Tackling Today's Radiology Workflow Challenges
Modern radiology departments are facing increasing complexity. The sheer volume of imaging requests continues to climb, while staffing shortages persist. This creates immense pressure to deliver faster turnaround times. The strain on existing resources is palpable, pushing traditional workflows to their limits. Many departments are struggling to meet current demands, underscoring the critical need for radiology workflow optimization.
Increased imaging volume often creates bottlenecks in image interpretation. These backlogs can delay critical diagnoses and negatively impact patient care. Staff shortages compound the problem, placing a heavier burden on existing personnel and increasing the risk of burnout. Departments must find ways to accomplish more with fewer resources, requiring a fundamental shift in their operational strategies.
Another major contributor to workflow inefficiency is the constant barrage of interruptions. These disruptions fracture focus and reduce productivity for both radiologists and technologists. A 2025 study highlighted just how pervasive these interruptions are. Researchers analyzed over 39,000 electronic messages related to CT scan requests within a single academic radiology practice. They discovered that staff received an average of 4.2 messages per hour – totaling over 100 per day. This constant influx of communication significantly impacts their ability to concentrate. For a more detailed breakdown of these statistics, see this helpful resource: Top Reasons for Radiology Workflow Interruptions and How to Address Them
Simply acknowledging these challenges isn't enough. Departments must actively identify their specific bottlenecks to implement effective, targeted solutions. This requires an honest internal assessment and a willingness to embrace change and adapt. Forward-thinking departments are already proactively addressing these issues to improve their overall efficiency.
Identifying Key Bottlenecks
Improving workflow begins with pinpointing the root causes of inefficiency. This involves a thorough analysis of every step in the imaging process, from initial order entry to final report delivery. Common areas where bottlenecks frequently occur include:
- Patient Scheduling and Registration: Inefficient scheduling can lead to delays and wasted time for both patients and staff.
- Image Acquisition: Technical issues or outdated equipment can significantly slow down the imaging process.
- Image Interpretation: Backlogs in image reading can delay diagnoses and impact treatment decisions.
- Report Generation and Distribution: Manual report creation and distribution are often time-consuming and prone to errors.
- Communication: Poor communication between staff, radiologists, and referring physicians can create confusion and hinder workflow.
By identifying these specific bottlenecks, radiology departments can develop focused strategies for improvement. This targeted approach ensures that resources are allocated effectively, maximizing the impact of implemented solutions and paving the way for a more efficient and effective workflow.
The Cost of Inefficiency
Inefficient workflows have far-reaching consequences that extend beyond simply impacting turnaround times. They also affect staff satisfaction and, most importantly, patient care. Burnout among overworked staff can lead to decreased morale and higher turnover rates. This further strains resources and creates a self-perpetuating cycle of inefficiency. For patients, delays in diagnosis and treatment can cause increased anxiety and potentially worsen health outcomes. The financial implications are also substantial, as inefficient processes often lead to increased costs and decreased revenue.
Therefore, radiology workflow optimization is not merely about increasing efficiency; it's about enhancing the quality of care. By addressing workflow challenges, departments can cultivate a more positive work environment for staff, improve patient experiences, and bolster the financial well-being of the organization. This creates a ripple effect, driving positive change across the healthcare system.
How AI Is Revolutionizing Radiology Operations
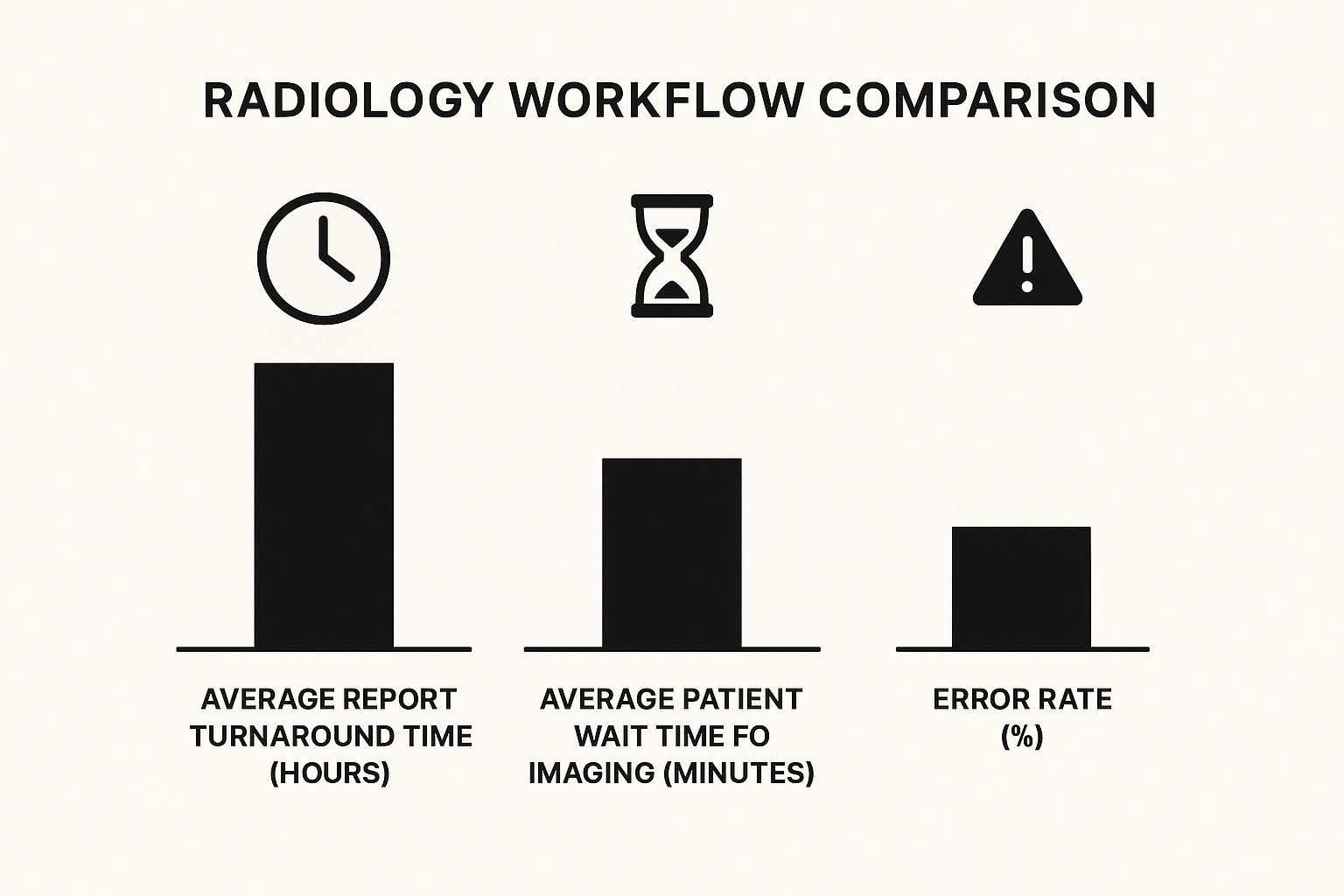
The infographic above visualizes AI's impact on key radiology workflow metrics: average report turnaround time, patient wait time for imaging, and the error rate. Improvements in these areas translate directly to improved patient care and more efficient resource use. Faster turnaround times, shorter patient waits, and a dramatic reduction in errors are all key benefits of AI integration.
Artificial intelligence is reshaping how radiology departments operate. AI-powered solutions deliver measurable results, addressing challenges faced by modern radiology departments. Intelligent image routing, for example, eliminates manual sorting by automatically directing images to the appropriate specialist. This significantly speeds up the diagnostic process and reduces potential delays.
Predictive analytics is another valuable AI tool. By identifying workflow bottlenecks before they cause disruptions, predictive analytics enables proactive intervention. This helps create smoother, more predictable workflows and minimizes delays.
Automating Administrative Tasks
One of AI's most significant contributions to radiology is automating routine administrative tasks. AI algorithms can now handle tasks like data entry, image sorting, and report prioritization. This frees up radiologists and other staff to focus on more complex diagnostic challenges requiring their expertise.
Automating these tasks also reduces the risk of manual errors, enhancing the accuracy and reliability of information. This precision and timeliness are crucial for patient care. This shift allows radiologists to dedicate more time to analyzing images and providing accurate diagnoses.
The following table summarizes the benefits of various AI technologies in a typical radiology workflow:
AI Technology Benefits in Radiology Workflow
Comparison of different AI technologies and their specific impact on workflow efficiency metrics
| AI Technology | Primary Function | Efficiency Improvement | Implementation Timeline |
|---|---|---|---|
| Intelligent Image Routing | Automates image distribution to specialists | Reduces turnaround time by up to 20% | Short-term (6-12 months) |
| Predictive Analytics | Forecasts workflow bottlenecks | Minimizes delays by up to 15% | Mid-term (12-18 months) |
| AI-Powered Diagnostic Support | Aids in image analysis and anomaly detection | Improves diagnostic accuracy by up to 10% | Long-term (18-24 months) |
This table highlights how different AI technologies can be implemented to achieve specific efficiency gains within a defined timeframe. Strategic implementation of AI offers a clear path towards optimizing radiology operations. Applying principles from automation in software development can further enhance the efficiency of these processes.
This shift in focus has led to improved turnaround times, giving radiologists quick access to crucial patient data, critical for prompt diagnosis and treatment. These improvements directly impact patient satisfaction, as patients experience shorter wait times and more efficient care. The market for AI in radiology workflow optimization is growing rapidly, fueled by this automation of routine tasks. It’s projected to reach US$4.93 billion by 2029, growing at a CAGR of 32.56% from 2024. Learn more about AI adoption in radiology.
AI-Powered Diagnostic Support
Beyond administrative tasks, AI plays an increasingly important role in diagnostic support. AI algorithms analyze medical images to identify patterns and anomalies that might be missed by the human eye. This improves diagnostic accuracy and helps radiologists make more informed decisions.
This added layer of analysis is particularly valuable in complex cases or when dealing with large volumes of images. AI-powered tools also assist with time-consuming tasks like image segmentation and 3D reconstruction, which often require specialized expertise. This assistance further streamlines the workflow and frees up radiologists for other important tasks.
These advancements are transforming radiology operations and contributing to improved patient outcomes. By enhancing diagnostic accuracy and streamlining workflows, AI plays a crucial role in delivering better patient care.
Essential Tools That Actually Make A Difference

Beyond the frequent discussions surrounding AI, several practical tools can significantly enhance the efficiency of your radiology workflow. These tools offer tangible advantages without necessitating substantial financial investments. This article explores cloud-based image access systems, smart routing technologies, and integration solutions, examining how these tools can work effectively with your existing PACS and RIS infrastructure. These tools address common pain points in radiology, eliminating time-consuming manual processes and facilitating improved communication with referring physicians.
Cloud-Based Image Access
Cloud-based image access systems provide numerous benefits for optimizing radiology workflows. Radiologists gain secure access to images from any location with an internet connection, enabling greater flexibility for remote consultations and work. Cloud storage also minimizes the need for on-site servers, which reduces physical space requirements and lowers IT infrastructure costs. This enhanced accessibility streamlines collaboration and ensures critical information is readily available when needed.
Cloud-based systems also offer improved disaster recovery capabilities and data redundancy, ensuring data integrity and business continuity in unforeseen circumstances.
Smart Routing Technologies
Smart routing technologies represent another valuable toolset. They automatically direct imaging studies to the appropriate specialist based on several criteria, including modality, body part, and urgency. This automation eliminates manual sorting and prioritization of studies, significantly saving time and minimizing the risk of delays. The automated routing process ensures that studies are promptly reviewed by the appropriate expert, enhancing overall efficiency. This contributes to faster turnaround times, allowing radiologists to focus their expertise on interpreting images and providing timely diagnoses.
Integration Solutions
Integration solutions seamlessly connect disparate systems, like PACS and RIS, within a radiology department. By enabling effective communication between these systems, integration tools streamline data flow and remove the need for manual data entry. This integration not only saves valuable time but also reduces the potential for errors associated with manual data transfer.
As reported in May 2025, integrated tools, incorporating features like cloud-based image access, smart image routing, and seamless PACS/RIS integration, have demonstrably reduced manual steps by up to 40% in some implementations. This improvement translates to shorter patient wait times and more effective utilization of radiologists’ expertise. Find more detailed statistics here.
Cost-Effective Solutions for All
Optimizing radiology workflows doesn't necessitate a complete system overhaul. Numerous cost-effective solutions integrate smoothly with existing infrastructure. These tools are scalable and adaptable, catering to departments of all sizes, from small clinics to large hospitals. This scalability allows for a phased implementation approach, enabling departments to begin with a smaller scope and expand as their needs evolve.
Implementation Strategies and Measurable Benefits
Successfully implementing new tools requires a strategic approach, considering factors such as budget, staffing, and existing technologies. Effective implementation often emphasizes staff training and ongoing support to maximize tool adoption. The measurable benefits of these tools include reduced turnaround times, enhanced communication, and increased staff satisfaction, ultimately contributing to improved patient care and outcomes.
While some tools provide immediate value, others require a longer-term commitment to fully realize their potential. Understanding this distinction is crucial when selecting and implementing tools. By prioritizing tools that align with their specific needs and resources, radiology departments can maximize their return on investment and achieve their workflow optimization goals.
Building Communication Systems That Protect Focus Time
Constant interruptions can drastically reduce productivity and negatively affect team morale. This section explores practical strategies that successful radiology departments utilize to minimize disruptive communication while ensuring crucial information gets to the right people at the right time. This delicate balance is the key to radiology workflow optimization.
Establishing Communication Protocols
Effective radiology workflow optimization depends significantly on well-defined communication channels. Creating clear organizational protocols is the first step in directing messages effectively. By sorting messages according to urgency and content type, departments can ensure that critical information takes precedence, while less urgent messages are handled appropriately.
This organized method helps to reduce the continuous stream of interruptions that can break concentration. For example, a system for flagging urgent requests enables immediate action. Routine communications, on the other hand, can be addressed during scheduled times.
This prioritization is essential for managing urgent tasks while still preserving focused work periods.
Implementing Communication Windows
Designated communication windows help preserve valuable focused work time. By scheduling specific times for routine communication and updates, radiology departments cultivate an environment that allows staff to concentrate on essential tasks. These dedicated windows also make communication itself more efficient.
During these designated times, staff can fully focus on addressing messages and working together productively. This structured approach boosts both productivity and concentration. It guarantees dedicated time for focused work, leading to greater efficiency and minimizing distractions that obstruct radiology workflow optimization.
Creating Escalation Pathways
Even with the best systems in place, urgent issues will still arise. This is why reliable escalation pathways are crucial. These pathways ensure urgent matters are addressed quickly and efficiently. Well-defined protocols for escalating critical issues to the right personnel guarantee fast response times.
These protocols should outline specific procedures for different levels of urgency, including relevant contact information and clear lines of decision-making authority. This level of preparation allows for swift action in critical situations, preventing potential delays and negative repercussions.
These pathways are vital for both patient safety and efficient radiology workflow optimization, enabling rapid response without disrupting the overall workflow.
Technology Solutions for Streamlined Communication
A range of technology solutions can help streamline communication workflows. Secure messaging platforms, task management software, and integrated communication systems all play an important role in radiology workflow optimization. These tools promote seamless communication between staff, radiologists, and referring physicians, making sure everyone has the information they need.
For example, a secure messaging platform enables direct communication with specialists while maintaining patient confidentiality. Task management software aids in monitoring progress and assigning responsibilities, fostering accountability and efficient follow-through. These technological solutions enhance communication and boost overall workflow efficiency.
Real-world examples show these strategies in action. Departments implementing these methods have reported significant decreases in interruptions without compromising patient care. They have seen improvements in report turnaround times, less staff stress, and higher overall satisfaction. These real results highlight the tangible benefits of streamlined communication systems. For further information on productive meetings and enhanced communication, resources such as this family meeting agenda offer valuable insights. By combining these strategies—prioritizing communication, protecting focus, and utilizing technology—radiology departments can create a more productive and less stressful work environment, greatly contributing to radiology workflow optimization.
Measuring What Matters: Workflow Success Metrics

Optimizing radiology workflows isn't a one-time fix; it's an ongoing process. It demands careful monitoring and measurement to ensure improvements are sustained and continue to evolve with the needs of the department. This section delves into the Key Performance Indicators (KPIs) that offer the most valuable insights for tracking workflow efficiency, covering everything from turnaround times and throughput to quality measures and staff satisfaction. These metrics provide the bedrock for data-driven decisions in radiology workflow optimization.
Establishing Baseline Measurements
Before making any changes, it's essential to understand where you stand. Establishing a baseline of your current performance provides that critical starting point. This baseline serves as a benchmark against which the impact of any radiology workflow optimization initiatives can be measured. By tracking specific metrics, departments can accurately assess the effectiveness of changes implemented over time. This data-driven approach guarantees that solutions deliver tangible results and contribute to continual improvement.
Setting Realistic Improvement Targets
With a baseline in place, the next logical step is defining realistic improvement targets. These targets should adhere to the SMART criteria: Specific, Measurable, Achievable, Relevant, and Time-bound. For instance, a department could aim to reduce report turnaround time by 15% within six months. These clearly defined goals provide teams with a concrete objective and a framework for evaluating success. Open communication is paramount; consider using a structured approach like a family meeting agenda to discuss targets and ensure team buy-in.
Implementing Monitoring Systems
For sustained radiology workflow optimization, implementing robust monitoring systems is vital. These systems should go beyond simply presenting raw data; they must offer actionable insights. This requires regularly tracking data and presenting it in a format that empowers informed decision-making. Regular analysis of these data points enables departments to identify emerging trends, detect potential problems early, and adapt workflow processes as needed. This iterative process helps maintain progress toward optimization goals.
Advanced Analytics for Workflow Optimization
Advanced analytics can unlock a deeper understanding of workflow patterns. These approaches help pinpoint hidden inefficiencies and forecast future capacity needs. By examining historical data, predictive models can anticipate workload fluctuations, allowing departments to proactively allocate resources. This promotes efficient staffing and prevents bottlenecks that can disrupt workflow. Data analysis also plays a key role in optimizing resource allocation to maximize efficiency and minimize waste.
Data-Driven Decision Making for Continuous Improvement
Leading radiology departments leverage data-driven decision-making to continually refine their processes. By tracking key metrics and analyzing workflow data, departments gain valuable insights that shape their strategies. This creates a feedback loop, helping departments anticipate challenges, adapt to changing demands, and maintain a competitive edge in the evolving healthcare environment. Maintaining a focus on staff satisfaction ensures teams remain engaged and motivated to contribute to ongoing radiology workflow optimization.
Key Metrics for Tracking Workflow Efficiency
Several key metrics are crucial for effectively tracking workflow efficiency in radiology:
- Report Turnaround Time: This metric measures the time from exam completion to the availability of the final report.
- Throughput: This refers to the number of patients or studies completed within a given timeframe.
- Error Rate: This is the percentage of reports or procedures requiring correction.
- Patient Wait Times: This measures the time patients spend waiting for exams or results.
- Staff Satisfaction: These are measures of employee morale and job satisfaction within the department.
These metrics offer a holistic view of workflow performance, enabling departments to monitor progress and identify areas for improvement.
To illustrate these key metrics and their target ranges, we've compiled the following table:
Critical Workflow Optimization KPIs
Essential metrics for measuring radiology workflow efficiency and their target improvement ranges
| KPI Category | Specific Metric | Baseline Range | Optimized Target | Measurement Frequency |
|---|---|---|---|---|
| Timeliness | Report Turnaround Time | 24-48 hours | <24 hours | Daily/Weekly |
| Volume | Examinations per Radiologist | 50-75 per day | 75-100 per day | Daily/Weekly |
| Quality | Error Rate | 2-5% | <2% | Monthly/Quarterly |
| Patient Experience | Patient Wait Time | 30-60 minutes | <30 minutes | Daily/Weekly |
| Staff Satisfaction | Employee Turnover Rate | 10-15% | <10% | Annually |
By diligently monitoring these KPIs and striving towards established improvement targets, radiology departments can successfully implement radiology workflow optimization strategies, leading to a more efficient, effective, and satisfying experience for everyone involved.
Key Takeaways For Radiology Workflow Success
This section offers a practical guide to optimizing radiology workflows. We'll cover effective strategies, warning signs, and realistic success metrics from departments that have successfully improved their operations. This includes practical checklists, achievable goals for different department sizes, and honest perspectives on what truly matters when resources are limited. Each takeaway focuses on actionable steps you can take immediately, with clear indicators to track progress and acknowledge successes. We'll examine which changes offer quick wins and which require a longer-term strategy, plus how to maintain momentum for continuous improvement.
Focus on Quick Wins for Early Momentum
Some changes bring immediate improvements, providing quick wins that motivate your team. For example, implementing standardized protocols for image acquisition or improving patient scheduling can greatly reduce delays. Streamlining communication with a secure messaging system can be another quick win. These early successes build momentum and encourage acceptance for more complex optimization projects. For instance, a department could potentially reduce patient wait times by 10% in the first three months simply by standardizing patient arrival procedures.
Prioritize Communication for Smooth Operations
Effective communication is essential for successful radiology workflow optimization. Establishing designated communication channels and timelines minimizes interruptions during focused work periods. Regular meetings, daily huddles, or specific "communication windows" can preserve valuable focus time for radiologists. A system for escalating urgent issues ensures these matters are addressed quickly without disrupting the overall workflow. One example would be dedicating certain times each day for handling routine requests, freeing up the rest of the day for focused work.
Utilize Technology Strategically
Technology is crucial in radiology workflow optimization. Consider tools like cloud-based PACS systems for better image access, smart routing solutions for efficient image direction, and integrated communication platforms. However, technology implementation needs to align with your department's specific needs and resources. Start by identifying your biggest bottlenecks and then choose the technologies that best address those specific issues. For instance, if a department is struggling with image interpretation backlogs, they might prioritize AI-powered diagnostic support tools.
Data-Driven Decisions for Continuous Improvement
Tracking key metrics is essential to evaluate the effectiveness of optimization efforts. Monitor metrics like report turnaround times, throughput, error rates, and patient wait times. Regularly review this data to identify trends and areas needing improvement. Advanced analytics can help anticipate capacity needs and optimize resource allocation. For example, a department might find that image acquisition delays frequently happen on particular days, allowing them to proactively adjust staffing.
Build a Culture of Continuous Improvement
Radiology workflow optimization is a continuous journey. Cultivate a culture of ongoing improvement. Regularly seek feedback from staff and address their concerns. Celebrate successes and recognize team contributions. This promotes ownership and encourages staff to contribute to the optimization process. This could involve using a suggestion box or holding regular team meetings to gather feedback about workflow issues and potential solutions.
Achievable Goals Based on Department Size
Realistic optimization goals should match your department's size and resources. Smaller departments might concentrate on improving existing processes and using basic technology, while larger departments could explore more advanced AI-powered solutions. No matter the size, prioritizing impactful changes and recognizing accomplishments is critical. For instance, a small clinic might initially focus on streamlining communication, while a larger hospital might invest in a department-wide PACS upgrade.
Honest Perspectives on Limited Resources
When resources are constrained, focus on maximizing the impact of existing tools and staff. Prioritize changes that address the most critical workflow challenges. Small, incremental changes can significantly improve efficiency over time. For instance, a department with a tight budget might use free or low-cost communication tools instead of expensive software.
Ready to improve your radiology workflow with AI? PYCAD specializes in integrating artificial intelligence into medical imaging, offering solutions to optimize medical devices for improved diagnostic accuracy and operational efficiency. From data handling and model training to seamless deployment, PYCAD provides comprehensive support for your radiology needs. Visit PYCAD to discover how their AI-powered solutions can improve your radiology operations.






