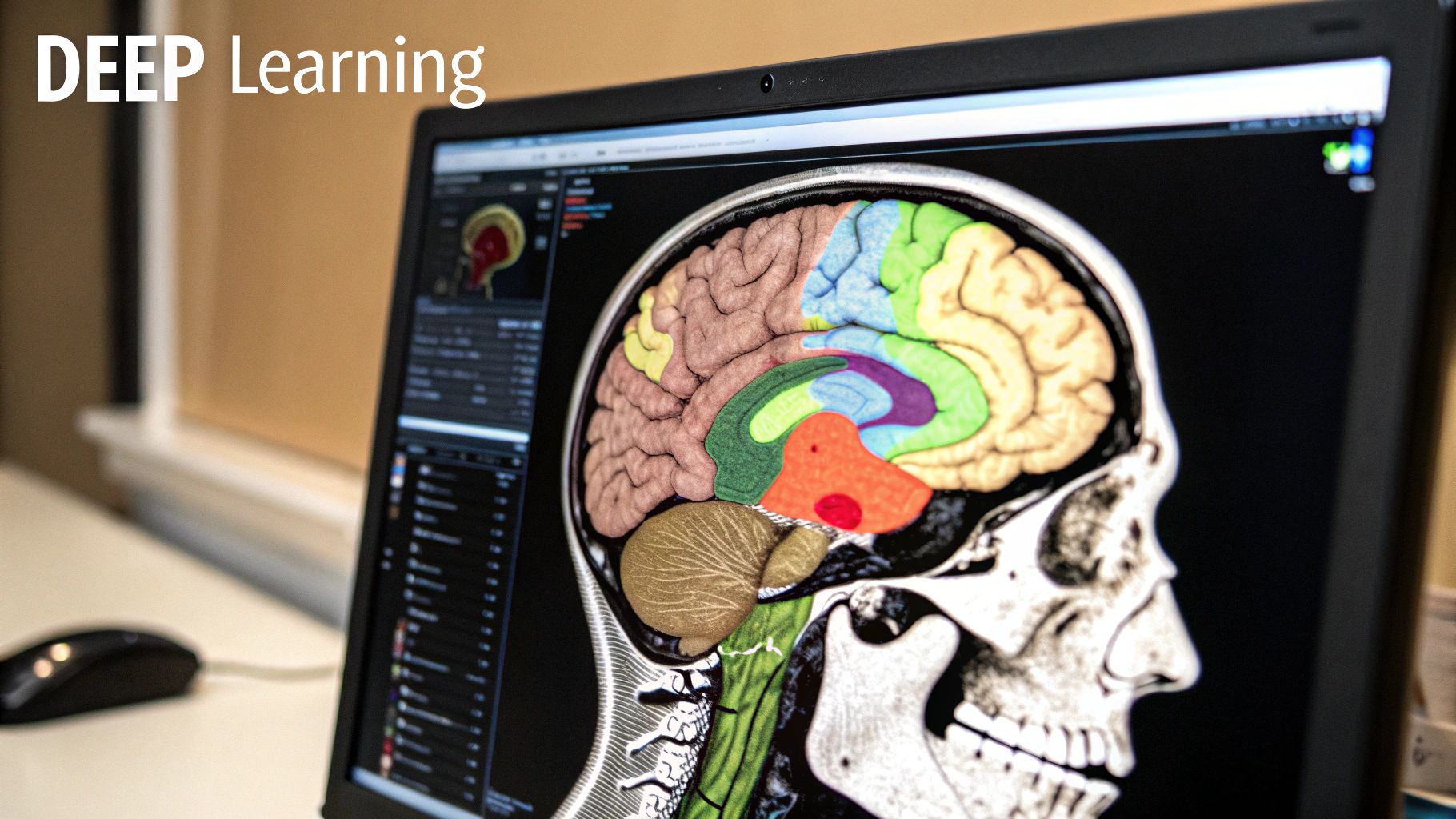
How CNNs Segment Medical Images
CNNs work by processing images through multiple layers that learn increasingly complex features. The initial layers identify basic elements like edges and textures, while deeper layers recognize more abstract patterns specific to the segmentation task. This multi-level approach enables better understanding of image context and improved accuracy. The U-Net architecture, developed by Olaf Ronneberger, has proven particularly effective for medical image segmentation through its ability to capture both fine details and broader structural information.
Key Features and Benefits
- End-to-end learning: CNNs learn directly from image data without manual feature engineering
- Hierarchical feature extraction: Analysis at multiple scales enables comprehensive image understanding
- Multiple architecture options: Various CNN designs like U-Net and Mask R-CNN suit different segmentation needs
- Transfer learning capability: Using pre-trained models reduces training requirements
Real-World Examples and Case Studies
- Brain tumor segmentation: CNNs accurately identify and outline brain tumors in MRI scans to assist diagnosis and treatment monitoring
- Organ segmentation: Precise mapping of organs in CT scans enables automated measurements and surgical planning
- Retinal vessel analysis: CNN-based segmentation of retinal blood vessels helps diagnose conditions like diabetic retinopathy
Pros and Cons
Pros:
- High accuracy and reliability
- Handles complex patterns effectively
- Automatic feature detection
- Good generalization with sufficient data
Cons:
- Needs large training datasets
- Resource-intensive computing requirements
- Limited interpretability
- Training can be time-consuming
Practical Implementation Tips
- Data augmentation: Expand training data through image transformations like rotation and scaling
- Use pre-trained models: Start with existing models to reduce development time
- Validate thoroughly: Test generalization using cross-validation
- Plan computing resources: Ensure adequate GPU processing power for model training
Deep learning segmentation has become invaluable for medical image analysis, driving improvements in healthcare delivery. While data and computing demands present challenges, ongoing advances in architectures and training methods continue enhancing this technology’s capabilities. For medical technology companies and research institutions, CNN-based segmentation enables significant advances in diagnostic accuracy and patient care.
3. Region Growing Segmentation
Region growing segmentation is a method of analyzing medical images that identifies distinct areas based on similar properties. This technique starts from specific points and expands outward to find connected regions with shared characteristics, making it useful for medical applications that need precise identification of anatomical structures.
The process begins with user-selected “seed points” placed within the target area. From these seeds, the algorithm examines neighboring pixels and adds those that match predefined criteria to the region. This process repeats until it reaches boundaries or meets stopping conditions.
Key Features and Functionality:
- Seed Point Selection: Success depends heavily on choosing good starting points that represent the target region’s typical properties
- Similarity Criteria: Rules that determine which nearby pixels join the region, often based on intensity levels or texture patterns
- Region Merging: Methods for combining multiple growing regions that share common features
- User Control: Most implementations allow adjusting parameters and seed placement during the process
Comparison of Benefits and Limitations:
| Advantages | Disadvantages |
|---|---|
| Works well with uniform regions | Results depend on seed placement |
| Creates connected areas | May spread into nearby regions |
| Can use multiple criteria | Processing can be slow for large images |
| Effective with clear edges | Sensitive to parameter changes |
Real-World Medical Applications:
- Liver Tumor Analysis: Helps surgeons plan procedures by marking tumor boundaries and distinguishing healthy tissue
- Heart Chamber Measurement: Maps heart chambers in MRI and CT scans to assess heart function
- Breast Cancer Screening: Assists in finding and measuring suspicious areas in mammograms
Implementation Guidelines:
- Strategic Seed Placement: Take time to position seeds accurately – complex structures may need multiple starting points
- Clear Stopping Rules: Set firm boundaries using intensity changes, texture shifts, or statistical measures
- Combined Methods: Mix region growing with other techniques like edge detection for better results
- Testing and Verification: Compare results against known data to optimize settings for each specific use
Region growing remains a key tool in medical image analysis because it handles uniform regions well and offers direct user control. While results depend on careful setup and parameter choice, its straightforward approach and flexibility make it valuable when used appropriately and with an understanding of its limitations.
4. Active Contour Models (Snakes)
Active Contour Models, commonly called “snakes,” are advanced tools for medical image segmentation that excel at finding complex anatomical boundaries. These models work by evolving a flexible contour that moves toward object edges, guided by internal forces that control smoothness and external forces derived from image features like edges and gradients.

The method stands out for handling intricate shapes, resisting noise, and creating smooth boundaries. Its energy minimization framework allows incorporation of prior shape knowledge, improving accuracy. Users can also guide the process through interactive initialization, while topology preservation ensures structural consistency.
Key Features:
- Energy Framework: Optimizes boundary detection using balanced internal and external forces
- Flexible Representation: Supports both parametric and geometric approaches
- User Interaction: Allows manual guidance for complex cases
- Shape Preservation: Maintains structural integrity during processing
- Clean Results: Produces smooth, well-defined boundaries
Advantages:
- Complex Shape Handling: Effectively segments intricate anatomical structures
- Noise Resistance: Maintains accuracy even in noisy medical images
- Smooth Output: Creates clear, analytically useful boundaries
- Prior Knowledge: Integrates anatomical shape information
Limitations:
- Initial Placement: Requires careful positioning of starting contour
- Optimization Issues: Can settle for suboptimal solutions
- Parameter Settings: Needs precise tuning for best results
- Processing Load: Demanding on computational resources
Clinical Applications:
- Heart Analysis: Segmenting ventricles in cardiac imaging
- Cell Studies: Identifying individual cells in microscopy
- Vascular Imaging: Mapping blood vessels in angiograms
History and Development:
First introduced by Kass, Witkin and Terzopoulos in 1988, snakes have seen major advances in energy functions, optimization methods, and integration with other techniques. This ongoing refinement has established them as essential tools in medical imaging.
Implementation Guidelines:
- Start Position: Use automated methods or anatomical landmarks for initialization
- Force Balancing: Carefully adjust internal and external force weights
- Consider GVF: Add Gradient Vector Flow fields to improve range
- Multi-Scale: Process at different resolutions for better results
Active Contour Models continue to play a vital role in medical image analysis. Understanding their capabilities and proper implementation allows researchers to effectively use this technique for complex segmentation tasks.
5. Atlas-Based Segmentation
Atlas-based segmentation is a powerful medical image analysis method that uses pre-labeled images (atlases) to segment structures in new images. This technique provides an anatomically-informed approach to identifying organs, tissues, and regions of interest in medical imaging.
How it Works:
The main concept involves matching atlas images to the target image through spatial alignment of anatomical structures. After alignment, labels from the atlas transfer to the target image to segment the desired areas. The process involves these key steps:
- Reference Atlas Creation: Start with high-quality, manually segmented images. These can be from single subjects or multiple subjects to account for anatomical differences.
- Registration Algorithms: Use methods like affine transformations and deformable registration to align the atlas with target images. Algorithm choice depends on anatomical complexity.
- Label Fusion Methods: For multi-atlas approaches, combine transferred labels using techniques like majority voting or statistical fusion methods.
- Multi-atlas Capability: Using multiple atlases improves accuracy and helps handle anatomical variations between patients.
Development and Growth:
Atlas-based methods grew with advances in medical imaging technology and computing power. Early single-atlas approaches had limitations with anatomical variations. Modern multi-atlas techniques and improved registration methods have made these approaches central to medical image segmentation.
Practical Applications:
- Brain Analysis: Used to segment structures like the hippocampus and cortical regions for studying neurological conditions
- Abdominal Imaging: Helps identify organs like liver and kidneys for surgery planning
- Skeletal Imaging: Labels bones in X-rays and CT scans for fracture assessment
Advantages:
- Uses proven anatomical knowledge for better accuracy
- Performs well with standard anatomy
- Handles image noise effectively
- Can segment multiple structures at once
Disadvantages:
- Needs carefully chosen atlas images
- Takes significant computing power
- May struggle with unusual anatomical variations
- Registration errors affect results
Implementation Guidelines:
- Use Multiple References: Include several atlas images to better handle anatomical differences
- Optimize Registration: Select appropriate algorithms based on anatomy and available computing resources
- Add Local Adjustments: Include methods to fine-tune results in areas with significant anatomical differences
- Verify Atlas Choice: Ensure atlas images match your target population and imaging type
Atlas-based segmentation stands out for incorporating proven anatomical knowledge into image analysis, leading to reliable results for well-defined structures. While computationally intensive, improved algorithms and hardware continue to expand its use across medical imaging applications.
6. Watershed Segmentation
Watershed segmentation is an important image segmentation method that treats grayscale images like topographic landscapes. It works by simulating water flooding from the lowest points (valleys) of pixel intensity to create dividing lines called “watersheds” between different regions. This ability to naturally separate touching objects makes it a key tool in medical imaging.
Understanding the Concept
The main principle is finding object boundaries using image gradient information. The algorithm begins at the lowest intensity points and simulates rising water levels. As water from different low points is about to merge, virtual dams (watershed lines) are created to keep regions separate. These dams ultimately define the boundaries between different segments.
Key Features:
- Edge Detection: Uses image gradients to find meaningful boundaries between anatomical structures
- Marker Control: Allows users to guide segmentation by pre-selecting regions of interest
- Multi-level Analysis: Creates hierarchical region groupings for examining details at different scales
- Region Merging: Can combine segments based on size or intensity to improve accuracy
- Complete Boundaries: Ensures fully closed contours, which is essential for 3D medical imaging
Advantages:
- Very effective at separating touching or overlapping objects
- Performs well on images with clear edge definition
- Offers flexibility through hierarchical segmentation levels
Limitations:
- Over-segmentation: Can create too many regions due to image noise
- Noise Sensitivity: Often requires pre-processing like smoothing
- Marker Placement: Results heavily depend on accurate marker selection
- Processing Load: Can be demanding for large 3D image sets
Real-world Medical Applications:
- Cell Analysis: Separating and counting individual cells in microscopy images for leukemia diagnosis
- Tissue Segmentation: Distinguishing tumor tissue from healthy brain matter in MRI scans
- Bone Assessment: Measuring bone density and finding micro-fractures in CT images
History and Development:
While watershed segmentation is not new, it remains widely used in medical imaging because it handles complex shapes well. Modern computing power and improved marker-based methods have made it even more practical and effective.
Implementation Tips:
- Use Strategic Markers: Place markers carefully to minimize excess segmentation
- Apply Pre-processing: Use smoothing filters to reduce noise interference
- Consider Combined Methods: Mix watershed with other techniques like region growing
- Verify Results: Compare segmentation output against known reference images
Watershed segmentation continues to be valuable because it excels at a fundamental challenge in medical imaging – separating connected objects. Though it requires careful setup and parameter adjustment, its effectiveness in complex scenarios makes it essential for medical device makers, researchers and healthcare providers.
7. Graph Cut Segmentation
Graph Cut Segmentation is a key method for medical image segmentation that works by treating the image as a network of connected points. The approach converts each pixel into a node in a graph, with edges between nodes representing how similar neighboring pixels are. By using mathematical techniques to find the optimal way to split this graph, Graph Cut can separate important structures (like organs or tumors) from the background.
The method works by assigning higher weights to edges between similar pixels (like those within the same organ) and lower weights to edges between different pixels (like those at organ boundaries). The algorithm then finds the “minimum cut” – the smallest set of edges that needs to be removed to split the graph into two parts. This split effectively segments the image into foreground and background regions.
Features and Benefits:
- Graph Structure: The method can include both region-based information about pixel similarity and boundary information about edges between different areas
- Energy Function: Finding the minimum cut leads to the best possible solution by balancing regional and boundary information
- User Input: The method works well with user-provided hints about which areas are foreground vs background
- Optimal Results: Unlike some other methods, Graph Cut finds the mathematically best solution for the given graph setup
Pros:
- Best Possible Solution: Guarantees finding the optimal segmentation for how the graph is defined
- Works with Complex Shapes: Can accurately segment objects with irregular or complicated boundaries
- Multiple Information Sources: Uses both region similarity and boundary sharpness for better results
- User Control: Allows users to guide the segmentation when needed
Cons:
- Memory Usage: Converting large 3D medical images into graphs requires significant computer memory
- Speed Issues: Processing time increases with image size due to the mathematical complexity
- Manual Input: Some cases need user guidance, making full automation difficult
- Two-Region Focus: Basic Graph Cut works best for separating just two regions – extensions for more regions add complexity
Examples in Medical Imaging:
- Tumor Analysis: Finding precise tumor boundaries for treatment planning
- Organ Segmentation: Separating specific organs from surrounding tissues
- Lesion Detection: Identifying and outlining areas of tissue damage
Tips for Implementation:
- Graph Setup: Choose edge weights carefully based on the specific medical imaging application
- Software Tools: Use optimized computer programs for faster processing
- Multiple Regions: Consider special Graph Cut variations when segmenting more than two regions
- Parameter Balance: Adjust the importance of region vs boundary information for best results
Historical Impact:
Yuri Boykov’s research and publications, especially “Graph cuts in vision,” helped establish Graph Cut as a major tool in medical image analysis by showing its effectiveness and providing practical algorithms.
Graph Cut Segmentation remains valuable in medical imaging because it can find mathematically optimal solutions while considering both regional similarities and boundary information. Though computing resources can be a constraint, the method’s strengths make it essential for many medical applications.
8. Level Set Segmentation
Level set segmentation is a leading approach in medical image analysis that excels at handling complex anatomical shapes and changing structures. It represents object boundaries implicitly using a higher-dimensional level set function rather than explicit tracking. Think of it like a 3D landscape where the sea level contour represents the object boundary in a 2D image. This approach works especially well for analyzing dynamic medical structures like dividing cells or branching blood vessels.
The method works by evolving the level set function based on an image-guided speed function. This function considers factors like image gradients, intensity, and texture to guide the contour towards object boundaries. The evolution process also includes curvature-based smoothing to prevent jagged edges.
Key Features:
- Implicit representation: No need to explicitly track boundaries, making it easier to handle complex shapes
- Flexible topology: Naturally handles splitting and merging without complex tracking
- Customizable speed function: Can incorporate different image features and prior knowledge
- Smooth evolution: Produces clean, regularized contours through curvature terms
Advantages:
- Great for changing shapes: Perfect for objects that split, merge or deform
- Works in 3D: Easily extends to volumetric medical datasets
- Handles noise well: Implicit approach provides natural noise resistance
- Complex boundary detection: Accurately finds irregular anatomical shapes
Limitations:
- Computing intensive: Solving level set equations requires significant processing power
- Parameter sensitivity: Results depend heavily on speed function parameters
- Potential instability: Can become unstable without careful parameter selection
- Needs regular updates: Level set function requires periodic reinitialization
Common Applications:
- Blood vessel analysis: Effectively segments complex vascular networks
- Brain structure mapping: Identifies detailed brain anatomy in MRI scans
- Heart motion studies: Tracks movement of cardiac walls over time
Implementation Tips:
- Use efficient methods: Fast marching and narrow band approaches reduce computation
- Focus computation: Only update values near the evolving boundary
- Initialize carefully: Starting conditions significantly impact results
- Monitor stability: Watch for and address numerical instabilities
Historical Note: Stanley Osher and James Sethian developed the level set method for tracking interfaces. It has since become a cornerstone technique in medical image analysis.
Level set segmentation earns its place among key medical imaging tools through its unique ability to handle the complex, changing structures found in biological systems. While computationally intensive, its flexibility and robustness make it indispensable for many medical applications. The method’s journey from mathematical theory to practical medical tool demonstrates its lasting value in healthcare imaging.
8-Point Medical Image Segmentation Comparison
| Technique | Implementation Complexity (🔄) | Resource Requirements (⚡) | Expected Outcomes (⭐📊) | Ideal Use Cases | Key Advantages (💡) |
|---|---|---|---|---|---|
| Thresholding-Based Segmentation | Low; simple threshold selection, sometimes manual adjustments | Low; suitable for real-time processing | Effective for high-contrast images; may suffer in noisy/low-contrast settings | Bone segmentation, brain tumor detection, lung nodule CT | Computational efficiency and simplicity |
| Deep Learning-Based Segmentation (CNNs) | High; involves network design, training, and parameter tuning | High; requires GPUs and large training data | High accuracy and robustness; excels in complex pattern recognition | Organ segmentation, brain tumor segmentation, retinal vessel segmentation | Automatic feature learning and improved accuracy |
| Region Growing Segmentation | Moderate; seed selection and iterative region expansion | Moderate; iterative process may increase load | Effective for homogeneous regions; sensitive to seed placement | Liver tumor segmentation, cardiac chamber detection, breast lesion detection | Extracts connected regions using flexible criteria |
| Active Contour Models (Snakes) | Moderate to high; energy minimization and parameter tuning | Moderate; increased compute for complex shapes | Produces smooth boundaries; robust to noise with proper initialization | Cardiac ventricle segmentation, cell boundary detection, vessel segmentation | Robust shape handling and prior knowledge integration |
| Atlas-Based Segmentation | Moderate; requires atlas registration and label fusion | High; computationally expensive | Anatomically consistent segmentation; works best with normal anatomical structures | Brain structure, abdominal organ segmentation, skeletal labeling | Leverages anatomical knowledge and noise robustness |
| Watershed Segmentation | Moderate; marker-controlled options reduce issues like oversegmentation | Moderate; standard computational demand | Produces closed contours and effective separation; risk of oversegmentation exists | Cell segmentation, tissue separation, bone structure analysis | Hierarchical results with effective edge delineation |
| Graph Cut Segmentation | High; involves complex graph construction and optimization | High; memory intensive with larger images | Globally optimal segmentation; handles complex topologies | Tumor segmentation, organ boundary detection, lesion separation | Integrates regional and boundary information well |
| Level Set Segmentation | High; implicit contour evolution with critical parameter selection | High; computationally demanding | Robust handling of topological changes and complex shapes | Vessel segmentation, brain structure analysis, cardiac motion tracking | Natural 3D extension with flexible boundary evolution |
The Future of Medical Image Segmentation
Medical image segmentation has evolved from basic methods like thresholding and region growing to highly capable deep learning systems. While classic techniques like atlas-based and watershed segmentation remain useful, Convolutional Neural Networks (CNNs) now deliver the highest accuracy. A thorough grasp of each method’s capabilities and constraints – from graph cuts to level sets – helps determine the best approach for specific tasks.
The selection of segmentation techniques requires evaluating multiple factors carefully. Key considerations include the imaging type (CT, MRI, ultrasound), anatomical target, required precision level, and available computing power. For example, while deep learning models achieve excellent results, they need substantial computational resources and large training datasets. In contrast, basic thresholding may work well for high-contrast structures.
Professional growth is essential in this fast-moving field. Keeping up with new developments in deep learning architecture design, loss functions, and optimization methods is critical. Additionally, finding novel ways to combine CNNs with traditional approaches or adapt models to different imaging types helps expand what’s possible in medical image segmentation.
Current developments show increasing focus on 3D and 4D segmentation, allowing detailed analysis of anatomical structures and their changes over time. Real-time applications are becoming more practical thanks to better hardware and optimized algorithms, enabling use during surgery and time-critical procedures. Combining image segmentation with genomic data and electronic health records also creates opportunities for more precise, personalized diagnoses.
Key Takeaways:
- Deep learning and CNNs have dramatically improved medical image segmentation
- Traditional methods remain valuable and can enhance deep learning solutions
- Technique selection depends on specific use cases and resource availability
- Continuous professional development is vital in this dynamic field
- Future advances focus on 3D/4D analysis, real-time use, and integrated data
Looking to improve your medical imaging capabilities with AI-powered segmentation? PYCAD provides complete solutions from data processing to model training and deployment, helping you increase diagnostic accuracy and operational efficiency. Partner with us to enhance your medical devices and patient care.