Understanding What Makes Medical Software Different
Building medical software isn't anything like creating your typical consumer app. If you're coming from a world of ride-sharing or social media platforms, you'll find the landscape here is completely different. The core reason? The stakes are incredibly high. A bug in a photo-sharing app might be an annoyance, but a flaw in medical software could pose a genuine risk to a patient's health.
This means the Silicon Valley mantra of "move fast and break things" gets thrown out the window. Instead, the guiding principle becomes "move deliberately and prove everything." It’s a fundamental shift in thinking that goes beyond just writing good code. It’s about building a system that is demonstrably safe, thoroughly documented, and ready to face intense examination by regulatory bodies.
Juggling a Unique Cast of Stakeholders
In most software projects, you're trying to keep users and business owners happy. With medical software, the room gets a lot more crowded. Picture a project meeting where you need to satisfy:
- A surgeon who needs instant access to a lot of data for quick, critical decisions.
- A hospital administrator who is laser-focused on liability and data privacy.
- An FDA auditor who meticulously checks every piece of documentation.
- An IT professional worried about how your new software will play with their ancient, existing systems.
Each of these stakeholders speaks a different language, has competing priorities, and measures success differently. For example, that surgeon's request for a data-heavy interface might be flagged by a human factors engineer. They'll argue that too much information at once can lead to cognitive overload and dangerous mistakes, particularly at the end of a 12-hour shift. The administrator, on the other hand, just wants to know if the software is fully compliant with HIPAA. Finding a balance between these conflicting needs is a central challenge in this field.
The Heavy Weight of Regulation and Risk
The level of regulation you'll face depends entirely on what your software does. A simple wellness app for tracking daily steps is a low-risk project with minimal oversight. However, software that controls a radiation therapy machine or helps diagnose conditions from an MRI scan is a different beast altogether. This is known as Software as a Medical Device (SaMD), and it's subject to strict government regulations.
For these high-risk applications, every decision has to be justified and documented—from the programming language you choose to the color of a button. You can’t just apply a standard agile development process off the shelf. Agile's focus on quick iteration can conflict with the need for detailed, upfront risk analysis and frozen, validated requirements. A "sprint" in this context might need to include formal verification steps not seen in other industries, often leading to a hybrid model that blends agile flexibility with waterfall's structure.
This detailed process is becoming more important as healthcare leans more on digital solutions. Looking ahead to 2025, a staggering 90% of health system executives expect virtual health to be a huge part of how they deliver care. This push requires software that can manage complex patient data and integrate smoothly with new technologies. To learn more about this trend, you can check out Deloitte's 2025 global health care outlook. This growth highlights why getting a handle on the unique demands of the medical software development process is more critical than ever.
Gathering Requirements Without Losing Your Mind
Kicking off any project with requirements gathering is always a delicate dance. For medical software, it's more like navigating a minefield while juggling chainsaws. Your stakeholders aren't just product owners; they're busy clinicians, risk-averse hospital administrators, and meticulous regulatory advisors. Getting this right isn’t just about listening—it’s about translating needs, anticipating unstated problems, and documenting everything with the precision of a legal proceeding.
One of the toughest parts is getting clear, usable information from medical professionals. A surgeon might say they need a dashboard to be "more intuitive," but what does that really mean? For them, it could mean having instant access to pre-operative imaging, patient vitals, and lab results all on one screen. For someone else, it might mean larger buttons that work with gloved hands in a sterile setting. You can’t build software on vague wishes; you have to dig deeper.
The Art of Clinical Translation
As a product manager or business analyst in this space, your role is to act as a translator between the clinical and technical worlds. This goes beyond just asking, "What do you want?" and requires a more investigative approach.
Here are a few techniques that have proven effective in real-world healthcare environments:
- Shadowing and Observation: Don't just rely on what you're told in meetings. Spend time watching clinicians in their element. Observe how they interact with current systems, notice their workarounds (those sticky notes on monitors are goldmines of hidden needs), and map out their actual workflow, not just the one they describe. You'll often discover critical requirements they wouldn't have thought to mention.
- Use-Case Scenarios: Instead of asking for a list of features, walk them through specific situations. For example: "A patient comes into the ER with symptoms X, Y, and Z. Using our proposed interface, show me every step you would take, from assessment to ordering tests." This anchors the discussion in reality and reveals important procedural details.
- Prototype and Iterate: A simple wireframe or an interactive prototype is worth a thousand meetings. Busy doctors can provide more valuable feedback in five minutes with a tangible mock-up than in an hour-long abstract discussion. This feedback loop is crucial for refining the user experience while keeping patient safety as the top priority.
To properly categorize the information you gather, it helps to understand the different types of requirements you'll encounter. Each one comes from a different source and has its own set of rules for documentation and validation.
Requirements Categories in Medical Software Development
Comparison of different requirement types, their sources, documentation needs, and validation approaches
| Requirement Type | Primary Source | Documentation Level | Validation Method | Regulatory Impact |
|---|---|---|---|---|
| Functional | End-users (clinicians), stakeholders | High (detailed in SRS) | Use-case testing, user acceptance testing (UAT) | High (directly impacts intended use) |
| Non-Functional | Technical team, administrators | Medium to High (performance, security) | Stress testing, security audits, performance benchmarks | High (impacts safety, security, and reliability) |
| Regulatory | FDA, MDR, ISO standards | Very High (requires traceability) | Audits, formal verification, compliance checks | Critical (non-compliance blocks market access) |
| User Experience (UX) | End-users, observation | Medium (wireframes, prototypes) | Usability testing, user feedback sessions | Medium (poor UX can introduce use-related risks) |
| Data | System integrations, legacy systems | High (data dictionaries, mapping) | Data integrity checks, validation rules testing | High (impacts patient data privacy and accuracy) |
This table shows that while a clinician's input is vital for functional needs, regulatory requirements from bodies like the FDA demand a much more formal and rigorous approach to documentation and validation.
Balancing User Wants with Regulatory Needs
In the world of medical software, the most convenient design isn't always the safest or most compliant one. A clinician might ask for a one-click process to prescribe medication to save time. From a safety and regulatory perspective, that’s a massive red flag. A compliant workflow might demand multiple verification steps, clear confirmations, and a detailed audit trail to prevent accidental overdoses or incorrect prescriptions.
This can create tension. The solution is to explain the "why" behind the constraints. Position regulatory rules not as bureaucratic obstacles, but as critical safety features designed to protect both the patient and the provider. Explaining that a two-step confirmation process is a safeguard against medication errors—a known patient safety risk—helps get buy-in from even the most time-crunched users.
The journey from an initial idea to a market-ready product is long, and every requirement must be prepared for it, as shown in the graphic below.
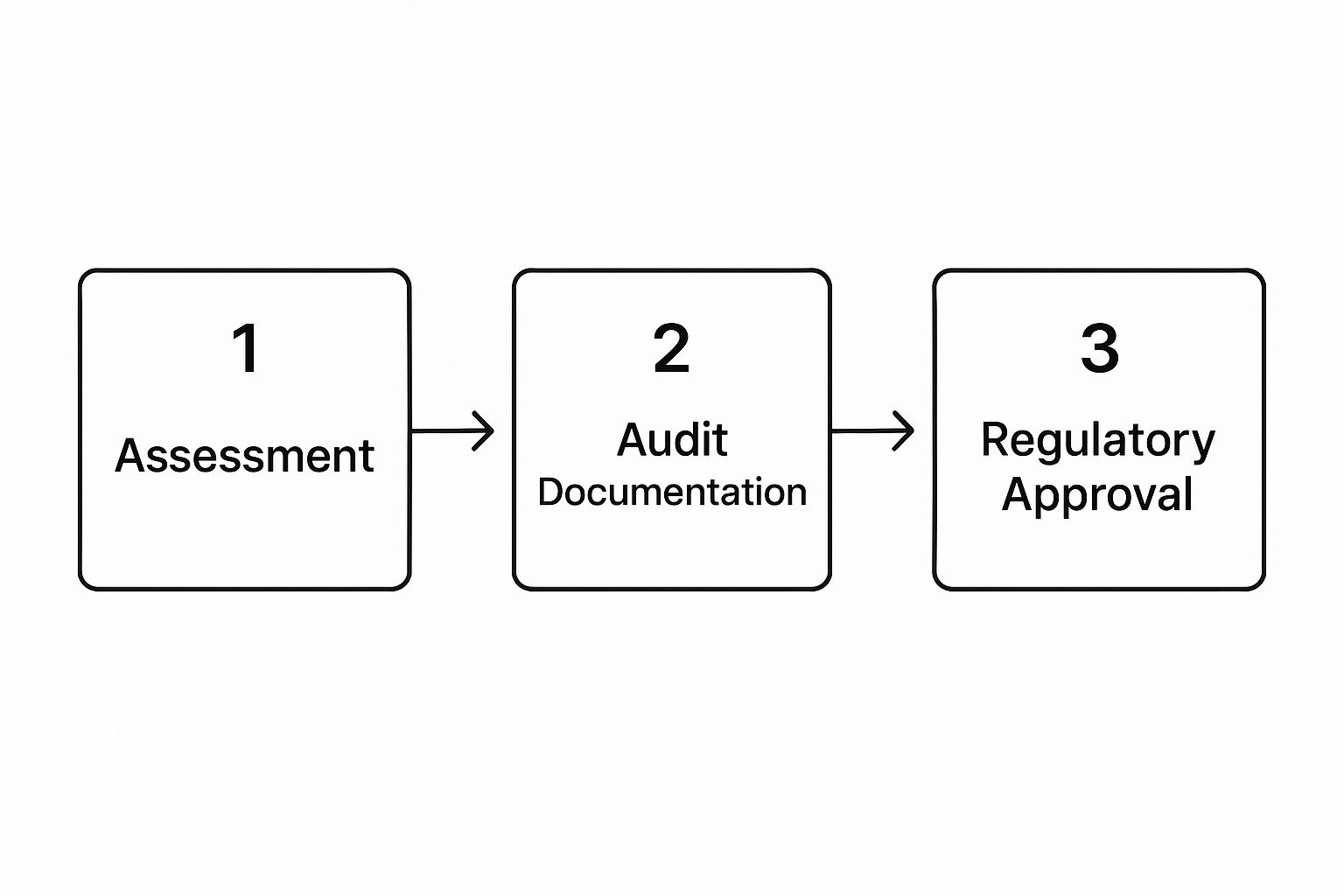
This visual makes it clear: every requirement collected during the assessment phase needs to be documented well enough to pass a formal audit before it can be considered for final approval.
Documenting for Two Audiences: Developers and Auditors
Your requirements documentation needs to satisfy two very different groups. Your development team needs clear, unambiguous technical specs to build the software correctly. Auditors, on the other hand, need proof of a controlled process, complete with risk analysis and traceability from start to finish.
A Software Requirements Specification (SRS) document is absolutely essential. It must carefully detail every functional, non-functional, and data requirement. Each requirement should have a unique identifier, which allows you to trace it from its origin, through development and testing, and all the way to the final validation report. This traceability is a cornerstone of regulatory compliance, proving you built exactly what you planned and tested every potential risk. This disciplined approach early on prevents major scope creep and expensive rework later, ensuring a smoother path through the demanding medical software development process.
Designing Interfaces That Keep Patients Safe

When you're designing medical software, you're not just making something that looks nice. You're building a tool that has to perform under intense pressure. Imagine designing an airplane cockpit—the user could be tired, stressed, and a single mistake can have serious consequences. This is why the best medical software teams see user interface (UI) and user experience (UX) design as a critical part of patient safety, not just an aesthetic choice.
Every single design decision needs to be thought out and justified. Your goal isn't just to create a pleasant workflow but to build a system that actively prevents errors. This is especially true for a clinician who might be using your software at the end of a demanding 12-hour shift. That’s where human factors engineering (HFE) comes in. It's the science of designing systems around human abilities and limitations, a foundational practice in the medical software development process.
Human Factors and Reducing Cognitive Load
The main objective of HFE in medical UI design is to cut down on cognitive load. An interface that’s cluttered with irrelevant information forces a healthcare professional to waste mental energy hunting for what they need instead of concentrating on their patient. For example, a poorly designed electronic health record (EHR) might show a patient's entire lab history all at once. A safer, more thoughtful design would highlight only the newest and most critical results, keeping older data accessible but out of the immediate view.
To build safer medical interfaces, you should focus on a few key principles:
- Clarity Above All: Labels should be clear and direct. While standard clinical terms are necessary for precision, avoid confusing jargon. A button that says "Discharge" is always better than one with a vague icon.
- Consistency is Key: Similar elements must behave the same way throughout the application. If a red alert indicates a critical warning in one part of the software, it must mean the same thing everywhere.
- Forgiveness in Design: Your design should have checks and balances to stop irreversible mistakes. Before a clinician confirms a high-dose medication order, the system should pop up a confirmation that clearly states the dose and its potential dangers.
Designing for the Real World: Beyond the Basics
Designing for medical settings means planning for the chaos of reality. A screen that looks great on your high-resolution monitor might be unreadable on a small tablet mounted on an IV pole in a dimly lit hospital room. Accessibility here goes beyond the usual web standards. It means using color-blind-friendly palettes for charts and high-contrast text that stays legible under harsh fluorescent lights.
A tragic real-world example involved an infusion pump with a confusing numeric keypad layout. A nurse, trying to enter "5.0," accidentally typed "50," resulting in a tenfold overdose. This event highlights how a seemingly small UI mistake can have devastating outcomes. It’s why every design choice, from button placement to font size, must be documented with a clear safety rationale to get through regulatory checks.
Because security is so vital for medical devices, building in strong development practices from the very beginning is a must. Integrating security during the design phase is key to protecting patient data and ensuring the system works as intended. You can learn more about embedding these practices by checking out DevSecOps best practices for secure software, which offers a solid framework for creating safer applications built for the healthcare environment.
Development Practices That Survive FDA Scrutiny

When you're writing code for a medical device, every single line is under a microscope. The objective isn't just to make something that works; it's to create a product that is provably safe and operates exactly as intended, every single time. This calls for a level of discipline that goes well beyond standard "clean code" principles. The medical software development process requires practices that can withstand the intense scrutiny of regulatory bodies like the FDA.
This reality is why the tools supporting this industry are growing so quickly. The global life science software market is a perfect example, projected to expand from $17.69 billion in 2025 to $36.25 billion by 2032. This growth is largely driven by medtech companies needing to improve their development and regulatory workflows. You can find more insights into the life science software industry to see how this trend highlights the absolute need for bulletproof development practices.
Coding Standards with a Clinical Focus
In regulated software, coding standards aren't just helpful suggestions—they're a core part of your risk mitigation strategy. General best practices like avoiding "magic numbers" and using clear variable names are a decent start, but medical-grade standards are far more rigorous. For example, your team needs strict, documented rules for error handling. A generic error message that’s fine in a consumer app could be a genuine safety risk in a clinical setting.
Your coding standards must also cover:
- Defensive Programming: You have to write code that can handle unexpected inputs and system states without failing. Always assume external data or user input might be incorrect or even malicious.
- Static Code Analysis: Integrate automated tools directly into your build process. These tools can enforce standards and catch problems like null pointer dereferences or resource leaks before the code even gets to a tester.
- Peer Review Rigor: Code reviews can't be casual. They must be formal, documented processes. Reviewers need to check for logic and style, but more importantly, for adherence to documented software requirements and risk controls.
Version Control and Traceability: An Auditor's Dream
Your version control system, like Git, is much more than a place to store code. It's a critical piece of your evidence for a regulatory submission. Auditors demand a clear, unbroken trail for every change made to the software. This means lazy commit messages like "fixed bug" are out of the question. A compliant commit message must reference the specific task, requirement, or bug ID from your project management system, such as Jira.
This concept of traceability is non-negotiable. An auditor must be able to pick any single requirement from your initial design documents and follow its entire journey. They need to see every commit related to it, review the tests that were run against it, and find the final validation results. This documented trail proves that you have a controlled and deliberate development process.
Because patient data is often involved, development practices must also account for things like secure HIPAA compliant document sharing to ensure all artifacts are handled safely. Maintaining this level of detail can feel like extra work, but it's exactly what makes regulatory reviews go smoothly.
Testing and Validation That Actually Proves Safety
When your medical software moves from development into testing, the entire game changes. In a typical software project, this phase is about hunting down bugs to make sure everything works as planned. But for medical software, the stakes are infinitely higher. You’re not just fixing glitches; you’re building a mountain of evidence to prove your software will not cause harm, no matter the circumstances. Every test case, validation script, and document must be crafted to demonstrate safety and effectiveness to regulatory bodies.
This intense validation is crucial, especially as software becomes more deeply integrated with physical medical devices. The medical device industry is a massive, expanding market. In 2025, it's projected to hit $678.88 billion, with a steady growth of 6%. Software is the intelligence behind countless devices, from diagnostic imaging tools to instruments for minimally invasive surgery. This tight link between hardware and software is why a "good enough" testing approach is a non-starter. You can explore more about the medical device industry's growth on arterexmedical.com to understand the scale we're talking about.
Designing Test Cases for Regulatory Eyes
You need to create your test plans for two very different audiences: your internal quality assurance team and the external regulatory reviewer. The reviewer isn't just checking to see if your software works; they want to see how you proved it’s safe. This calls for a risk-based testing approach. Instead of giving every feature equal attention, you must prioritize based on the risk analysis you completed earlier. Any function tied to a high-risk activity—like calculating a medication dose or controlling a surgical laser—needs exhaustive testing that covers every conceivable edge case.
For example, imagine your software helps a radiologist measure a tumor. Your test cases must go beyond the ideal scenario and include:
- Perfect, high-resolution images.
- Blurry, low-contrast images.
- Images that contain digital artifacts.
- Scenarios where a user tries to measure an object that isn't a tumor.
- Instances where a user inputs nonsensical calibration data.
Each test must be explicitly linked back to a specific requirement and a specific risk. This traceability is the bedrock of your validation documentation and is absolutely non-negotiable.
From Unit Tests to Full Clinical Simulation
Validating medical software is a multi-layered effort. It starts with the smallest piece of code and expands to encompass the entire system running in a simulated real-world environment.
-
Unit and Integration Testing: At the code level, developers run unit tests that do more than check basic logic. For a software module that controls a physical infusion pump, tests must simulate hardware failures, communication drops, and power interruptions. Integration tests then confirm that these individual units work together correctly and reliably.
-
System Validation: This is where you test the complete, assembled software. It’s not enough to run it on a pristine lab server; you have to mimic the chaotic, unpredictable clinical setting. This includes performance testing to ensure the system responds instantly when seconds matter and security testing to protect sensitive Protected Health Information (PHI).
-
User Acceptance Testing (UAT): This is the ultimate validation step. You put the software in the hands of the people who will actually use it—doctors, nurses, and technicians. They follow predefined clinical scenarios to confirm the software is not just functional but also safe and intuitive in practice. A feature that seems perfectly logical to a developer might be confusing or error-prone for a nurse in a high-stress situation. UAT feedback is priceless for catching these use-related hazards before the software goes live.
To help visualize how these testing stages connect to regulatory requirements, the table below breaks down each phase, its goals, and the documentation needed.
| Testing Phase | Primary Objective | Key Activities | Documentation Required | Regulatory Milestone |
|---|---|---|---|---|
| Unit Testing | Verify individual code components work as designed. | Isolate and test small code units (functions, methods) for logic, errors, and boundary conditions. | Unit Test Plan, Unit Test Cases, Code Coverage Reports. | Foundational evidence of code quality for internal review. |
| Integration Testing | Ensure different software modules interact correctly. | Combine and test units to check data flow, communication, and interface integrity. | Integration Test Plan, Integration Test Reports, Defect Logs. | Demonstrates system components work together as specified. |
| System Testing | Validate the entire system against its requirements. | Test the fully integrated software in a controlled, simulated environment. Includes performance, security, and stress testing. | System Test Protocol, Traceability Matrix, System Test Report. | Key evidence for V&V (Verification and Validation) submission. |
| User Acceptance Testing (UAT) | Confirm the software is safe and effective for its intended users and use environment. | Real clinicians perform tasks based on clinical workflows. Gathers feedback on usability and safety in practice. | UAT Plan, UAT Scenarios, User Feedback Forms, Usability Engineering Report. | Critical input for Human Factors Engineering (HFE) and final validation reports for regulatory approval. |
This table shows that each testing phase builds upon the last, creating a comprehensive evidence trail. From the smallest code unit to a full clinical simulation, every step is designed to prove the software is ready for the real world.
Carefully documenting these phases is just as critical as running the tests. Your final validation report isn’t just a summary; it's the complete, undeniable case that proves your software meets its intended use safely and effectively. This body of evidence is what will ultimately determine if your product gets the green light from regulators.
Getting Through Regulatory Approval Without Going Insane
The journey through regulatory approval can feel like entering a mysterious maze where the walls constantly shift. For many teams in the medical software development process, this phase represents the final, most intimidating hurdle. But it doesn't have to be a black box that consumes your budget and timeline. With the right strategy, you can get through this complex environment methodically and predictably.

This screenshot from the FDA's website gives a glimpse into the structured pathways available for medical devices, including software. The key takeaway here is that regulatory bodies don't use a one-size-fits-all approach; your path depends heavily on your software's risk classification.
Choosing Your Regulatory Pathway
The first, and most critical, decision is selecting the correct regulatory pathway. This choice is dictated by your software's intended use and the level of risk it poses to patients. Is your software a simple wellness app (low risk), or does it actively diagnose disease or control a therapeutic device (high risk)? Getting this wrong can lead to rejection and force you to restart a multi-year process.
For instance, in the U.S., you might be looking at one of these common FDA pathways:
- 510(k) Premarket Notification: This is the most common route. You must demonstrate that your software is "substantially equivalent" to a legally marketed device that is already on the market (a predicate device). This requires meticulous documentation comparing your software's features, performance, and safety against the predicate.
- Premarket Approval (PMA): This is the most stringent pathway, reserved for high-risk, life-sustaining, or novel devices for which no predicate exists. A PMA requires you to provide valid scientific evidence, often from clinical trials, proving your software's safety and effectiveness.
Each pathway has vastly different requirements for data, documentation, and cost. A 510(k) submission might take months to review, whereas a PMA can easily take over a year. Making the right choice upfront saves an immense amount of time and resources.
Preparing Documentation That Gets Approved
Once your path is set, the real work of assembling your submission begins. Regulatory reviewers are looking for a clear, logical story that proves you have a controlled process. Your documentation isn't just a collection of files; it's a comprehensive argument for your software's safety.
A common mistake is submitting documentation that is disorganized or incomplete. This almost guarantees a long series of questions and requests for additional information (AIs) from the agency, adding months to your timeline. Your submission file should be so well-organized that a reviewer can easily trace any requirement from its conception through design, coding, testing, and final validation.
Navigating the complex world of digital regulations and compliance is a key challenge for medical software; insights from experts in the field can be incredibly helpful. It’s also crucial to remember that different global markets, like the EU with its Medical Device Regulation (MDR), have their own distinct requirements. If you plan to launch internationally, your documentation strategy must account for these variations from day one. By treating regulatory approval as an integral part of development, not an afterthought, you can turn a potentially chaotic process into a manageable, and ultimately successful, part of your journey.
Your Practical Action Plan for Medical Software Success
Let's move from theory to a concrete roadmap you can actually use. Successfully navigating the medical software development process is about being proactive, not reactive. This takes more than good intentions; it requires solid strategies, an eye for warning signs, and a team that understands the unique pressures of healthcare tech.
Assembling Your A-Team and Cultivating the Right Culture
Your first move is building the right team, and it’s about more than just hiring skilled developers. A winning medical software project needs a mix of experts from the very beginning, including clinical specialists, regulatory advisors, and human factors engineers. These aren't just consultants you call in later; they should be core team members shaping the product from its earliest days.
A strong partnership with clinicians is especially important. You need professionals who get your technical goals but also understand your budget. Look for a clinical champion—a doctor or nurse who is genuinely passionate about the project's success. They will be your connection to the realities of a clinical setting, helping to turn user needs into clear requirements and giving essential feedback.
The culture you build is just as important as the people you hire. It needs to find a balance between creating new solutions and a serious commitment to safety. This means every single person on the team, from a junior developer to the project manager, knows that patient safety is the number one priority. This mindset shapes everything from code reviews to design choices, building a strong foundation that will hold up under regulatory review.
Budgeting, Timelines, and Staying the Course
Budgeting for medical software involves specific costs that are easy to miss. Beyond salaries, you have to plan for:
- Regulatory Submissions: The fees for filing with bodies like the FDA or for Notified Body reviews in the EU can be significant.
- Quality Management System (QMS): Putting a compliant QMS in place and keeping it running requires specific tools and dedicated staff.
- Prolonged Validation: The deep testing and validation cycles take much more time and money than in other industries.
Project timelines are often a marathon, not a sprint. A realistic timeline for a moderately complex medical device can be 18-36 months from idea to market approval. Keeping the team motivated over these long periods is a real challenge. Make sure to celebrate the small wins, like passing a phase review or getting great feedback from usability studies, to keep spirits high.
Post-Market Responsibilities and Sustainable Compliance
Getting regulatory clearance isn't the end of the road. You must have a solid plan for post-market surveillance. This means you're actively watching how your software performs in the real world, gathering user feedback, and tracking any negative events.
Handling software updates is another key post-launch task. While not every bug fix or new feature needs a full re-submission to regulators, you need a documented process to evaluate the impact of every change. A small tweak to the user interface might seem minor, but if it could confuse a user and lead to a mistake, regulators might see it as a major change. Creating sustainable practices for ongoing compliance allows you to improve your product without getting stuck in unnecessary regulatory loops.
At PYCAD, we specialize in building the AI engine that drives next-generation medical software. We manage the complex data and model development, so you can focus on delivering safe, effective, and compliant medical solutions. Find out how our expertise can speed up your project at PYCAD.co.






