Think of medical imaging software as the brain behind the brawn of an MRI or CT scanner. The machine itself is a marvel of engineering, but it's the software that translates the raw, complex data it captures into something a doctor can actually use to see what's happening inside your body.
The Digital Darkroom of Modern Medicine
At its heart, medical imaging software is the essential link between a high-tech scanner and a doctor's diagnosis. Hospitals generate an enormous amount of data every year, and a staggering 80% of it is medical images. Without sophisticated software, that information would be a jumble of digital noise.
It’s more than just a fancy picture viewer. Imagine a professional photography studio. The scanner is the camera, capturing the raw image data. The software is the digital darkroom where that image is developed, processed, and enhanced. It allows radiologists to zoom in, adjust contrast, and manipulate the view to uncover subtle details that might otherwise be missed.
From Scan Data to a Clear Diagnosis
The path from a patient scan to a treatment plan involves a series of crucial steps, all managed by specialized software modules working together. These systems aren't just for looking at pictures; they create a connected workflow for analysis, storage, and collaboration.
The main jobs of this software are to:
- Capture and Organize: First, it has to grab the image data from all sorts of different machines and get it into a standard format. The universal language for this is DICOM (Digital Imaging and Communications in Medicine).
- Store and Manage: Next, it securely archives these massive files in a way that lets doctors pull up a patient's entire imaging history in seconds, from anywhere in the hospital. This system is often called a PACS (Picture Archiving and Communication System).
- Analyze and Interpret: This is where the magic happens. The software gives radiologists a powerful toolkit to measure tumors, highlight potential fractures, and compare a new scan to a previous one to see how a condition is progressing.
- Share and Report: Finally, it makes it easy to share these findings with the referring physician and other specialists, ensuring everyone involved in a patient's care is on the same page.
This whole process ensures a patient's imaging record tells a clear, continuous story, not just a collection of random files.
Medical imaging software does more than just display images—it transforms abstract data into a visual story of a patient's health. It gives clinicians the power to see what the naked eye can't, turning pixels into life-saving answers.
As scanners get more powerful—capturing incredible 3D and even 4D (time-based) images—the software has to keep up. Handling these incredibly complex datasets requires serious computing power and smart algorithms. In this guide, we'll dive deeper into how these digital engines work, see how AI is changing the game, and look at what's next for medical diagnostics.
Understanding the Core Components
To really get a handle on how software in medical imaging changes patient care, you have to look under the hood at its essential building blocks. These aren't just separate programs; they're interconnected systems that create a seamless digital workflow, from the moment a scan is ordered to the final diagnostic report. Each piece has a specific job, and they all work together like a well-oiled machine.
Think of it like a sophisticated diagnostic assembly line. Raw data from scanners goes in one end, and a clear, actionable clinical insight comes out the other. The software is what manages every single step of that journey, ensuring the data is secure, accessible, and ready for deep analysis.
This kind of integrated environment is absolutely critical for managing the sheer volume of data hospitals produce. On average, a hospital generates 50 petabytes of data every year, and a staggering 80% of that comes from medical images. You need a robust and specialized setup to handle that.
At the heart of any modern medical imaging department are three key pieces of software working in concert. Let's break down what they are and what they do.
Core Modules of Medical Imaging Software
To make sense of this ecosystem, it helps to think of each component in terms of a real-world analogy. The table below breaks down these core modules, their primary function, and a simple way to understand their role in the bigger picture.
| Module Name | Primary Function | Analogy |
|---|---|---|
| PACS | Stores, retrieves, and archives all medical images. | The high-security digital library. |
| RIS | Manages the entire radiology department's workflow. | The department's air traffic controller. |
| Image Processing Software | Provides tools for viewing, manipulating, and analyzing images. | The analyst's advanced digital toolkit. |
Together, these three pillars—storage, workflow, and analysis—form the foundation of modern diagnostic imaging. They create a powerful system that turns raw data from sophisticated hardware into a tool for saving lives.
PACS: The Digital Library
The Picture Archiving and Communication System (PACS) is the heart of medical imaging storage. Think of it as a massive, high-security digital library built specifically for medical images. Its main job is to safely store and retrieve every single X-ray, CT scan, and MRI taken across a healthcare network.
Gone are the days of radiologists hunting for physical film in a dusty archive. With PACS, they get instant access to a patient's entire imaging history with just a few clicks. This immediate access is crucial for comparing new scans with old ones to track how a disease is progressing or to see if a treatment is working.
RIS: The Command Center
While PACS handles the images, the Radiology Information System (RIS) manages the whole radiology department’s workflow. If PACS is the library, RIS is the air traffic controller, coordinating every operational detail from start to finish.
This system takes care of the essential tasks that keep a busy department running smoothly, including:
- Patient Scheduling: Managing appointments for all the different imaging machines.
- Billing Information: Tracking services performed for accurate financial processing.
- Reporting: Giving radiologists a platform to dictate or type up their findings.
By integrating perfectly with PACS, the RIS makes sure the right images are always linked to the right patient records, schedules, and reports. This connection minimizes errors and keeps things moving.
Image Processing Software: The Analyst's Toolkit
The final core component is the image processing software itself. This is the radiologist's advanced digital toolkit, where raw data from a scan becomes a detailed diagnostic map. These tools let specialists manipulate and analyze images in ways that were once impossible.
This is where a simple scan is transformed into a life-saving diagnosis. The software empowers clinicians to see beyond the pixels, uncovering subtle patterns and precise measurements that guide critical treatment decisions.
The infographic below illustrates how different imaging modalities all feed into this complex software ecosystem. It really drives home the central role that data management and analysis play.
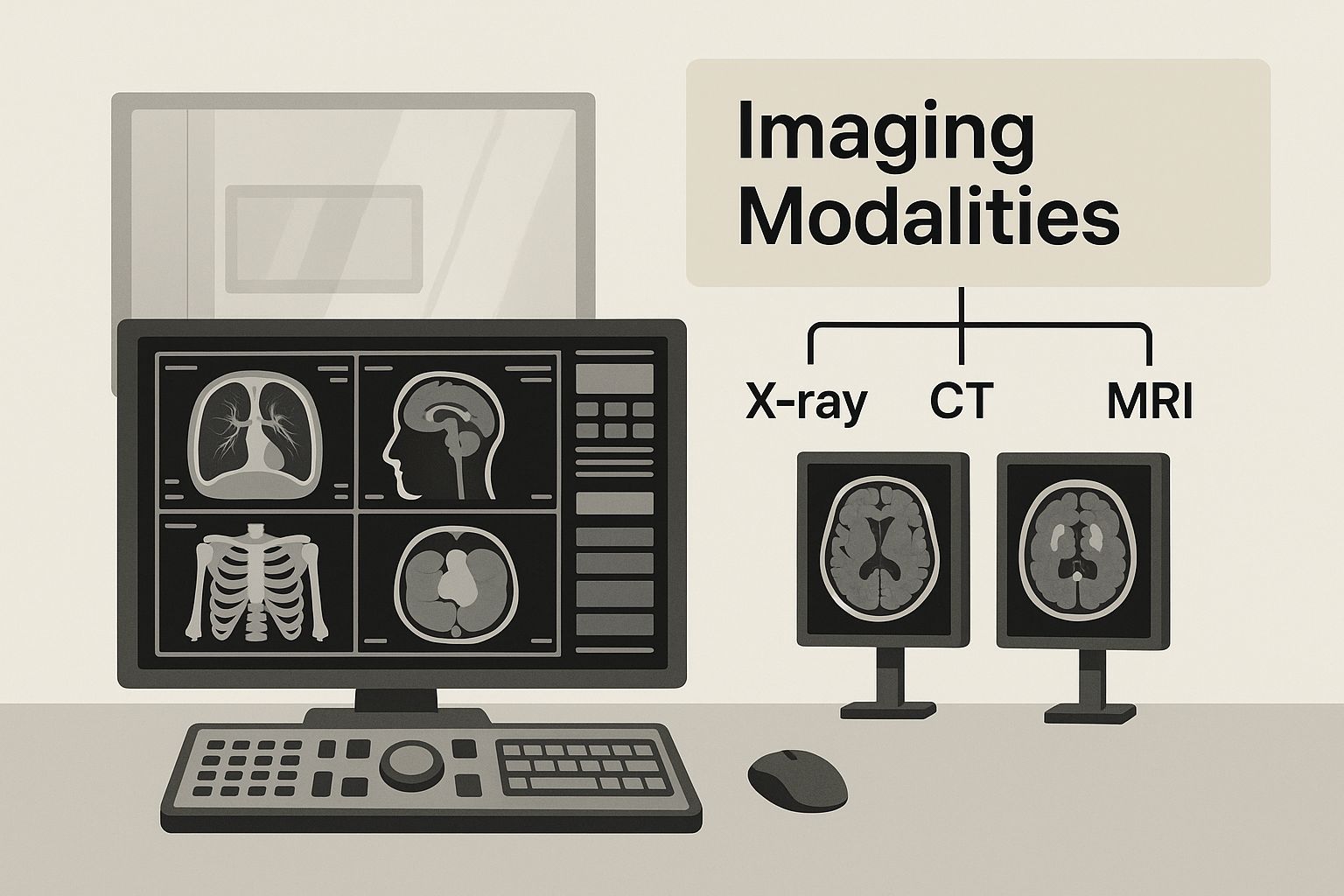
As you can see, it’s all about creating a cohesive control room where data from MRI, CT, and other scanners comes together. Everything is managed through a central software interface, an integrated approach that has become the cornerstone of modern radiology.
The demand for these powerful systems is growing fast. The global medical imaging software market was valued at around USD 7.6 billion in a recent year and is expected to hit USD 13.93 billion by 2033. According to insights from Straits Research, this growth is fueled by the increasing need to manage chronic diseases and serve an aging population.
How AI Is Revolutionizing Medical Imaging
Artificial intelligence isn't some far-off idea in healthcare—it's here now, and it’s completely changing the game in diagnostics. When AI is integrated into medical imaging software, it acts like an incredibly skilled co-pilot for radiologists. It handles the routine, tedious work and uncovers insights that the human eye might miss, truly shifting how clinicians approach complex scans.
Think of an AI algorithm as a tireless assistant with laser focus. It can meticulously measure tumor growth across hundreds of scans, a job that's not only time-consuming for a person but also susceptible to tiny errors. By taking over these repetitive tasks, AI gives specialists back their most valuable resource: time. This allows them to focus their expertise on the most challenging cases that need real human judgment.
This partnership between human experts and intelligent machines is where the magic really happens. The goal was never to replace radiologists but to give them superpowers, making the entire diagnostic process faster and more accurate for everyone.
Uncovering Patterns Beyond Human Sight
One of the biggest breakthroughs AI brings to the table is its ability to spot subtle patterns in images that are practically invisible to us. Machine learning models can be trained on enormous datasets of anonymized CT scans, MRIs, and X-rays. Over time, they learn to pick up on the faintest signals of disease.
For example, an AI might detect microscopic calcifications in a mammogram that point to early-stage breast cancer. Or it could notice faint shifts in brain tissue density on a CT scan that warn of a coming stroke. This power turns diagnostics from a reactive process into a proactive one, paving the way for earlier treatments and much better patient outcomes.
AI essentially gives doctors a second set of eyes—eyes that have been trained on a scale no single human could ever match. By analyzing millions of images, it learns to recognize the almost imperceptible signatures of disease, giving clinicians a critical head start.
This isn't just theory. The FDA has approved nearly 700 AI/ML-enabled medical devices, and a staggering 77% of them are built for radiology. This shows just how much trust and investment is pouring into this technology. These tools are already hard at work in hospitals, helping to prioritize critical cases and cut down on diagnostic mistakes.
Automating Workflows and Sharpening Image Quality
Beyond just finding anomalies, AI is also a workhorse for optimizing the day-to-day grind in a radiology department. The development of these tools is often supercharged by powerful hardware and support from tech leaders. For example, incubator programs like Nvidia's Inception program provide crucial support for startups building the next wave of intelligent healthcare solutions. These partnerships are driving real, practical changes.
AI-powered medical imaging software can streamline workflows in a few key ways:
- Intelligent Triage: An algorithm can scan incoming studies and automatically flag those with critical findings. This ensures the most urgent cases jump to the front of the line.
- Smarter Reporting: AI can help draft preliminary reports by automatically pulling out measurements, finding locations, and other standard data. The radiologist then just needs to review, edit, and finalize.
- Image Enhancement: Machine learning can clean up low-dose scans, reducing a patient's radiation exposure without losing diagnostic clarity. It can even build sharp, clear images from noisy or incomplete data.
These automations lift the administrative weight off clinical staff, freeing them up to focus on patient care and complex decision-making.
Training the Next Generation of Diagnostic Tools
Another fascinating frontier is how AI helps create synthetic data. To train a reliable AI model, you need a massive, diverse dataset. But with strict patient privacy rules and the simple scarcity of data for rare diseases, that’s a huge hurdle.
AI gets around this with something called Generative Adversarial Networks (GANs). These networks can create incredibly realistic, completely anonymous medical images from scratch. This synthetic data can then be used to train new models without ever touching confidential patient information. It’s also a game-changer for rare diseases, where finding enough real-world examples is nearly impossible.
This ability to generate data speeds up the entire development and testing cycle for new diagnostic tools, constantly pushing the boundaries of what’s possible. As these AIs get more sophisticated, they’ll become even more deeply woven into clinical practice, becoming an essential part of modern medicine that makes sure every single pixel in a scan is working to save lives.
How Imaging Hardware and Software Push Each Other Forward
The relationship between medical imaging hardware and the software that runs it is a classic feedback loop. One breakthrough always sparks another. Scanners—whether it’s an MRI, CT, or something else—aren't just taking pictures; they're gathering incredibly dense, complex data. It's the software's job to make sense of that data, translating it into something a doctor can actually use to make a diagnosis.
Think about the jump from an old flip-phone camera to a modern DSLR. The first took grainy, low-res photos that any basic program could open. The second captures massive RAW files packed with detail, requiring powerful software like Adobe Lightroom to truly unlock their potential. It's the exact same story in medical imaging. When scanner technology leaps forward, the software has to race to catch up.
This back-and-forth creates a constant cycle of innovation. A hardware advance, like an MRI that sees in higher resolution or a CT scanner that works in seconds, immediately creates a need for better software in medical imaging. The software now has to wrestle with bigger datasets, build 3D models more quickly, and run sophisticated algorithms to pull meaningful insights out of all that new information.
Different Scanners, Different Software Demands
Not all medical images are the same. Each type of hardware, or modality, generates its own unique kind of data, which creates specific challenges and opportunities for the software.
- MRI (Magnetic Resonance Imaging): This is the go-to for incredibly detailed images of soft tissues, like the brain or joints. MRI software needs to be a powerhouse at handling complex 3D and even 4D (functional) datasets.
- CT (Computed Tomography): Using X-rays, CT scanners create detailed slices of the body, perfect for looking at bones, organs, and blood vessels. Speed is often key here, so the software is built for rapid processing and 3D reconstruction, especially in trauma cases.
- Ultrasound: This modality uses sound waves for real-time imaging. Instead of static pictures, the software has to interpret a dynamic video stream, which is a completely different ballgame.
As these machines get better, the data they produce gets richer. A modern CT scanner might capture hundreds of individual "slices" of the body in one go. It’s up to the software to seamlessly stitch them together into a 3D model that a radiologist can spin, slice, and analyze from any angle imaginable.
The pattern is unmistakable: better hardware produces richer, more complex data. That, in turn, demands smarter, more powerful software. This symbiotic relationship is the engine driving progress in diagnostics, letting doctors see inside the human body in ways that were pure science fiction not long ago.
The Market is Moving Toward More Detailed Imaging
This technological race is being fueled by a real clinical need for more detailed images. While ultrasound has been a workhorse for decades, the trend is clearly shifting toward more data-heavy techniques. Projections show the market share for CT imaging is expected to grow from 15% to 16%, while MRI is set to climb from 12% to 14% over a nine-year span. This highlights a clear move toward high-resolution modalities that depend on robust software to be useful, a trend you can see in these medical image analysis software statistics.
This isn't just a matter of preference; it's a clinical necessity. The detailed views from MRI and CT scans are essential for diagnosing and managing complex diseases like cancer, neurological disorders, and heart conditions. As doctors order more of these scans, the pressure builds on developers to create tools that can wrangle the resulting terabytes of data, paving the way for the next wave of diagnostic innovation.
Key Benefits and Real-World Challenges
Advanced software in medical imaging brings some incredible advantages to the table, directly shaping patient care for the better. But let's be real—adopting these systems isn't a simple plug-and-play operation. On one hand, you get sharper diagnostic accuracy and smoother hospital workflows. On the other, you're faced with serious financial, technical, and ethical questions that every healthcare organization has to wrestle with.
The most obvious win is a massive leap in diagnostic precision. AI-powered tools can spot subtle patterns or tiny anomalies a human radiologist might overlook after a long shift, leading to earlier detection and better treatment plans. This software also takes over the repetitive, time-consuming tasks, freeing up radiologists to focus their expertise on the most complex cases that truly need a human touch.
And it doesn't stop there. These platforms completely erase geographical lines. A top-tier specialist in New York can review scans from a small rural clinic in minutes, making expert care accessible to everyone. That kind of collaboration is what directly leads to better outcomes for patients.
The Operational and Financial Hurdles
While the clinical upside is compelling, the practical side of getting these systems up and running can be tough. The first and most significant roadblock for many is the price tag. The cost of buying, integrating, and maintaining these sophisticated software systems can be staggering.
Beyond the initial check you write, there’s the persistent headache of interoperability—making sure all your different software systems can actually talk to each other. If your Radiology Information System (RIS) can't cleanly pass data to your Electronic Health Record (EHR), you end up with frustrating data silos. This not only kills efficiency but can also introduce dangerous errors.
The greatest challenge isn’t just buying the best software; it’s making sure all the different pieces of a hospital's digital ecosystem can speak the same language. Without true interoperability, even the most powerful tools can't deliver their full potential.
Navigating Security and Ethical Complexities
Data security is, of course, paramount. Medical images are deeply personal health information, protected by stringent regulations like HIPAA in the U.S. Any software handling this data must be built like a fortress to prevent breaches, which can be catastrophic for patients and providers alike.
On top of that, the growing role of AI in medical imaging opens up a new can of worms from an ethical standpoint:
- Algorithmic Bias: What happens if an AI model is trained mostly on data from one demographic group? It might be less accurate for others, which could actually make health disparities worse, not better.
- Accountability: If an AI-assisted diagnosis is wrong, who’s on the hook? Figuring out where the responsibility lies—with the software developer, the hospital, or the clinician—is a thorny legal and ethical problem with no easy answers.
These challenges don't mean we should shy away from advanced software in medical imaging. Far from it. They simply underscore the need for a thoughtful, strategic plan for adoption. The key is to balance the powerful benefits against the real-world costs and risks to bring this technology into modern healthcare successfully.
What's Next for Medical Imaging Software?
Medical imaging isn't just getting better; it's getting smarter, faster, and more connected. We're moving away from software that simply lets us view images and heading toward intelligent platforms that actively help manage a patient's entire health journey. A few key trends are driving this fundamental change, and they’re completely reshaping the field.
First and foremost is the massive shift to cloud-based systems. Picture a hospital’s entire imaging archive—all those bulky servers and backup drives—being moved into a secure, elastic digital space. This simple change has profound implications. It frees medical images from the hospital's four walls, making them available to any authorized specialist, anywhere in the world, at a moment's notice.
This is what has fueled the incredible growth of teleradiology. A radiologist in New York can now read a scan for a patient in rural Alaska, and experts from different continents can collaborate on a complex case as if they were in the same room. The bottom line? Faster diagnoses and better access to specialized care, no matter where the patient lives.
From Finding Disease to Predicting It
The next big frontier is predictive analytics. For decades, medical imaging has been reactive; we use it to figure out what's already gone wrong. The future is about being proactive. Software is emerging that won't just spot existing diseases but will help predict future health problems by picking up on subtle patterns in the data that are invisible to the human eye.
Think about it this way: a patient gets a chest CT for one specific reason, but the software simultaneously analyzes their coronary arteries. It might flag early-stage plaque buildup that isn't causing any symptoms yet but points to a high risk of a heart attack down the road. This gives doctors a chance to step in with preventative care long before an emergency ever happens.
This capability transforms a routine diagnostic scan into a powerful screening tool. It’s a genuine shift from just treating sickness to actively preserving wellness.
Building the Complete Patient Picture
Another game-changer is the push for integrated diagnostics. For too long, different types of patient data have lived in separate, disconnected silos. The next generation of software is designed to break down those walls. It won’t just look at medical images in isolation; it will merge that visual data with other critical information.
This approach creates a complete, personalized health profile by combining:
- Imaging Data: The rich anatomical detail from CT, MRI, and PET scans.
- Electronic Health Records (EHR): The patient’s entire medical history, from lab results to doctor's notes.
- Genetic Information: Genomic data that can highlight a person's predisposition to certain conditions.
By weaving these different threads of data together, software can build a multidimensional view of a person's health. This is the foundation for truly personalized medicine, where treatments are designed not just for a disease, but for an individual's unique biology and life story.
This deep integration is where the real power of software in medical imaging will be realized. We're building a more connected, proactive, and intelligent healthcare system. The market is certainly taking notice. The Medical Imaging Software Market is projected to climb from USD 8.75 billion in 2025 to USD 12.76 billion by 2030, a surge driven by AI adoption and increased healthcare investment. You can explore the market forecast from Mordor Intelligence to get a fuller picture of this growth.
Got Questions About Medical Imaging Software? We Have Answers.
Diving into the world of medical imaging software can feel a bit like learning a new language. There are a lot of technical terms and complex ideas floating around. To clear things up, we've put together some plain-English answers to the questions we hear most often.
This isn't just for the tech-savvy. Whether you're a patient wondering about your recent scan or a healthcare pro just starting out, this guide breaks down how it all works.
Is All Medical Imaging Software Basically the Same?
Not even close. The software is built specifically for the type of imaging machine, or modality, it's paired with. For example, an MRI machine is brilliant at capturing detailed images of soft tissues, so its software needs to be a powerhouse at handling huge 3D and 4D datasets. A CT scanner, on the other hand, creates cross-sectional "slices" of the body, and its software is fine-tuned to reconstruct those images at high speed.
On top of that, the software is often specialized for certain medical fields.
- Cardiology software will have built-in tools for measuring how well the heart is pumping.
- Neurology packages come equipped with features designed specifically for analyzing brain scans.
- Oncology software is tailored to help doctors track tumor growth and see how it's responding to treatment.
A good analogy is professional creative software. A video editor and a photo editor both deal with images, but you wouldn't use one to do the other's job. It’s the same story with software in medical imaging—each tool is precision-engineered for a specific diagnostic task.
How Is Patient Data Kept Secure?
Security isn't just a feature; it's the absolute top priority. Medical imaging software operates under strict regulations like the Health Insurance Portability and Accountability Act (HIPAA) to keep patient information locked down. This is done with several layers of security.
First, all data is encrypted. This happens both when it's just sitting on a server (at rest) and when it's being sent over a network (in transit). Access is also strictly limited, so only authorized people—like the radiologist reading the scan or the doctor who ordered it—can view the images. Finally, everything that happens is recorded in an audit trail, which creates a permanent log of who accessed what data and when they did it.
Protecting patient information isn’t an afterthought. It's the bedrock on which all medical imaging software is built. These systems are designed from the ground up to ensure privacy and integrity at every single step.
This multi-layered approach is crucial for earning and keeping patient trust, making sure sensitive health information stays exactly where it belongs: confidential.
Ready to bring smart, reliable AI into your medical imaging workflow? PYCAD specializes in everything from data annotation to deploying custom models, helping you transform complex medical images into clear, actionable insights. See how we can speed up your innovation at https://pycad.co.