Medical imaging software is the digital engine room of modern diagnostics. It’s what allows clinicians to take the raw data from an MRI, CT scan, or X-ray and transform it into a crystal-clear picture they can actually use to diagnose and treat patients. It's the critical link between a scanner and a life-saving decision.
This software essentially replaces the old, cumbersome world of physical film with a dynamic digital toolkit. It’s what makes collaborative, precise, and fast patient care a reality.
What Is Medical Imaging Software?
Think of it like a highly sophisticated digital workshop for doctors. Instead of just showing a static picture, this software gives them the tools to interact with it—to zoom in on a tiny detail, rotate a 3D model of an organ, or measure the exact size of a tumor.
It’s an entire ecosystem that handles the complete journey of a medical image. It starts the moment a scanner captures the data, continues as it’s securely stored and organized, and finishes when a specialist, maybe even one on the other side of the world, pulls it up for a second opinion. The software manages that whole process securely and efficiently.
The Core Components Explained
To really get what this software does, you have to understand the main pieces of the puzzle. A few core systems work in tandem to make sure every image is captured, stored, viewed, and shared correctly. Without them, it would be digital chaos.
Before diving into the individual parts, it's helpful to see how they fit together. The following table breaks down the essential software types in a medical imaging ecosystem, what they do, and a simple analogy for each.
Core Components of Medical Imaging Ecosystems
| Component | Primary Function | Analogy |
|---|---|---|
| DICOM | The universal file format and communication protocol for medical images. | A universal language. It ensures an image from a GE scanner can be perfectly understood by a Siemens viewing station, just like English allows people from different countries to communicate. |
| PACS | A localized digital archive for storing and accessing images within a specific department (e.g., radiology). | A departmental library. It’s the go-to place for radiologists to find and review all the books (scans) belonging to their section of the hospital. |
| VNA | A central, enterprise-wide archive that consolidates images from multiple PACS and departments. | A central city library. It brings together collections from all the smaller neighborhood libraries (departments) into one massive, standardized, and easily searchable archive for the entire city (hospital system). |
Let’s look a little closer at what each of these components actually does.
-
DICOM (Digital Imaging and Communications in Medicine): This is the foundation of it all. DICOM is the universal standard that lets imaging equipment and software from different manufacturers talk to each other. It’s the reason a radiologist can open an MRI from one machine on a viewing station made by a completely different company. It’s the bedrock of interoperability.
-
PACS (Picture Archiving and Communication System): This is the digital filing cabinet for a hospital's imaging department. A PACS securely stores huge volumes of scans and makes them instantly available to doctors and technicians across the hospital network. It’s what killed the need for giant, dusty rooms filled with physical film.
-
VNA (Vendor Neutral Archive): A VNA takes things a step further. While a PACS often serves one department, a VNA is a master archive for the entire healthcare organization. It pulls in imaging data from radiology, cardiology, oncology, and more, breaking down data silos. Think of it as a universal translator that consolidates everything into one central, long-term repository.
The shift to these digital systems isn't just a trend; it's a massive economic driver. The global medical imaging software market was valued at USD 7.6 billion in 2024 and is on track to hit USD 13.93 billion by 2033. That steady growth highlights just how essential these tools have become for improving patient care. You can explore detailed market growth reports on Straits Research to see the full picture.
How AI Is Changing the Game in Medical Imaging

AI in medicine isn’t some far-off concept anymore. It's here, and it’s fundamentally changing how medical imaging software works. The best way to think about it is to imagine AI as a highly-trained partner for the radiologist. It doesn't replace their expertise—it enhances it, acting like a second set of eyes that can spot patterns a human might miss.
This technology marks a huge shift from a purely manual, observational process to one that’s augmented by powerful data analysis. AI algorithms are trained on millions of images, teaching them to recognize the incredibly subtle signs of different diseases. This allows them to flag potential problems with a speed and accuracy that were previously unthinkable.
Automated Detection and Smarter Triage
One of the most powerful applications of AI is its ability to automatically detect abnormalities. For instance, an AI model can scan a chest CT and immediately highlight a tiny, suspicious nodule that could be an early-stage cancer. This gives radiologists a huge head start, allowing them to prioritize the most critical cases first.
This isn't just about working faster; it's about building a better safety net. Radiologists face enormous workloads, and AI helps reduce the chance of human error while making sure that urgent findings get immediate attention.
- Anomaly Flagging: AI systems are trained to spot anything that deviates from normal anatomy, automatically flagging areas of concern for a specialist to review.
- Intelligent Prioritization: A scan showing signs of a stroke or intracranial hemorrhage can be automatically bumped to the top of the reading queue.
- Unwavering Consistency: The software applies the same rigorous analysis to every single scan, day or night, ensuring a consistent standard of care.
Advanced Image Segmentation and Analysis
Beyond just finding potential problems, AI is brilliant at precisely outlining and measuring them. This process, called segmentation, is absolutely vital for planning treatments.
Think about a surgeon getting ready to remove a brain tumor. An AI-powered tool can generate a perfect 3D model of that tumor in minutes. It can clearly define its borders and show exactly how close it is to critical brain structures—information that is crucial for a successful surgery. What used to be a painstakingly manual task now takes a fraction of the time.
By taking over repetitive and time-consuming jobs like organ segmentation, AI frees up clinicians to focus on what they do best: solving complex diagnostic puzzles and interacting with patients.
Predictive Insights and Forecasting Disease
Perhaps the most exciting frontier for AI in imaging is its ability to predict what might happen next. By analyzing subtle changes in scans over time—changes often invisible to the human eye—AI models can start to forecast how a disease might progress.
An algorithm might, for example, predict the likelihood of a patient's multiple sclerosis lesions getting worse based on hidden patterns in their MRI scans.
This opens the door to truly personalized, proactive medicine. It allows doctors to step in earlier and adjust treatment plans based on solid, data-driven forecasts instead of waiting for symptoms to appear. The progress we're seeing in medical imaging is directly tied to the incredible innovation happening across the broader AI industry landscape, which continues to push the boundaries of what's possible in diagnostic care.
Unlocking Better Diagnostics and Workflows

Beyond the impressive technology, the real story of medical images software is how it changes lives—for both patients and the clinicians who care for them. This isn't just about fancy features; it's about translating that power into tangible benefits that reshape diagnostics and daily hospital operations. Think of it as the critical link between a raw digital scan and a life-saving decision.
The most immediate and profound impact is the surge in diagnostic confidence. By equipping clinicians with tools for 3D visualization, precise measurements, and instant comparisons of old and new scans, the software helps them see the complete story. This clarity is instrumental in catching subtle issues early and reducing the risk of diagnostic errors.
A New Era of Diagnostic Precision
Advanced visualization tools completely change the game, turning flat, grayscale images into interactive, multi-dimensional models. Imagine a radiologist being able to virtually "fly through" a CT scan of a patient's lungs, inspecting a tiny, suspicious nodule from every possible angle. That's a level of detail you just can't get from a stack of 2D images.
This deeper insight directly translates to better patient outcomes. It makes staging tumors more accurate, identifying vascular blockages clearer, and assessing how well a treatment is working far more precise. In the end, this precision allows for care plans that are truly tailored to the individual.
By making complex anatomical structures easier to interpret, modern medical imaging software acts as a powerful clarifying lens, helping clinicians spot problems that might otherwise be missed. This heightened accuracy is a cornerstone of modern patient safety.
Streamlining the Entire Clinical Workflow
The efficiency gains are just as significant. Not long ago, getting a patient's old X-rays meant digging through a dusty physical archive, a process that could take hours. Now, with integrated medical images software, a clinician can pull up a patient’s entire imaging history—spanning years and multiple scan types—in a matter of seconds.
This immediate access completely overhauls the clinical workflow.
- Faster Reporting: Radiologists can dictate their findings right into the system, using templates that automatically pull in patient data. This simple step slashes the time spent on administrative busywork.
- Seamless Collaboration: A specialist in a major urban hospital can instantly review a complex scan with a doctor in a remote rural clinic. Geographical barriers to expert care simply disappear.
- Reduced Turnaround Times: The whole cycle, from the moment a scan is taken to the delivery of the final report, gets shorter. That means patients get their diagnosis and start treatment sooner.
The Human Impact of Better Imaging
Let's look at a real-world scenario: a patient needs complex surgery to remove a tumor dangerously close to a major artery. In the past, the surgical team would rely on 2D scans and their own experience to navigate this delicate procedure.
Today, medical images software can build an exact 3D model of that tumor and its relationship to the surrounding anatomy. The team can use this model to meticulously plan their approach, down to the millimeter, before ever making an incision. They can even run through a virtual rehearsal of the surgery, spotting potential hurdles and refining their strategy. This level of preparation doesn't just make the operation safer—it often leads to less invasive procedures and a faster recovery for the patient.
Understanding Different Imaging Modalities
Medical imaging isn't one single technology; it’s a whole collection of different tools, each giving us a unique window into the human body. Because of this, good medical images software has to be a jack-of-all-trades, built to handle the specific quirks and demands of every imaging type. It's a lot like a professional kitchen—you wouldn't use a bread knife to filet a fish, and you can't use basic X-ray software to analyze a complex MRI scan.
Each modality creates data in a completely different way. An X-ray is a flat, 2D shadow, while an MRI builds a sophisticated 3D model using magnetic fields. This means the software requirements aren't just slightly different; they're fundamentally distinct. Getting a handle on these differences is the first step to understanding why a one-size-fits-all software solution just doesn't cut it in a real clinical setting.
X-Ray and Computed Tomography (CT)
We all know the X-ray. It uses a small dose of radiation to create 2D images of dense stuff in the body, like bones. It’s incredibly fast and effective, making it the go-to for diagnosing a broken arm or spotting pneumonia in the lungs. Software for X-rays is usually straightforward, focusing on sharp, high-contrast viewing and simple tools for annotations and measurements.
Computed Tomography (CT) is essentially an X-ray on steroids. Instead of one flat picture, a CT scanner takes a whole series of X-ray images from every angle and then uses a computer to stitch them together. The result is a set of detailed cross-sectional "slices" of the body.
- Primary Use: CT is fantastic for getting a clear look at bones, soft tissue, and blood vessels all at once. It’s a workhorse in the ER for trauma cases, cancer staging, and finding internal bleeding.
- Software Needs: The real magic here is in the processing power. The software has to be robust enough to reconstruct all those slices into a single, cohesive 3D model that a radiologist can digitally spin around and examine from any angle.
Magnetic Resonance Imaging (MRI)
Unlike X-rays and CTs, Magnetic Resonance Imaging (MRI) uses zero ionizing radiation. Instead, it relies on powerful magnets and radio waves to create incredibly detailed images of soft tissues—think the brain, muscles, tendons, and ligaments. This makes it indispensable for neurological exams, diagnosing joint injuries, and spotting certain tumors that other scans might miss.
Because MRI data is so rich and complex, the software has to match that sophistication. It needs advanced visualization tools and what’s called multi-planar reconstruction, which lets clinicians view the anatomy from any plane—top-down, side-on, or front-to-back—without rescanning the patient.
Ultrasound and Its Real-Time Demands
Ultrasound, or sonography, uses high-frequency sound waves to create live, moving pictures of what’s happening inside the body. Its biggest advantage is that it’s dynamic. You can see things in real-time, which is why it’s invaluable in obstetrics for watching a fetus develop or in cardiology for observing the heart muscle pump blood.
Because ultrasound is a live-capture modality, the software must be optimized for real-time video processing and analysis. It needs to handle high frame rates and provide tools for measuring flow and movement as they happen.
To give you a sense of how these modalities fit into the bigger picture, it helps to look at the global medical image analysis software market. An analysis of market share shows some interesting shifts. While ultrasound held the largest share at 31% back in 2016, its slice of the pie is expected to shrink slightly to 29% by 2025. Meanwhile, MRI and CT are on the rise; MRI's share is projected to grow from 12% to 14%, and CT's from 15% to 16% over the same period. You can learn more about medical imaging market trends to see how these technologies are evolving.
To see how these modalities stack up in practice, here's a quick overview of their common uses and the key software features they depend on.
Comparison of Medical Imaging Modalities
| Modality | Primary Use Case | Key Software Feature |
|---|---|---|
| X-Ray | Bone fractures, chest imaging | High-contrast viewing, annotation, and simple measurement tools |
| CT | Trauma, cancer staging, vascular disease | 3D volume rendering, multi-planar reconstruction (MPR) |
| MRI | Neurological exams, soft tissue injuries | Advanced visualization, image segmentation, functional analysis |
| Ultrasound | Obstetrics, cardiology, real-time guidance | Live video processing, Doppler flow analysis, high frame rate support |
Ultimately, each imaging type tells a different part of the patient's story, and the software is what translates that data into a clear, actionable diagnosis.
This chart breaks down some of the key performance metrics for popular imaging software solutions, comparing them on speed, cost, and user satisfaction.
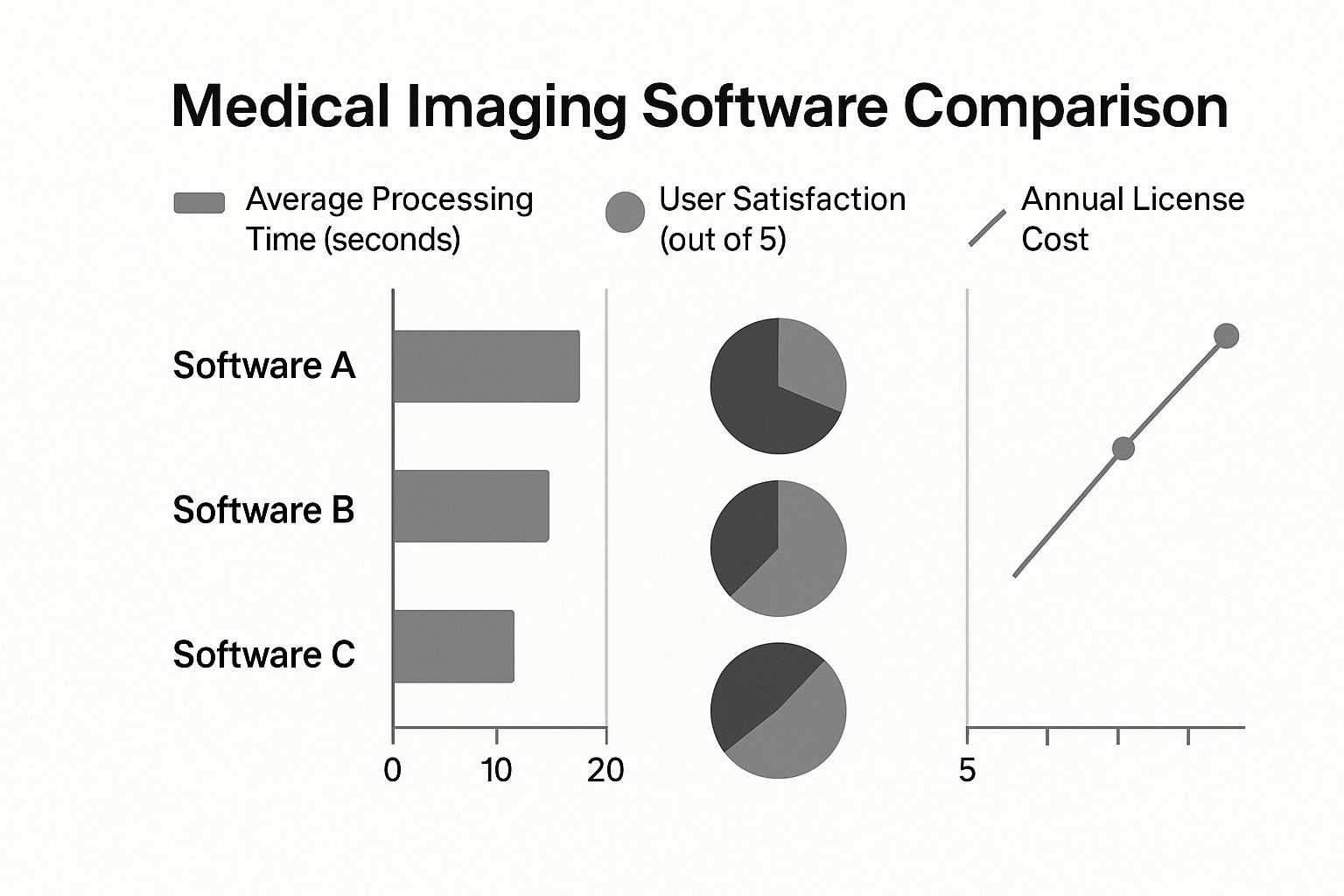
As you can see, there's often a direct trade-off between pure processing speed and overall cost—a critical factor when a clinic or hospital has to choose a platform that fits its specific workflow and budget. A truly great medical images software platform is one that’s expertly built to handle all of these varied and highly specialized demands under one roof.
How to Choose the Right Imaging Software

Choosing the right medical imaging software is a foundational decision, not just another IT purchase. Think of it as designing the central nervous system for your hospital's entire imaging operation. Get it right, and you streamline workflows and improve diagnostics. Get it wrong, and you're stuck with frustrated clinicians, data silos, and a system that actively works against efficiency.
To make the right call, you need a team effort. Bring radiologists, IT staff, department heads, and administrative leaders to the table. Each person offers a critical perspective, making sure the solution you pick can handle the real-world complexities of a modern healthcare environment. The goal isn't just to find a tool that works today, but one that can grow with you tomorrow.
Start With Seamless Interoperability
Your new software can't be an island. Its ability to communicate with your existing health IT infrastructure isn’t just a nice-to-have; it's the most critical technical feature. It’s like hiring a new team member—they absolutely must speak the same language as everyone else from day one.
The top priority is a rock-solid connection to your Electronic Health Record (EHR). Clinicians have to be able to pull up patient images directly within the EHR, period. Logging into a separate application just to view a scan is a workflow killer.
Beyond the EHR, the software must play nicely with your Picture Archiving and Communication System (PACS) or Vendor Neutral Archive (VNA). True interoperability means the system can effortlessly pull historical studies from these archives and push new ones back without creating duplicates or data conflicts.
Prioritize Security and Regulatory Compliance
In healthcare, data security is non-negotiable. It's a legal and ethical mandate that underpins patient trust. The software you select must offer robust protection for sensitive patient information, with built-in features to prevent breaches and unauthorized access.
Look for explicit proof that the software meets key regulations:
- HIPAA (Health Insurance Portability and Accountability Act): This is the baseline for any organization handling patient data in the United States.
- GDPR (General Data Protection Regulation): If you manage data for any EU patients, this is a firm requirement.
- FDA Clearance: For any AI tools intended for diagnosis, make sure they have the proper regulatory sign-off. The FDA has already cleared nearly 700 AI/ML-enabled medical devices, so this is a standard expectation.
A vendor's commitment to security should be obvious and provable. Don't be shy about asking for detailed documentation on their security protocols, encryption methods, and audit results. If you get a vague answer on security, that's a major red flag.
Evaluate Scalability and Future-Readiness
Medical imaging data is growing at an incredible rate. The average hospital now generates around 50 petabytes of data each year, and roughly 80% of that is medical images. Your software has to handle this massive, ever-expanding volume without grinding to a halt.
This is where you should seriously consider a solution built on a cloud-based infrastructure. Cloud platforms offer almost limitless scalability, letting you add storage and processing power as needed without huge upfront hardware investments. It’s the only practical way to ensure your system won't buckle under the pressure as you start performing more advanced—and much larger—scans like 3D CTs.
Focus on an Intuitive User Experience
The most powerful software in the world is useless if your team hates using it. A clunky, confusing interface doesn't just waste time; it actively contributes to clinician frustration and burnout. The user experience (UX) has to be a top priority, not an afterthought.
An intuitive system means radiologists can view, manipulate, and report on images quickly and without friction. Common tools should be easy to find, buttons should make sense, and the learning curve should be gentle. The best way to vet this is to get your hands on the software. Insist on a live demo or, better yet, a trial period so your clinical team can give it a real-world test drive. Their buy-in is absolutely essential for a successful rollout.
Best Practices for Implementation and Integration
Choosing the right medical imaging software is a huge win, but it’s really just the first step. The real magic happens during implementation—the process of actually getting the system integrated into your daily workflows. Without a smart rollout, even the most powerful software will just gather digital dust.
This isn't just about plugging in a new server. It's about fundamentally changing how your clinical teams operate. It requires meticulous planning, from migrating years of patient data without losing a single file to making sure every user feels comfortable and confident from day one. A well-thought-out strategy prevents chaos and gets everyone on board quickly.
Crafting a Solid Data Migration Plan
One of the most nerve-wracking parts of any software transition is moving all that existing data. Losing or corrupting a patient's imaging history is simply not an option. The entire process has to be secure, precise, and double-checked at every turn.
A phased migration is almost always the safest route. Instead of trying to move everything at once in a "big bang" transfer, think about migrating department by department or even one imaging modality at a time. This breaks the massive task into manageable chunks, letting your IT team validate each batch and fix any small issues before they become system-wide problems.
Here are a few key steps to get right:
- Data Cleansing: Start by tidying up your current archives before you move anything. This means getting rid of duplicate files, standardizing how things are named, and fixing any existing errors.
- Validation and Auditing: Once a batch of data is moved, you need to run rigorous checks to confirm every single image and its associated metadata transferred perfectly.
- Legacy System Decommissioning: Set a firm, clear date for when the old system will be switched off. This prevents staff from getting confused and accidentally saving new studies to the outdated platform.
Driving Adoption Through Training and Change Management
Technology is only one part of the equation; the human element is just as critical. If your clinicians find the new software clunky or confusing, they'll just find workarounds. That's why top-notch training and a solid change management plan are non-negotiable.
Training can't be a one-size-fits-all, one-day event. It needs to be tailored to specific roles and be an ongoing resource. A radiologist, a surgeon, and a referring physician all use the software differently and need training that reflects that. Offer a mix of learning options—live workshops for hands-on practice, on-demand video tutorials for quick refreshers, and handy cheat sheets for at-the-elbow support.
Successful adoption hinges on turning your clinical staff into advocates, not obstacles. By involving them early and addressing their concerns directly, you build the buy-in needed to overcome natural resistance to change.
It's also a great idea to identify a few "super-users" in each department. These are the tech-savvy team members who can act as the go-to person for their colleagues, championing the new system and answering simple questions on the spot. Finally, to keep everything running smoothly, remember that reliable data transfer is key, especially when dealing with patient records. It's crucial to follow best networking practices for Electronic Health Records (EHR). Getting the network infrastructure right from the start ensures your newly integrated system performs exactly as it should.
Frequently Asked Questions
When you're dealing with something as complex as medical imaging software, questions are bound to come up. Whether you're in the IT department, on the clinical floor, or managing the budget, it's a big topic. Let's break down some of the most common questions we hear.
What's the Real Difference Between PACS and VNA?
It helps to think of it like this: a PACS (Picture Archiving and Communication System) is like a department's dedicated workshop, while a VNA (Vendor Neutral Archive) is the central warehouse for the entire organization.
The radiology department's PACS is built for speed and their specific day-to-day workflow. It's a high-performance system designed to get images in front of radiologists quickly.
A VNA, on the other hand, plays the long game. It’s designed to pull in and store images from every department—radiology, cardiology, pathology, you name it—into a single, standardized archive. This breaks down the walls between different clinical systems, giving you a complete, lifelong imaging history for every patient.
The key takeaway is that a VNA provides a long-term, unified storage strategy for the entire organization, while a PACS serves the immediate, high-speed needs of a specific clinical department.
Just How Secure Is Medical Imaging Software?
It absolutely has to be, and reputable platforms are built with security as a non-negotiable foundation. These systems are designed to meet stringent regulations like HIPAA in the U.S. and GDPR in Europe. This isn't just a single feature; it's a multi-layered defense strategy.
You'll almost always find these core security measures in place:
- End-to-End Encryption: Patient data is scrambled and unreadable, both when it's sitting on a server (at rest) and when it's being sent over a network (in transit).
- Strict Access Controls: Security is role-based. A surgeon in the OR can see the images for their patient, but they can't browse the records of another department. Everyone gets access only to what they need.
- Comprehensive Audit Trails: The system keeps a meticulous log of every single action. You can see exactly who accessed a patient's file, what they did, and when they did it.
How Does This Software Even Handle Such Huge Files?
Medical image files are massive. A single 3D CT scan can be made up of thousands of individual image slices. Trying to manage that much data with older technology would be a nightmare, but modern software is built for it.
This is where cloud-native platforms truly shine. They use highly scalable storage solutions, like Amazon S3, that can grow to handle practically infinite amounts of data. You don't have to worry about running out of space or buying another expensive server rack. The entire system is engineered for performance, so a clinician can pull up a massive study and scroll through it smoothly, without any frustrating lag.
At PYCAD, we build the intelligent engine inside the next wave of medical imaging tools. From annotating data to deploying powerful AI models, we partner with innovators to develop smarter, faster, and more precise diagnostic software. Find out how we can help you build the future at https://pycad.co.






