At its core, operational efficiency in healthcare is all about making the most of what you have. Think of it as a strategic puzzle: how do you arrange all your pieces—your skilled staff, your expensive medical equipment, your limited hospital beds—to deliver the absolute best patient care without breaking the bank?
It’s the key to improving patient outcomes while keeping the lights on and ensuring the organization can thrive for years to come.
Why Operational Efficiency in Healthcare Matters Now
Picture a bustling city's traffic system during rush hour. A single breakdown can trigger a chain reaction, causing gridlock and frustration for miles. A modern hospital is just as complex, but the stakes are infinitely higher. That's why the push for operational efficiency in healthcare has moved from a "nice-to-have" business goal to an absolute necessity for survival.
This isn't happening in a vacuum. Healthcare providers are caught in a perfect storm of rising costs, soaring patient expectations, and staggering levels of staff burnout. In this environment, the old mantra of "just work harder" is not only unsustainable, it's dangerous. The only path forward is to work smarter by fine-tuning every single process and workflow.
The Financial and Human Cost of Inefficiency
Inefficiency isn't just a line item on a budget report; it has real, tangible costs. For instance, something as seemingly simple as underused medical equipment can quietly drain a hospital of over $12,000 per bed every single year. These aren't just abstract numbers. They represent wasted funds that could have been poured back into life-saving technology, hiring more nurses, or creating a better healing environment for patients.
The true cost of inefficiency goes far beyond the balance sheet. It puts an immense strain on your team, tanks morale, and, most critically, can directly compromise patient health and safety.
When your systems are clunky and inefficient, nurses get bogged down in paperwork instead of being at the bedside. Patients face agonizingly long waits for diagnoses or treatments. It’s a frustrating reality that underscores just how urgently we need a smarter, more systematic way of delivering care.
To truly grasp the scope of operational efficiency, it helps to break it down into its core components. Each pillar represents a critical area where focused improvements can lead to significant gains across the entire organization.
Core Pillars of Healthcare Operational Efficiency
| Pillar | Description | Key Goal |
|---|---|---|
| Process Optimization | Analyzing and redesigning clinical and administrative workflows to eliminate waste, reduce steps, and remove bottlenecks. | To create smooth, fast, and error-free pathways for patient care and administrative tasks. |
| Resource Management | Effectively allocating and managing key assets like staff, equipment, operating rooms, and hospital beds. | To maximize the use of every resource, ensuring they are available when and where they are needed most. |
| Financial Stewardship | Managing costs, controlling budgets, and optimizing revenue cycles without compromising the quality of care. | To ensure the long-term financial health and sustainability of the healthcare organization. |
| Patient Flow & Experience | Managing the patient's journey from admission to discharge to ensure it is timely, safe, and positive. | To reduce wait times, improve communication, and enhance overall patient satisfaction. |
| Technology Integration | Implementing and integrating digital tools—from EHRs to AI—to automate tasks and provide data for better decision-making. | To empower staff with the right tools to work more effectively and make informed choices. |
By focusing on these five pillars, healthcare leaders can build a comprehensive strategy that addresses inefficiency from every angle, creating a stronger and more resilient organization.
A Global Push for Modernization
This isn't just a local problem; it's a challenge healthcare leaders are grappling with all over the world. A recent Deloitte survey of global C-suite executives revealed that over 70% identified improving operational efficiency and productivity as a top priority. This global consensus points to a massive, coordinated effort to drag healthcare operations into the 21st century, moving away from outdated manual workflows and—believe it or not—the still-too-common fax machine.
Ultimately, getting this right creates a powerful, positive feedback loop. Greater operational efficiency in healthcare directly leads to:
- Better Patient Outcomes: When processes are smooth, the risk of medical errors drops and patients get the care they need, right when they need it.
- Improved Staff Satisfaction: Freeing clinicians from administrative drudgery allows them to reconnect with their core mission: caring for patients.
- Enhanced Financial Stability: Making the most of every dollar and resource is the bedrock of long-term organizational health.
Pinpointing Common Hospital Operational Bottlenecks

To truly improve operational efficiency in healthcare, leaders have to get good at spotting the hidden friction that slows everything to a crawl. These operational bottlenecks aren't just minor annoyances. They are deep-seated issues that drain money, burn out staff, and directly compromise how quickly and effectively patients get treated.
Picture these bottlenecks as dams in a river. They block the natural flow, causing pressure to build up upstream while leaving other areas completely dry. Finding these dams is the essential first step to breaking them down and getting the current moving smoothly again.
Uncoordinated Patient Flow and Discharge Delays
One of the most common and maddening bottlenecks is a choppy, unpredictable patient flow. This isn’t just about the long waits in the emergency room; it’s a problem that follows the patient throughout their entire stay. The classic example? The discharge process. A patient is medically cleared to leave but ends up stuck in their room for hours.
What’s behind this holdup? Usually, it's a chain reaction of communication breakdowns. The doctor’s discharge order doesn't get to the nurse right away, the pharmacy takes too long to prepare take-home prescriptions, and nobody tells the transport team they’re needed. The immediate result is a tied-up bed that another patient—often in the ER—is waiting for, which triggers a domino effect of delays across the hospital.
Underutilized Assets and Clumsy Scheduling
Operating rooms (ORs) and high-tech imaging machines are huge capital investments. Yet, it's surprisingly common to see them sitting idle because of poor scheduling. An OR might go dark for a couple of hours between surgeries simply because of a coordination mix-up or a last-minute cancellation that no one managed to backfill.
This isn't just inefficient; it's lost revenue and a longer wait for the next person who needs a procedure. Fine-tuning how these critical assets are scheduled is one of the most direct ways to improve both the financial bottom line and patient access to care.
An operational bottleneck isn't just a process flaw; it's a direct barrier to delivering timely, effective care. It transforms a well-intentioned system into a source of frustration for both patients and the clinical staff trying to help them.
The Crushing Weight of Administrative Tasks
Maybe the most universal bottleneck of all is the mountain of administrative work that steals clinicians away from their real jobs. We see it every day: nurses and doctors bogged down in charting, coding, and piles of paperwork, which means less time spent with patients.
This administrative burden is a massive source of waste. In the U.S. alone, administrative tasks make up about 25% of all healthcare spending. Worse, studies show that nearly 30% of that figure is pure waste from inefficiency. This amounts to hundreds of billions in lost dollars every year—a compelling reason to find smarter ways to handle these behind-the-scenes processes. You can dig deeper into this by reviewing the path forward for mobilizing data for operational efficiency.
How to Measure Healthcare Efficiency Effectively

You can't improve what you don't measure. It’s an old saying, but it’s the absolute truth in healthcare. The diagram above, from Wikipedia, perfectly illustrates how efficiency isn't just about saving money; it's a core component of overall quality, sitting right alongside patient safety, equity, and effectiveness. To actually improve operational efficiency in healthcare, leaders need a solid set of Key Performance Indicators (KPIs) that give a clear, honest look at what’s working and what’s not.
Think of these KPIs as the gauges in a pilot's cockpit. Each one provides vital feedback on a different system, helping you steer the entire organization in the right direction. Flying without them is just guesswork.
The best KPIs aren't just numbers on a screen; they're strategic tools. The secret is to align your chosen metrics directly with your hospital's specific goals, turning raw data into a real plan for improvement.
Choosing the right metrics is everything. A hospital struggling with a crowded ER will focus on different KPIs than a facility trying to make its surgical department more profitable. It has to match the mission.
Patient-Focused Efficiency Metrics
These KPIs are all about seeing efficiency through the patient’s eyes. They track the patient's journey, giving you critical insight into their experience.
-
Average Length of Stay (ALOS): This is the average number of days a patient is admitted. When a patient can go home sooner (and safely), it usually means care was well-coordinated, resources were used wisely, and the discharge process was smooth.
-
Door-to-Doctor Time: A classic emergency department metric, this tracks the time from when a patient walks in the door to when they are first seen by a physician. It's a direct reflection of your front-end workflow and ER responsiveness.
Resource-Based Efficiency Metrics
These indicators measure how well a facility is managing its most expensive and crucial assets: its beds, operating rooms, and high-tech equipment.
-
Bed Occupancy Rate: This is the percentage of your staffed beds currently in use. While a high number might look good, a rate that’s consistently over 85% can be a red flag. It often means you have no flexibility for patient surges, which leads to ER diversions and bottlenecks throughout the hospital.
-
Operating Room Utilization: This measures how much of your scheduled OR time is actually used for surgery. Getting this number up is one of the most direct ways to boost surgical volume and, by extension, revenue.
Financial and Cost-Based Metrics
At the end of the day, a hospital is also a business that needs to remain financially healthy. These metrics tie operational performance directly to the bottom line.
-
Cost per Discharge: This calculates the average total cost of care for a patient’s entire stay. It gives you a bird's-eye view of how effectively your teams are using resources—from staffing to supplies—to deliver care.
-
Revenue per Bed: This KPI tells you how much revenue each of your available beds is generating. It helps you see which service lines are most productive and where you might need to reallocate resources for a better financial return.
By tracking a smart mix of metrics from all three categories, you create a balanced scorecard for your organization. This gives you a complete picture of performance, allowing you to make decisions that not only improve efficiency but also enhance patient care and secure your hospital's long-term financial stability.
Proven Strategies for Boosting Operational Performance
Once you've pinpointed where the snags are, the real work begins. It's time to put proven strategies into practice to boost operational efficiency in healthcare. These aren't just ideas from a textbook; they are field-tested approaches that deliver tangible results for your patients, your staff, and your budget.
The aim here is to systematically break down the barriers that slow things down and create more predictable, reliable workflows. A fantastic framework for this is Lean Healthcare. At its core, Lean is all about relentlessly finding and getting rid of "waste"—which is anything in a process that doesn't directly add value from the patient's perspective. Think unnecessary waiting, redundant paperwork, or even just walking across the hospital to find a piece of equipment.
Adopting a Lean mindset means you start looking at the entire patient journey with fresh eyes. You map it all out, from the first phone call to schedule an appointment all the way through to discharge, and you question every single step. Where do delays crop up? Where does information get dropped? Cutting out these wasteful steps doesn't just speed up care; it dramatically cuts down on the potential for errors.
Embrace Technology and Automation
Some of the most direct and powerful improvements today come from smart technology. Automation, especially, can completely change the game for both administrative and clinical tasks that have traditionally been manual and time-consuming.
- Telehealth Integration: This is so much more than just a video call. When used strategically, telehealth helps balance the patient load across your entire system. It allows you to see more people, handle follow-ups without needing an in-person visit, and provide crucial care to patients who can't easily travel. All of this happens without putting more physical strain on your facilities.
- Workflow Automation: Think about all the routine administrative work that happens every day. So much of it can be automated. Implementing effective document workflow management can drastically cut the time spent manually shuffling patient records, billing forms, and compliance documents. This frees up your highly skilled staff to focus on what they do best: patient care.
A culture of continuous improvement is the engine of operational excellence. It transforms efficiency from a one-time project into an ongoing organizational mindset, empowering every team member to be a problem-solver.
Foster a Culture of Continuous Improvement
At the end of the day, your most powerful asset in fixing inefficiencies is your frontline staff. They are the ones who live with the bottlenecks every single day. If you want to make real, lasting change, you have to build a culture where their feedback isn't just accepted—it's actively sought out.
This means creating straightforward ways for staff to report problems without any fear of blame. It's about empowering individual departments to try out new ideas on a small scale, see what works, and then celebrate those wins. When your nurses, technicians, and administrators feel like they own a piece of the improvement process, they become an incredible source of practical, innovative solutions.
When you combine this kind of culture with smart technology and proven methods like Lean, you create a flywheel of positive change. Small, consistent improvements build on each other, eventually leading to huge, sustainable gains in operational efficiency in healthcare. It's this comprehensive approach that gets every part of the organization working together to deliver care that is faster, safer, and more affordable.
The Role of AI in Modern Healthcare Operations

Artificial Intelligence is no longer some far-off concept—it’s a real, practical tool that's solving some of medicine's most stubborn operational headaches. Think of it as a powerful partner for healthcare providers, automating the tedious work and predicting future needs so doctors and nurses can make smarter decisions.
This isn't about replacing human experts. It's about augmenting them. AI handles the heavy lifting of data analysis and repetitive tasks, freeing up clinicians to focus on what only they can do: provide compassionate, direct patient care.
From Predicting Patient Surges to Automating Paperwork
One of the most impactful uses of AI is in predictive analytics. Imagine an advanced early warning system for your hospital. AI models can sift through years of patient data, local health trends, and even things like weather forecasts to predict when the emergency room is about to get slammed. This foresight allows hospitals to adjust staffing and prepare resources before a crisis, turning a potential chaotic scramble into a calm, managed response.
Then there's the administrative side. We all know that medical coding, billing, and processing insurance claims are huge time sinks, not to mention they're filled with opportunities for human error. AI-powered systems can handle these tasks with incredible speed and accuracy, freeing up countless staff hours that can be put to better use.
Artificial Intelligence is quickly becoming the backbone of operational efficiency in healthcare. Its ability to find meaningful patterns in massive datasets gives us a clear path to smarter resource management and better workflows.
This isn't just theory; the data backs it up. A recent analysis found a direct, statistically significant link between AI-driven management systems and operational efficiency, quantified with a coefficient of 0.525. Put simply, better AI systems lead to a substantial boost in how smoothly a facility runs. The study also highlighted an indirect benefit: these systems improve staff attitudes, which in turn creates a more productive workplace.
Making Smarter Decisions, From the Clinic to the Front Office
AI's value goes well beyond simple automation. It actively sharpens decision-making at every level. In the clinic, AI tools can help analyze complex medical images—like the kind our team at PYCAD works with—to flag potential abnormalities for a radiologist's expert review. Administratively, it can optimize operating room schedules to ensure they are used to their full potential, minimizing expensive downtime.
The table below shows how different AI applications tackle specific operational problems.
AI Applications for Healthcare Efficiency
| AI Application | Operational Challenge Addressed | Potential Impact |
|---|---|---|
| Predictive Patient Flow Analytics | Unexpected surges in ERs and clinics | Proactive staffing, reduced wait times, better resource allocation. |
| Automated Medical Coding & Billing | Time-consuming, error-prone administrative tasks | Faster revenue cycles, fewer claim denials, freed-up staff time. |
| AI-Powered Image Analysis | Radiologist burnout and diagnostic delays | Quicker, more accurate preliminary findings; faster report turnaround. |
| Smart Operating Room Scheduling | Inefficient OR utilization and costly downtime | Maximized surgical throughput, reduced patient backlogs. |
These examples are just the beginning. To really get the most out of these tools, it helps to understand the technology that makes it all possible. Exploring the latest advances in data infrastructure and AI reveals how these foundational pieces support such powerful applications.
By bringing AI into their daily operations, healthcare organizations aren't just getting more efficient. They're building a smarter, more responsive system for everyone.
Your Questions on Healthcare Efficiency Answered
Diving into a project to improve operational efficiency in healthcare can feel overwhelming. I've seen countless healthcare leaders ask the same practical questions: Where do we even start? How do we get our team on board? What results can we realistically expect?
Let's cut through the noise and tackle these common questions with clear, straightforward answers to help you get moving.
Where Is the Best Place to Start Improving Efficiency?
The best place to start is almost always with a persistent, nagging problem you can clearly see and control. For most hospitals and clinics, that problem is patient flow.
Begin by mapping out the entire patient journey for a specific, high-volume service. Think about a routine surgical procedure or an emergency department visit. Follow the patient step-by-step and look for the obvious friction points and delays. Is there a long wait between a patient's arrival and their first chat with a clinician? Does the discharge process grind to a halt for hours? These aren't just minor annoyances; they're giant red flags signaling a broken process.
Tackling a highly visible and frustrating bottleneck first, like patient wait times, can deliver a quick, impactful win. This early success builds crucial momentum and makes it easier to get buy-in for more ambitious, system-wide changes down the line.
Once you’ve zeroed in on a major bottleneck, put all your initial energy there. Solving one significant problem creates a tangible victory that proves the value of these efforts to your entire team.
This infographic breaks down what you can expect from these kinds of focused projects.
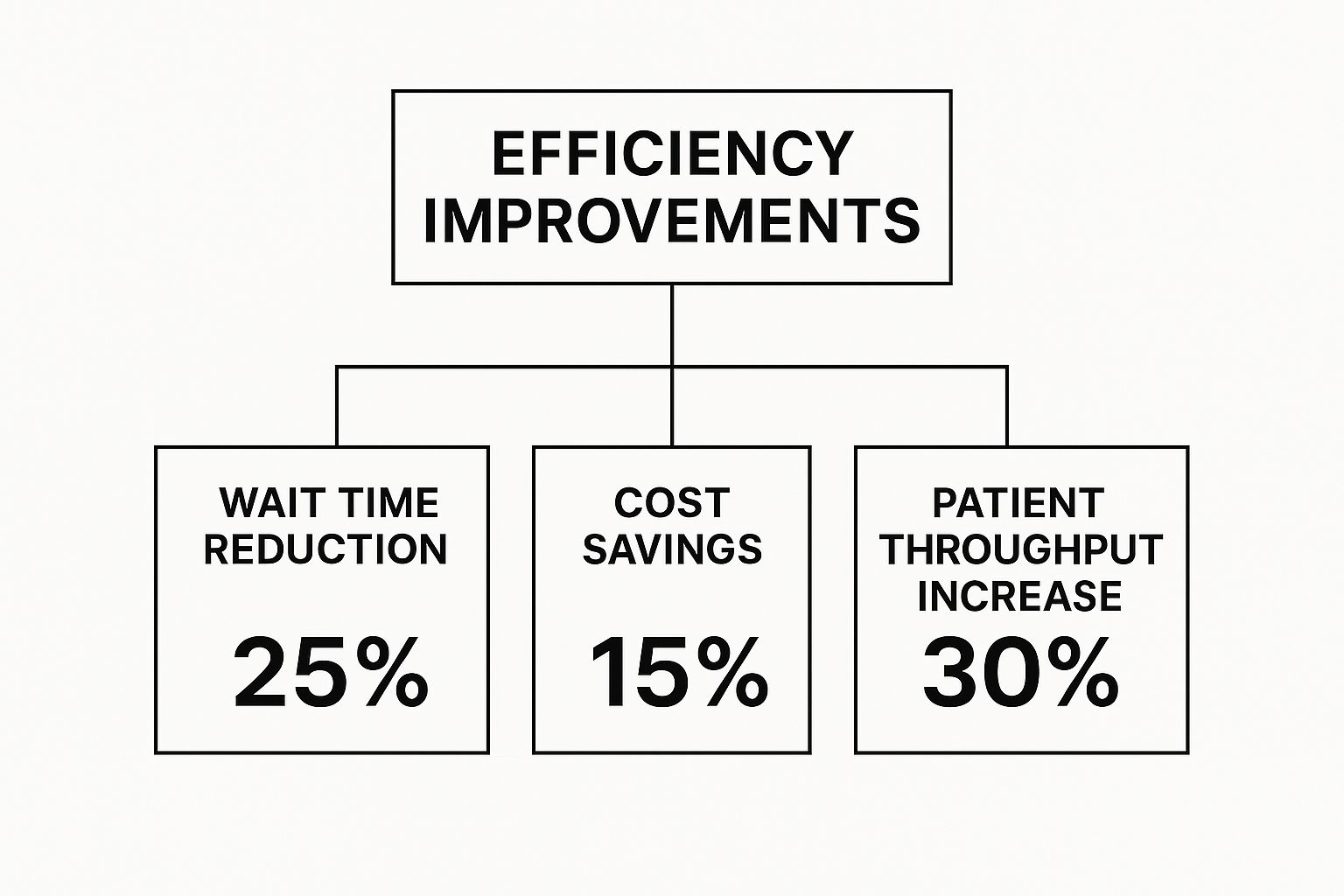
As you can see, targeted improvements often lead to big wins, like a 30% increase in patient throughput and a 25% reduction in wait times.
How Can We Get Staff to Support New Processes?
Honestly, getting your staff on board is the single most important part of this whole equation. Change is hard, and clinicians are rightfully skeptical of new initiatives that look like more work on their already full plates.
The secret is to frame efficiency not as a top-down order, but as a team effort to make their jobs easier.
Here’s how you build that support from the ground up:
- Involve Them Immediately: Bring your frontline staff—the nurses, doctors, techs, and admins—into the conversation from day one. They live these problems every day and are your best source for practical, real-world solutions.
- Focus on “What’s In It for Them”: Show them exactly how a new process will reduce their daily headaches. Will a new digital workflow get rid of that mountain of paperwork? Will better scheduling stop last-minute staffing scrambles? Connect the dots for them.
- Run Small Pilot Programs: Forget a massive, hospital-wide rollout. Test the new process in a single, receptive department first. This lets you iron out the kinks on a small scale and creates a group of internal champions who can vouch for the benefits.
- Listen and Adapt: Actively ask for feedback during and after the pilot. When your staff sees that you're actually listening to their concerns and acting on their suggestions, they'll go from being passive observers to active partners.
What Is a Realistic ROI for Efficiency Projects?
The return on investment from improving operational efficiency in healthcare isn't just about money. A realistic ROI is a mix of financial, clinical, and human returns.
- Financial Returns: This is the most obvious one. You’ll see cost savings from better resource management (like lower overtime pay thanks to smart staffing), less supply waste, and more revenue from higher patient throughput—think getting more out of your operating rooms.
- Clinical Quality Returns: This is all about patient safety and better outcomes. A successful project might lead to a measurable drop in hospital-acquired infections, fewer medication errors, or faster door-to-doctor times. The value here is immense.
- Human Capital Returns: Never underestimate the impact on your staff. When you reduce administrative burdens and burnout, you get lower staff turnover—a huge cost saving in itself—along with better morale and a more engaged team.
While the exact numbers will vary, it's not uncommon for well-run projects to deliver cost savings of 10-20% in the targeted area within the first 12-18 months.
At PYCAD, we focus on AI-powered medical imaging solutions that directly improve diagnostic accuracy and boost operational efficiency. To see how our technology can help you fine-tune your clinical workflows and achieve better patient outcomes, explore our services.






