Medical imaging quality assurance (QA) is the methodical process of making sure every single diagnostic image is clear, accurate, and safe for the patient. Think of it as the essential pre-flight check for healthcare. It’s the very foundation of diagnostic confidence and patient safety.
Why Medical Imaging Quality Assurance Matters
You wouldn't want a pilot to skip their pre-flight safety check before takeoff, would you? The same critical importance applies to medical imaging. A solid QA program is so much more than a technical checklist; it’s a clinical and ethical must-have that directly affects patient outcomes every single day.
Without it, even the most sophisticated, multi-million dollar imaging equipment becomes unreliable.
At its heart, medical imaging quality assurance stands guard over diagnostic integrity. It’s the system that guarantees the images a radiologist sees are a true and precise representation of the patient's internal structures. A fuzzy MRI, a warped X-ray, or a CT scan full of artifacts isn’t just a bad picture—it's a potential detour toward a devastating misdiagnosis or a missed chance for early, life-saving treatment.
The Human Impact of High-Quality Imaging
The stakes couldn't be higher. Take the global battle against non-communicable diseases (NCDs) like cancer, stroke, and cardiovascular conditions. These diseases are responsible for a shocking 74% of all deaths worldwide. For nearly all of them, high-quality medical imaging is non-negotiable for an accurate diagnosis and a solid treatment plan.
The World Health Organization (WHO) has repeatedly stressed the urgent need to improve medical imaging capacity and quality around the globe, directly connecting it to better patient care. You can learn more about the WHO's global health initiatives and imaging's role from our partners at Philips.
A disciplined QA program brings real, tangible benefits that ripple throughout a healthcare facility:
- Prevents Misdiagnosis: Sharp, precise images give radiologists the confidence they need to make the right call, avoiding the serious fallout from a diagnostic error.
- Minimizes Radiation Exposure: QA protocols, especially for CT and X-ray, are designed to follow the ALARA principle (As Low As Reasonably Achievable), protecting patients from radiation they don’t need.
- Builds Patient and Clinician Trust: When a facility consistently produces high-quality results, it builds trust with both referring physicians and patients, cementing its reputation for excellence.
Quality assurance isn't just an expense; it's a direct investment in patient safety and diagnostic certainty. It elevates an imaging department from a service that just takes pictures to a cornerstone of clinical decision-making.
Ultimately, QA provides the framework that lets incredible technology live up to its promise. It ensures that every scan, every single time, is optimized to deliver the most diagnostic value possible. This unwavering commitment to quality is what all successful patient diagnoses are built on, making it a non-negotiable part of modern medicine.
The Three Pillars of an Effective QA Program

A top-tier medical imaging quality assurance program isn't just a checklist; it's a solid structure built on three critical pillars. If any one of them is shaky, the whole system becomes unreliable. By focusing on these core areas, any facility can create a resilient foundation for diagnostic confidence.
These pillars are Equipment Performance, Process Consistency, and Personnel Competency. They work together to cover the technology, the workflows, and the human expertise, ensuring every single image is both safe and diagnostically sound.
Pillar 1: Equipment Performance
Think of a multi-million dollar MRI or CT scanner like a high-performance race car. It doesn't matter how skilled the driver is if the engine is misfiring or the tires are worn. The car simply won't perform. The same is true for your imaging equipment.
Equipment Performance is the pillar that keeps these sophisticated machines in peak condition. It’s all about a strict schedule of testing and preventative maintenance to ensure the hardware is performing exactly as it should. These aren't just box-ticking exercises; they're your first line of defense against poor image quality.
Key activities include:
- Acceptance Testing: This is done the moment new equipment arrives. It's a thorough check to confirm it meets the manufacturer's promises and is ready for patient use.
- Routine Quality Control (QC): These are the regular check-ups, often done daily or weekly by technologists. They use special tools called "phantoms" to test for consistency and catch any drift in performance.
- Annual Performance Evaluations: A deep dive conducted by a qualified medical physicist. They rigorously assess everything from image sharpness (spatial resolution) to the radiation dose.
Neglecting equipment performance is a recipe for disaster. It can lead to artifacts, electronic noise, or distorted images—flaws that could easily hide a small tumor or mimic a pathology that isn't there, leading to a misdiagnosis.
Pillar 2: Process Consistency
The second pillar, Process Consistency, is all about creating a reliable, repeatable system. Imagine a world-class orchestra where every musician plays from the same sheet music, at the same tempo. The result is a perfect symphony. In imaging, our "sheet music" is our standardized protocols.
This pillar ensures that every patient gets the same high standard of care and that their scans are comparable over time, no matter which technologist is on duty. It’s about stamping out the variables that undermine quality.
Process consistency eliminates variability, which is the enemy of quality. It ensures that a patient's follow-up scan in six months can be accurately compared to their baseline scan today.
This standardization touches every part of the imaging journey—from how a patient is scheduled and prepped to the specific acquisition settings and even how images are labeled. The need for this level of reliability is growing fast. The global medical imaging market was valued at USD 41.6 billion in 2024 and is expected to climb, driven by an aging population and more chronic diseases. You can explore more insights on medical imaging market growth on Grandview Research. This growth only amplifies the need for consistent, high-quality data.
To illustrate how these QA tests vary by machine, here’s a quick overview of some essential checks for different imaging systems.
Key QA Activities Across Imaging Modalities
| Imaging Modality | Key QA Test Example | Purpose of Test |
|---|---|---|
| X-ray/Radiography | Collimator and Beam Alignment | Ensures the X-ray beam is precisely aligned with the light field, minimizing patient radiation exposure to areas not being imaged. |
| CT Scanner | CT Number Accuracy (using a water phantom) | Verifies that the scanner accurately represents tissue densities. Water should always measure 0 Hounsfield Units (HU). |
| MRI | Signal-to-Noise Ratio (SNR) | Measures the strength of the useful image signal relative to background noise. High SNR is crucial for clear, detailed images. |
| Ultrasound | Geometric Accuracy (using a phantom with pins) | Checks that the system accurately measures distances and sizes, which is critical for things like fetal biometry or organ sizing. |
As you can see, while the goal of quality is universal, the specific checks are tailored to the unique physics and technology of each machine.
Pillar 3: Personnel Competency
The final, and arguably most important, pillar is Personnel Competency. At the end of the day, technology and processes are only as good as the people who run them. A state-of-the-art scanner and a flawless protocol mean very little in untrained hands.
This pillar focuses on the continuous education, training, and skill assessment of the entire imaging team—from the radiologists and technologists to the medical physicists and support staff. It ensures everyone not only knows what to do but why they're doing it. For a deeper dive into the skills required, exploring resources on the mastery of QA workflows and techniques can provide valuable context.
Competency is built and maintained through:
- Initial Training and Credentialing: Verifying that every team member has the proper qualifications and certifications from day one.
- Ongoing Education: Keeping everyone current on new technologies, evolving safety standards, and advanced imaging techniques.
- Performance Reviews: Regularly assessing skills to provide constructive feedback and spot opportunities for professional growth.
A competent team is nimble. They can troubleshoot unexpected problems, adapt to new challenges, and champion a culture where quality is everyone's responsibility. By investing in these three pillars, a healthcare facility can build a truly world-class QA program that patients can trust.
What Makes a Good Medical Image? Measuring Quality
We can all look at a picture and decide if it's blurry or sharp. But in medicine, "good enough" isn't good enough. While a radiologist's trained eye is the ultimate judge, a truly reliable medical imaging quality assurance program can't run on subjective opinion alone. It needs objective, consistent measurements.
These metrics are what turn the vague concept of "image quality" into solid numbers. They provide the data we need to track how well our equipment is performing and, ultimately, how much confidence we can place in a diagnosis. Think of them as the vital signs for the scanner itself.
Signal-to-Noise Ratio: Finding the Signal in the Static
One of the most foundational concepts in imaging is the Signal-to-Noise Ratio (SNR). Imagine you’re trying to listen to a quiet conversation (the signal) at a loud party (the noise). If the chatter is too loud, you can't make out the words. It's the same principle here.
In medical imaging, the "signal" is the meaningful data from the patient’s body that creates the picture. The "noise" is the random, grainy, visual static that can obscure it. A scan with high SNR is crisp and clear; one with low SNR is fuzzy and difficult to interpret.
A high Signal-to-Noise Ratio is essential for seeing subtle details. It's the difference between clearly identifying a small lesion and having it be completely obscured by visual static.
Getting a high SNR often involves a trade-off. We can boost the signal, but it might mean a longer scan time or a higher radiation dose. A good QA program is all about finding that sweet spot—the settings that produce the clearest possible image while keeping the patient safe. A sudden drop in SNR during a routine check is a big red flag that the scanner needs maintenance, fast.
Spatial Resolution: It’s All About the Details
Next up is Spatial Resolution, which is all about detail. Think about the difference between an old standard-definition TV and a modern 4K screen. The 4K TV can show incredibly fine textures because it has more pixels packed into the same space.
Spatial resolution is the imaging system's ability to tell two tiny, adjacent objects apart. This isn’t just an academic detail; it has huge clinical implications. High spatial resolution is absolutely critical when you need to:
- Trace the delicate, branching paths of tiny blood vessels.
- Spot microcalcifications on a mammogram, often an early sign of breast cancer.
- Examine the tiny, intricate bones of the inner ear.
Without excellent spatial resolution, these small but vital structures would just blur together. It directly impacts a doctor's ability to diagnose conditions that hide in the smallest anatomical features.
Phantom Testing: The Secret to Consistency
So, how do we measure these things day in and day out? We can't use real patients—everyone is built differently. That's where phantom testing becomes essential.
Phantoms are specially designed objects built from materials that act like human tissue when scanned. They contain precise patterns, grids, and shapes that allow us to test a scanner's performance in a perfectly controlled and repeatable way.
By scanning the exact same phantom every day or week, technologists build a log of the machine's performance. This data trail allows medical physicists to spot subtle drifts in SNR or spatial resolution over time. It’s an early warning system that flags a problem long before it ever affects a patient scan, providing the hard evidence needed for maintenance and repairs.
Mapping the QA Workflow From Patient to Report
Quality assurance in medical imaging isn't just a single step; it's a continuous process that follows the patient from the moment they're scheduled for a scan until a final, accurate report is in the physician's hands. Think of it as a series of crucial checkpoints, each designed to protect the patient and ensure the final image tells the right clinical story.
This journey is best understood by breaking it down into three key phases: Pre-Scan, During the Scan, and Post-Scan. Every member of the clinical team has a part to play in these stages. By mapping out this flow, a facility can spot potential weak points and build a stronger, safer process from start to finish.
Pre-Scan: The First Line of Defense
The QA process kicks off long before the patient even sees the scanning equipment. The Pre-Scan phase is all about meticulous preparation to head off problems down the line. It's a lot like a pilot's pre-flight checklist—getting these initial steps right is absolutely essential for a safe and successful outcome.
First up is positive patient identification. This simple but vital check confirms the right patient is about to get the right scan, preventing dangerous mix-ups. The technologist then verifies the doctor's orders and carefully reviews the patient’s history for any red flags, like metal implants for an MRI or allergies to contrast dye.
Finally, they select the correct imaging protocol. This is essentially the "recipe" of scanner settings, fine-tuned for the specific body part and the clinical question being asked. Using the wrong protocol can easily lead to a useless scan, forcing a repeat procedure and exposing the patient to unnecessary radiation.
The Pre-Scan phase is where more than 50% of potential errors can be caught and prevented. It is the most effective and lowest-cost opportunity to ensure quality.
During the Scan: Real-Time Quality Control
As soon as the patient is on the scanner table, we enter the During the Scan phase. This is where the technologist's hands-on expertise becomes the core of quality assurance. They aren't just pushing buttons; they're actively managing quality in real time.
Their responsibilities are dynamic and require sharp attention to detail:
- Patient Positioning: Getting the patient positioned perfectly is critical. Even a tiny misalignment can warp the anatomy on the screen, making a confident diagnosis much harder for the radiologist.
- Artifact Monitoring: Technologists are constantly on the lookout for artifacts—those strange distortions on an image caused by patient movement, implants, or equipment glitches. They have to spot the cause and fix it on the fly.
- Dose Optimization: For scans involving radiation, like CT and X-ray, technologists live by the ALARA principle (As Low As Reasonably Achievable). Their job is to use the absolute minimum radiation dose needed to get a clear, diagnostic-quality image.
This stage is a constant dance between technical skill and critical thinking, with the technologist acting as the direct guardian of image quality. This process is also made smoother by robust healthcare system integrations that ensure patient data flows correctly from the scanner to the archives.
The image below shows the technical procedures that support the hands-on, patient-facing workflow.
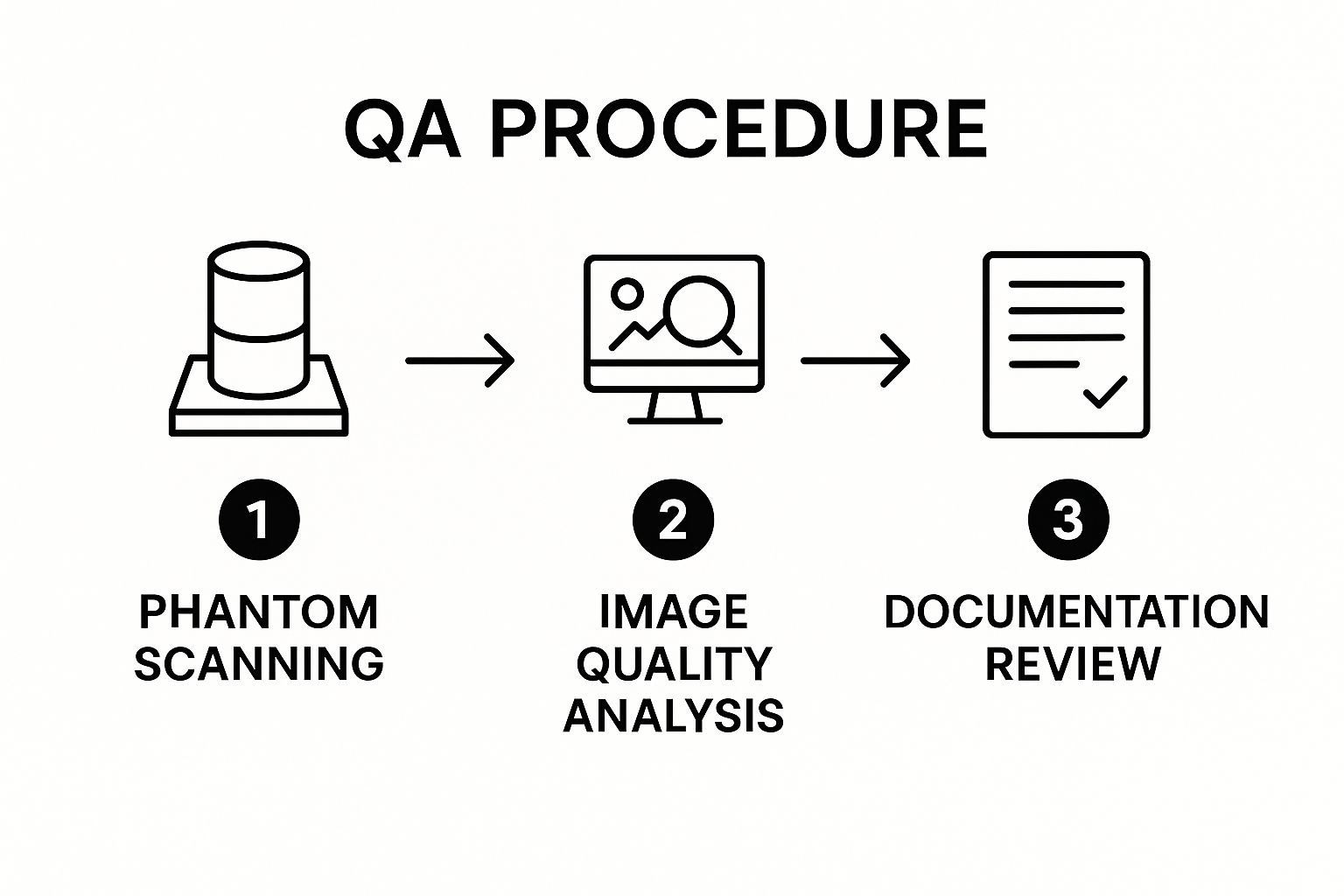
This cycle of phantom testing, analysis, and documentation is the technical backbone supporting every step of the patient's journey.
Post-Scan: The Final Verdict
The workflow concludes in the Post-Scan phase, after the images have been acquired. It starts with image processing, where technologists might apply special reconstructions to bring out more detail. From there, the images are sent to the Picture Archiving and Communication System (PACS).
This is where the radiologist performs the ultimate QA check. They meticulously review the entire study, judging its diagnostic quality. They check if the right area was scanned, if the resolution is sharp enough, and if any artifacts obscure their view. If a scan isn't up to par, they provide direct feedback to the technologist—a vital step for continuous improvement.
Only when the radiologist is fully satisfied with the image quality do they move on to interpretation and creating the final report. This final human review is the last, and arguably most important, checkpoint in the entire QA chain, ensuring clinical decisions are based on the most reliable visual evidence possible.
How AI Is Elevating Imaging Quality Assurance

Artificial intelligence isn't some far-off idea anymore—it's become a powerful partner in the quest for perfect medical images. In medical imaging quality assurance, AI is bringing a new level of precision and speed that simply wasn't possible before, acting as a tireless assistant to our human experts.
Think of it this way: AI is the ultimate QA co-pilot for technologists and radiologists. It takes over the tedious, repetitive quality checks, which frees up highly skilled professionals to focus on what they do best—tackling complex diagnostic problems and focusing on patient care. This blend of human expertise and machine precision is making the entire QA process faster, more consistent, and far more effective.
Automating Real-Time Quality Checks
One of the most significant ways AI is making a difference is by checking image quality in real time, right as the scan is happening. Algorithms trained on thousands of images can instantly analyze a scan and flag common problems that could otherwise compromise its diagnostic value.
For instance, AI can immediately spot issues like:
- Motion Artifacts: If a patient moves, even slightly, the AI flags the blurry image right away. This gives the technologist a chance to recapture it correctly on the spot.
- Image Noise: The system can evaluate the signal-to-noise ratio and alert the operator if it's too low for a clear diagnosis.
- Improper Positioning: AI tools are smart enough to know if a specific body part isn't centered correctly or fully included in the scan.
By catching these errors at the source, some AI software can even automatically reject a subpar scan before it ever gets sent to the PACS. It’s a proactive approach that dramatically cuts down on patient recalls, which means less unnecessary radiation exposure and less wasted time for everyone involved.
The Power of Predictive Maintenance
Beyond just looking at images, AI is also revolutionizing how we maintain the scanners themselves. Instead of waiting for a machine to break down, AI makes predictive maintenance a reality. It's like having a smart car that tells you the engine needs service weeks before you'd ever end up stranded on the side of the road.
AI systems continuously track subtle performance data from imaging equipment—tiny fluctuations that are often invisible to the human eye. By spotting patterns in this data over time, the algorithm can forecast when a specific part is likely to fail.
This shift from reactive repairs to proactive maintenance is a total game-changer. It minimizes unexpected downtime, a huge headache that leads to lost revenue and delayed patient care. An AI system might, for example, predict an X-ray tube is nearing the end of its life, allowing the facility to schedule a replacement during off-hours, avoiding any disruption.
The growth in this field has been huge. The market for medical imaging analytics software in North America alone jumped from USD 780.8 million in 2016 and is projected to hit USD 1.31 billion by 2025—a growth rate of over 67%. This boom shows just how much demand there is for tools that can automate error-spotting and optimize clinic workflows. You can discover more insights about medical imaging analytics on Market.us.
Enhancing Human Expertise, Not Replacing It
It’s really important to see AI's role for what it is: a tool to augment human experts, not replace them. The best systems are built on collaboration, where AI handles the high-volume, data-heavy tasks, and humans provide the final, critical judgment and nuanced oversight.
The FDA has already given the green light to hundreds of AI/ML-enabled medical devices, and about 75% of them are in radiology. This shows a strong acceptance from both regulators and clinicians. AI is incredibly good at spotting subtle patterns across massive datasets that a person might miss, presenting those findings to a radiologist or physicist for the final call. This teamwork makes the entire QA process smarter, faster, and ultimately, safer for patients.
Building a Bulletproof QA Program at Your Facility
Knowing the principles of quality assurance is one thing, but putting them into practice is where the real work begins. Creating a robust medical imaging quality assurance program isn’t about just buying the latest equipment. It’s about weaving a commitment to quality into the daily fabric of your facility. This all starts with getting the right people in a room and giving them clear ownership over every step of the imaging process.
The first move is to form a dedicated QA committee. Think of this group as the program's steering committee. It's usually headed by a lead radiologist or department manager and should include key players like medical physicists and senior technologists. Their primary job is to set the standards—the specific rules and protocols your facility will live by, making sure they align with guidelines from respected bodies like The American College of Radiology (ACR) and The Joint Commission.
This committee handles the practical decisions: choosing the right phantoms and software, setting a schedule for routine QC checks, and creating a clear plan for what to do when equipment acts up. Without this kind of organized leadership, QA efforts can easily become scattered and inconsistent, which defeats the whole purpose.
Cultivating a Culture of Quality
A truly great QA program is about more than just checklists and procedures; it’s fueled by a genuine culture of quality. This means changing how people think about QA—moving it from a "have-to-do" chore to a "want-to-do" shared mission for patient safety and diagnostic accuracy. Every single person on the team, from the front desk scheduler to the radiologist reading the final scan, needs to feel like they have a stake in the outcome.
So, how do you build this culture? It comes down to a few key actions:
- Be Open with Communication: Don't keep QA results a secret. Share performance data with the entire team. When things go well, celebrate it. When there are issues, discuss them openly as a group to find solutions, not to point fingers.
- Establish Feedback Loops: Create a straightforward way for radiologists to give helpful, constructive feedback to technologists about image quality. This is how everyone improves and adapts their technique.
- Invest in Your People: Set aside real time and budget for ongoing training. When your staff feels confident in their skills and supported by management, they become your biggest champions for quality.
A true culture of quality is when doing things the right way becomes the easiest and most natural way to work. It shifts QA from a top-down order into a collaborative effort that everyone owns and believes in.
Documentation and Regulatory Readiness
Finally, meticulous documentation is the spine of any QA program you can stand behind. Every test, every calibration, and every repair needs to be logged—no exceptions. This isn't just about being organized; it's a non-negotiable part of regulatory compliance and accreditation.
Think of your documentation as the official story of your commitment to quality. It’s the proof you need to show that you're consistently meeting safety standards and providing excellent care. When inspectors from The Joint Commission show up or it's time to renew your ACR accreditation, well-kept records are your best friend.
Your documentation process should be simple and standardized, capturing what was tested, who did the test, what the results were, and any steps taken to fix problems. These days, digital QA management software can handle much of this heavy lifting, keeping your records secure, easy to find, and always audit-ready. This diligent approach protects your facility, your team, and above all, your patients.
Frequently Asked Questions About Medical Imaging QA
When you start digging into the nuts and bolts of a quality assurance program, a lot of practical questions pop up. We’ve gathered some of the most common ones we hear to help clear things up for clinical teams striving for excellence in diagnostic imaging.
What Is the Difference Between Quality Assurance and Quality Control?
It’s easy to use these terms interchangeably, but they actually mean two very different things.
Think of Quality Assurance (QA) as the big-picture strategy. It’s the entire proactive system you build to prevent mistakes from ever happening. This includes everything from how you train your staff and set department policies to your documentation protocols. It’s the overall game plan for quality.
Quality Control (QC), on the other hand, is a specific part of that plan. It’s the hands-on testing you do on the equipment to make sure it’s working correctly. That daily phantom scan a technologist runs on a CT machine to check its calibration? That’s a perfect example of QC in action.
So, QA is the grand strategy for the whole operation, while QC is the tactical, on-the-ground testing that makes sure the strategy is working.
How Often Should Imaging Equipment Be Tested?
There’s no one-size-fits-all answer here. The right testing schedule really depends on the type of equipment, what the manufacturer recommends, and the rules set by regulatory bodies like the ACR.
That said, a typical schedule looks something like this:
- Daily or Weekly: These are the quick, basic QC checks. Technologists will handle things like verifying phantom image uniformity or checking laser alignment to catch any immediate issues.
- Annually or Semi-Annually: This is when the big guns come out. A qualified medical physicist or certified engineer performs a deep-dive evaluation. They test everything from radiation output to spatial resolution, ensuring the machine is safe and stable for the long haul.
What Are the Biggest Challenges in Implementing a QA Program?
The toughest roadblocks are usually less about the technology and more about people and processes. One of the most common issues is simply money—getting the budget approved for the right testing tools and software can be a struggle.
Another major hurdle is time. It’s hard to carve out dedicated hours for QA tasks when you’re dealing with a packed patient schedule.
Getting past these obstacles really comes down to getting strong support from leadership. You need their buy-in to secure the resources and to help build a culture where everyone sees quality as their personal responsibility. Consistent training is also key, so the entire team is on the same page and working to the same high standards.
If you have more questions, you can often find answers by looking at broader industry discussions, like these additional frequently asked questions.
AI is a powerful tool that augments, not replaces, human expertise. The ideal model is a partnership between AI efficiency and human critical thinking and oversight.
Can AI Replace the Need for Human-Led QA?
Not a chance. Think of AI as an incredibly smart assistant, not a replacement for the human expert.
AI is fantastic at handling the tedious, repetitive stuff. It can spot tiny patterns in data that a human might miss and can even predict when a machine might be about to fail. This frees up your technologists and physicists to focus on what they do best: complex problem-solving, strategic planning, and making those subtle clinical judgments that a machine just can’t handle.
At PYCAD, we build AI solutions that strengthen medical imaging workflows, not take them over. Our custom models are built to slide right into your existing QA program. They automate the boring checks and give your team the data-driven insights they need to work smarter. Find out how our AI services can help your facility take its commitment to quality and patient safety to the next level at https://pycad.co.