Understanding What Makes 2D To 3D Magic Actually Work
Turning 2D medical images into 3D volumes isn't magic, but it feels like it sometimes! It's not just slapping on a filter. It's about mimicking how our brains understand depth. After working with tons of these images, I've learned it boils down to manipulating visual cues. Think about how shadows create a sense of layers, or how the right lighting makes details jump out. That's the key to making a flat image feel three-dimensional.
This screenshot from the Wikipedia page on Stereoscopy shows how two slightly offset images can trick your brain into seeing depth.  The offset mimics how our two eyes see the world from slightly different angles. That tiny difference is what our brain uses to build a 3D picture in our heads.
The offset mimics how our two eyes see the world from slightly different angles. That tiny difference is what our brain uses to build a 3D picture in our heads.
Some images are perfect for 3D conversion, others… not so much. It really depends on the visual information you're starting with. An image with sharp contrast and clear shapes will generally convert much better than a blurry, low-contrast one. For example, a detailed CT scan is a much easier starting point for a 3D volume than a grainy ultrasound image. This difference in image quality has a big impact on the final 3D model and how much detail you can actually see.
The history of 2D to 3D conversion is pretty cool, too. It goes all the way back to the mid-1900s, with things like anaglyphic 3D glasses (the red and blue ones!) popping up in the 1950s. But those old-school methods had problems with depth perception and messed up colors. Things really took off with the arrival of digital tech in the 1990s, which opened the door for all sorts of cool research in computer vision. Discover more insights.
So, knowing your source material is essential. Before you even start thinking about software, take a good look at the image. Analyze things like the lighting, texture, and overall composition. This helps you figure out how well it might convert to 3D, and will guide your choices throughout the entire process. Ultimately, this analysis impacts how realistic and immersive your final 3D representation will be. Then you can bring in techniques like depth mapping and lighting adjustments to enhance those cues and build a more convincing 3D effect. Think of it like seasoning a dish—a little goes a long way, and too much can ruin it!
Finding Your Perfect 3D Conversion Toolkit
I've lost count of the hours I've spent jumping between different tools, trying to wrestle 2D images into 3D. The software world can be a confusing place, with everything from free web-based converters to expensive professional suites. The biggest lesson I've learned? The "best" tool is completely dependent on what you're working on and your own skill level. Turning a portrait into 3D has very different requirements than creating a 3D architectural rendering, for example.
This infographic shows the depth-mapping accuracy you can get with three different techniques. 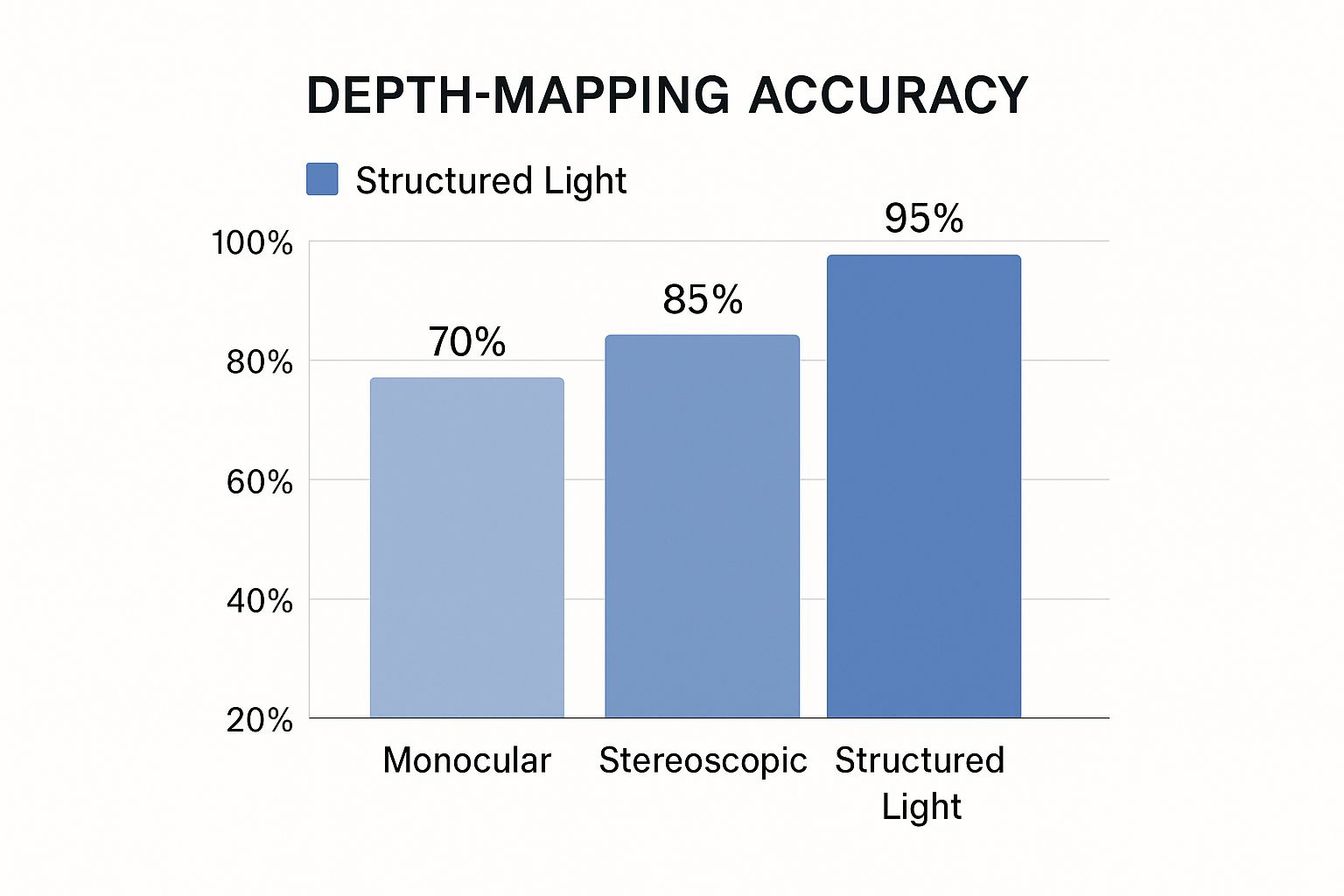 Notice how structured light methods hit the highest accuracy at 95%, followed by stereoscopic at 85% and monocular at 70%. This really highlights the balance you need to strike between complexity and precision when you're picking a 3D conversion method.
Notice how structured light methods hit the highest accuracy at 95%, followed by stereoscopic at 85% and monocular at 70%. This really highlights the balance you need to strike between complexity and precision when you're picking a 3D conversion method.
Let's get into some specifics. For quick and dirty conversions, a GIMP plugin might be surprisingly effective. However, if you're working with something like complex medical image data, you'll need something much more powerful. Think about it: if you’re dealing with intricate anatomical structures from CT scans, you absolutely need a dedicated tool that can handle DICOM data and volume rendering. That's where a program like Adobe After Effects comes into its own, giving you granular control over every single aspect of the 3D conversion process.
This screenshot from the Adobe After Effects product page gives you a sense of its powerful interface. 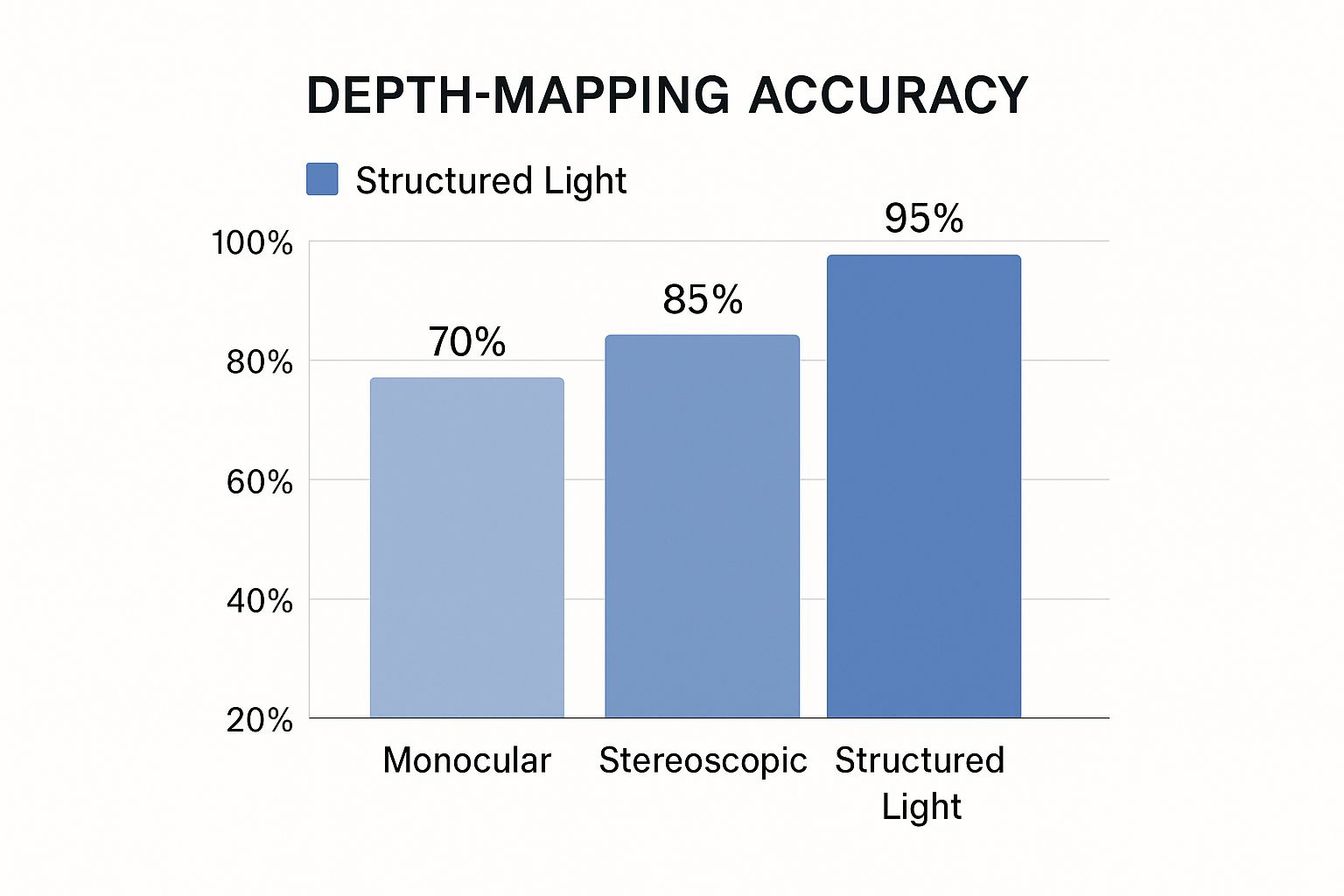 It might seem a little intimidating at first, but that level of control is exactly what you need for accurately representing complex medical data.
It might seem a little intimidating at first, but that level of control is exactly what you need for accurately representing complex medical data.
The image format you're using also makes a difference. Some tools are great for JPEGs, while others are specifically designed for DICOM or other specialized medical image formats. My advice? Always test different tools with your own data. A small test project can prevent major headaches down the line. Don't rely solely on the marketing hype; put the tools through their paces and see how they actually perform. And finally, don't overcomplicate things! Sometimes a simpler tool does the trick perfectly well, and often significantly speeds up your workflow. It’s all about finding the right tool for the specific task, not necessarily the one with all the fancy features. When building your toolkit, you might even consider using these crossposting tools to manage your content efficiently.
2D to 3D Conversion Tools Comparison
Before we go any further, I've put together this comparison table to help you get a quick overview of some popular 2D to 3D conversion tools. It highlights key features, pricing, and the type of projects they're best suited for.
| Tool Name | Price Range | Difficulty Level | Best For | Key Features |
|---|---|---|---|---|
| Blender | Free | Intermediate to Advanced | Animation, Modeling, Rendering | Open-source, versatile, large community support |
| Meshlab | Free | Intermediate | 3D Mesh Processing and Editing | Open-source, mesh repair, cleaning, and simplification |
| 3DF Zephyr | Paid (various tiers) | Beginner to Advanced | Photogrammetry | User-friendly, fast processing, various export options |
| Autodesk Maya | Paid (subscription) | Advanced | Professional 3D Animation and Modeling | Industry-standard, powerful features, complex workflows |
| GIMP (with plugins) | Free | Beginner to Intermediate | Image Editing and Basic 3D Conversion | Free, open-source, requires specific plugins for 3D conversion |
As you can see, there's a tool for every budget and skill level. Remember, the best tool for you will depend on your specific needs and project requirements.
Setting Your Images Up For 3D Success
This is where so many people stumble. I’ve seen amazing projects fall flat because of poor image prep. Truth is, your source image quality accounts for about 70% of the success in 2D to 3D conversion, regardless of your software. So, before diving into complex conversions, let's make sure your starting images are top-notch. When building your toolkit, even something as simple as finding the right crossposting tools can make a surprising difference in streamlining your content workflow.
First, evaluate whether an image is even worth converting. Some compositions, lighting, and detail levels naturally lend themselves to 3D, while others are an uphill battle. For example, a CT scan, with its clear tissue distinctions, is a perfect candidate. A blurry X-ray with overlapping structures? Much harder to convert into a clear 3D volume. This initial assessment saves you headaches later.
Choosing the Right Tools
Here’s a screenshot from the GIMP website: GIMP, while a powerful image editor, highlights the need for specialized tools in 3D medical imaging. Basic 3D manipulation is possible, but dedicated medical imaging software (like programs that handle DICOM files) is crucial for accurate visualizations.
Preprocessing for Success
Next, consider preprocessing. Certain techniques drastically improve conversion success. Think of it like prepping ingredients before cooking. Sharpening, for example, can enhance depth mapping, especially in medical images where subtle density differences are key. But be careful! Over-sharpening creates artifacts that hinder the 3D effect. It's a balancing act.
Color adjustments also impact the 3D effect. This is especially true in medical imaging where color represents tissue densities or other diagnostic data. Increasing contrast can make structures more distinct in the 3D volume, aiding interpretation. But avoid overdoing it – overly saturated colors make the final image look unnatural.
Avoiding Common Pitfalls
Finally, let's discuss subtle mistakes that can derail your project. Over-processing textures is one. While enhancing textures adds realism, too much creates a noisy, cluttered 3D image. This is problematic in medical imaging, where extra details can obscure important anatomical features.
Another mistake is ignoring the original lighting direction. Consistent lighting is crucial for believable 3D, particularly when combining multiple medical images into a single 3D volume. These details may seem minor, but they significantly impact the final quality. Remember, even the best software can't fix a poorly prepared image.
Crafting Depth Maps That Actually Convince Your Eyes
This is where the magic happens – transforming flat 2D images into believable 3D. A depth map is the key. It's like a set of instructions telling the software how far away each pixel should appear in 3D space. Imagine a grayscale image: brighter areas are closer, darker areas further away. After years of working with this, I've learned a few tricks for crafting depth maps that truly bring 3D models to life.
This screenshot, taken from the Wikipedia page on Depth Maps, shows this in action.  The different shades of gray directly translate to perceived depth, giving the illusion of a 3D surface. This is absolutely fundamental to 2D to 3D conversion, particularly in medical imaging.
The different shades of gray directly translate to perceived depth, giving the illusion of a 3D surface. This is absolutely fundamental to 2D to 3D conversion, particularly in medical imaging.
One of the most valuable skills is learning to "see" the depth cues already hiding in plain sight within a 2D image. These cues can be anything from shadows and highlights to perspective lines or even the size of objects relative to each other. In medical images, for example, the varying densities of tissues provide inherent depth cues, which we can translate into a depth map. This makes the resulting 3D model much more accurate and clinically useful.
Manual Depth Map Creation
Manual depth map creation is like digital sculpting. You use image editing software like Photoshop or GIMP to paint shades of gray directly onto the image, mimicking light and shadow. This offers the finest level of control, but it can be time-consuming. It’s especially valuable for medical images, where anatomical accuracy is paramount. This hands-on approach gives you the power to meticulously shape the final 3D model.
Layer Separation
Within manual creation, layer separation is a powerful technique. It involves separating different parts of the image into distinct layers based on their depth – think foreground, middle ground, and background. By creating separate depth maps for each layer, you gain even more control over the final 3D image, resulting in a more nuanced and realistic 3D effect.
Semi-Automated Approaches
For faster results, semi-automated tools can be a lifesaver. There are programs that can automatically generate a basic depth map from an image. This is a great starting point, particularly for simpler images. However, for medical images with their intricate details, you’ll probably still want to refine the automatically generated map manually to really capture the subtle nuances. It’s amazing to think how far 2D to 3D conversion has come! Films like Alice in Wonderland used this technology for specific scenes, blending manual artistry with automated processes. Learn more about this here. This combined approach lets you speed up your workflow without sacrificing creative control – a crucial balance in medical imaging, ensuring both efficiency and precision.
Polishing Your 3D Effects Until They Sing
Getting a basic 3D image from 2D medical scans is just the starting point. The real magic happens in the refinement. This is where a decent conversion transforms into something truly captivating. I’ve seen firsthand how these finishing touches separate the amateurs from the pros. Let me share some of my favorite techniques for elevating your 3D medical visualizations.
Speaking of maintaining visual fidelity, especially with large files, check out this article on compressing image without losing quality. It's a lifesaver when working with high-resolution medical images.
Calibrating Depth Intensity
One of the most critical aspects is calibrating the depth intensity. Too much, and you risk eye strain or a distorted, unrealistic image. Too little, and the 3D effect vanishes. It’s like adjusting the volume – you want it clear, not deafening. Finding that sweet spot is essential, especially in medical visualization where accurate depth perception is paramount.
This is particularly important when you're trying to visualize subtle anatomical structures. Overdoing the depth can make everything look artificially inflated, while underdoing it can obscure important details.
Managing Edge Artifacts
Edge artifacts – those jagged lines around objects – can instantly break the 3D illusion. Carefully masking and smoothing these edges is essential. Think of it like sanding a piece of wood – it’s detail-oriented but crucial for a polished final product. I use Photoshop for this, but other image editing software will work too.
My personal tip: zoom in close and take your time. It’s easy to miss small artifacts that can become glaring issues in the final render.
Enhancing, Not Distracting
The 3D effect should enhance the image, not overpower it. The goal is clarity, not spectacle. In a 3D rendering of a CT scan, the 3D effect should clarify anatomical structures, not create a distorted or exaggerated representation. Subtlety can be surprisingly powerful.
For instance, I once worked on a 3D reconstruction of a fractured bone. A dramatic 3D effect actually made the fracture harder to see, while a more subtle approach made it crystal clear.
Handling Tricky Elements
Hair, glass, and complex textures can often confuse automated 3D conversion systems. Manually refining these areas usually gives the best results. It’s like adding a personal touch – those small adjustments can make a world of difference.
I've found that using specialized 3D modeling software like Blender can be really helpful for these tricky bits. It allows for more precise control than standard image editing software.
3D Color Correction
Color plays a crucial role in 3D, and standard color correction techniques might not be enough. You might need to adjust colors specifically for the 3D effect, ensuring visual coherence across different viewing angles and lighting. This is especially important for medical images where color can convey critical diagnostic information.
I recommend experimenting with different color palettes and lighting setups. What looks good in 2D might not translate well to 3D.
Maintaining Visual Coherence
Finally, consider how the 3D image will be viewed. Different displays and lighting environments can affect the 3D effect. Testing your results on various devices is vital to ensure your work looks its best, no matter how it’s viewed.
Before we move on, let’s take a look at some key parameters and their impact on the 3D effect. The table below summarizes some common challenges and best practices that I’ve learned over time.
The following table provides a guide for fine-tuning the 3D effect in your medical visualizations. It's a compilation of some of the most important parameters and how they influence the final result.
| Parameter | Effect on Image | Recommended Range | Common Issues | Best Practices |
|---|---|---|---|---|
| Depth Intensity | Controls the perceived depth of the 3D effect | 0.1 – 1.0 | Exaggerated depth can distort the image; Insufficient depth makes the 3D effect barely noticeable | Start low and gradually increase until the optimal depth is achieved; Consider the specific anatomical structures being visualized |
| Edge Smoothing | Softens the edges of 3D objects | 1 – 5 pixels | Over-smoothing can blur details; Insufficient smoothing results in jagged edges | Adjust based on the resolution of the image; Focus on areas with prominent artifacts |
| Color Saturation | Influences the vibrancy of colors in 3D | 80% – 100% | Oversaturation can appear unrealistic; Undersaturation can make the image look dull | Adjust to maintain realistic color representation; Consider the diagnostic value of color in medical images |
| Lighting Intensity | Controls the brightness and contrast of the 3D scene | 50% – 100% | Harsh lighting can wash out details; Dim lighting can obscure important features | Adjust based on the complexity of the 3D model; Use multiple light sources for optimal illumination |
| Texture Detail | Determines the level of detail in surface textures | Medium – High | Excessive detail can increase rendering time; Low detail can make the image look flat | Balance detail with performance; Focus on textures that contribute to anatomical understanding |
This table summarizes some of the key parameters I’ve found to be most impactful. Experimenting with these settings is key to finding the perfect balance for your specific visualizations. Remember, these are just guidelines, and the best settings will always depend on the specific image and your artistic goals.
Sharing Your 3D Masterpieces Across Every Platform
So, you’ve successfully transformed your 2D medical images into impressive 3D volumes. Fantastic! Now, the next big question is: how do you share these creations with the world? Trust me, showcasing your work effectively is just as crucial as the conversion process itself. From my own experience, I can tell you that each platform, whether it’s Instagram or a prestigious scientific journal, has its own unique requirements. I’ve learned a thing or two about what really works, and I’m happy to share some tips.

Optimizing for Different Platforms
Social media, for example, thrives on visually captivating, bite-sized content. Short videos showcasing a rotating 3D organ model can be extremely effective, as can interactive 3D images that allow viewers to explore different anatomical layers. Think engaging and easily digestible.
On the other hand, if you’re aiming for print publications, high-resolution static images are your best bet. The focus here should be on crystal-clear image quality and accurate anatomical representation. And don't forget about creating tutorials to demonstrate your 3D modeling skills. Check out this helpful resource on how to create video tutorials.
Then there are the increasingly popular VR/AR platforms, which offer some truly mind-blowing possibilities. Imagine a surgeon exploring a patient’s 3D heart model in virtual reality before performing an operation! The key here is optimizing for real-time performance. You need to strike a balance between visual fidelity and smooth, lag-free interaction. Imagine how frustrating a slow, jerky 3D model would be during pre-operative planning – not ideal!
Interestingly, the entertainment industry has played a significant role in advancing 2D to 3D conversion techniques. The global 3D film market has seen remarkable growth. Even way back in the 1950s, which is considered the ‘golden era’ of 3D, films like Bwana Devil were hugely successful. Want to dive deeper? Here's a fascinating look at the history of 3D technology.
Compression and Future-Proofing
Let's talk about file sizes. Large files can be a real headache. Compression techniques, like reducing the polygon count in your 3D models, can help make your files more manageable without sacrificing too much detail. It's all about finding the sweet spot – the right balance for your particular project. Especially with medical imaging, preserving diagnostic quality during compression is absolutely essential. A slightly smaller file size isn’t worth it if you lose crucial clinical information.
Thinking ahead and future-proofing your work is also something to keep in mind. Display technologies are constantly evolving, so your export settings should too. Stay up-to-date with the latest file formats and compression standards. This ensures your 3D medical images remain compatible with emerging devices.
Testing Your Results
Finally, and I can't stress this enough: test, test, test! View your 3D content on a variety of devices – phones, tablets, computers, VR headsets – to make sure it looks fantastic on every platform. Something that looks stunning on your high-end monitor might look distorted or pixelated on a smaller screen. In medical visualization especially, consistent rendering across different platforms is vital for accurate diagnosis and treatment planning. Thorough testing ensures your hard work translates into impactful 3D visuals, no matter where they’re viewed.
Key Takeaways
Turning 2D medical images into 3D volumes is a powerful technique, but it's not magic. It's about understanding visual cues and how to create a convincing illusion of depth. Your source image quality is everything. A blurry, low-contrast image just won’t convert well, no matter how fancy your software is. Think of the difference between a crisp CT scan and a grainy ultrasound—it’s huge! Starting with good quality images is 70% of the battle.
So, before you even open your software, really look at your image. Is the composition right? Is the lighting even? Is there enough detail? This initial assessment will save you so much time and frustration later on. Then, prep your images carefully. Sharpening can help with depth mapping, but too much creates weird artifacts. Color adjustments can also boost the 3D effect, but be careful not to oversaturate. It’s a delicate balancing act.
The depth map is essentially your roadmap. It tells the software how to translate that 2D data into 3D space. Think of it like a sculptor's blueprint, guiding the creation of the final form. Creating a depth map manually gives you maximum control, but semi-automated tools in software like Blender can be a great starting point. From there, it’s all about refinement. Adjust the depth intensity until it feels just right – too much and it looks strained, too little and the 3D effect disappears. Smooth out any jagged edge artifacts and make sure the 3D effect enhances, not distracts from, the medical data.
Finally, remember to optimize your 3D visualizations for different platforms. A rotating 3D model on social media needs different settings than a high-resolution still image for a medical journal. Test your final product on different devices—phones, tablets, computers—to make sure it looks good everywhere.
Ready to see what AI can do for your medical images? Check out PYCAD to see how it can transform your 2D medical images into stunning, interactive 3D volumes.






