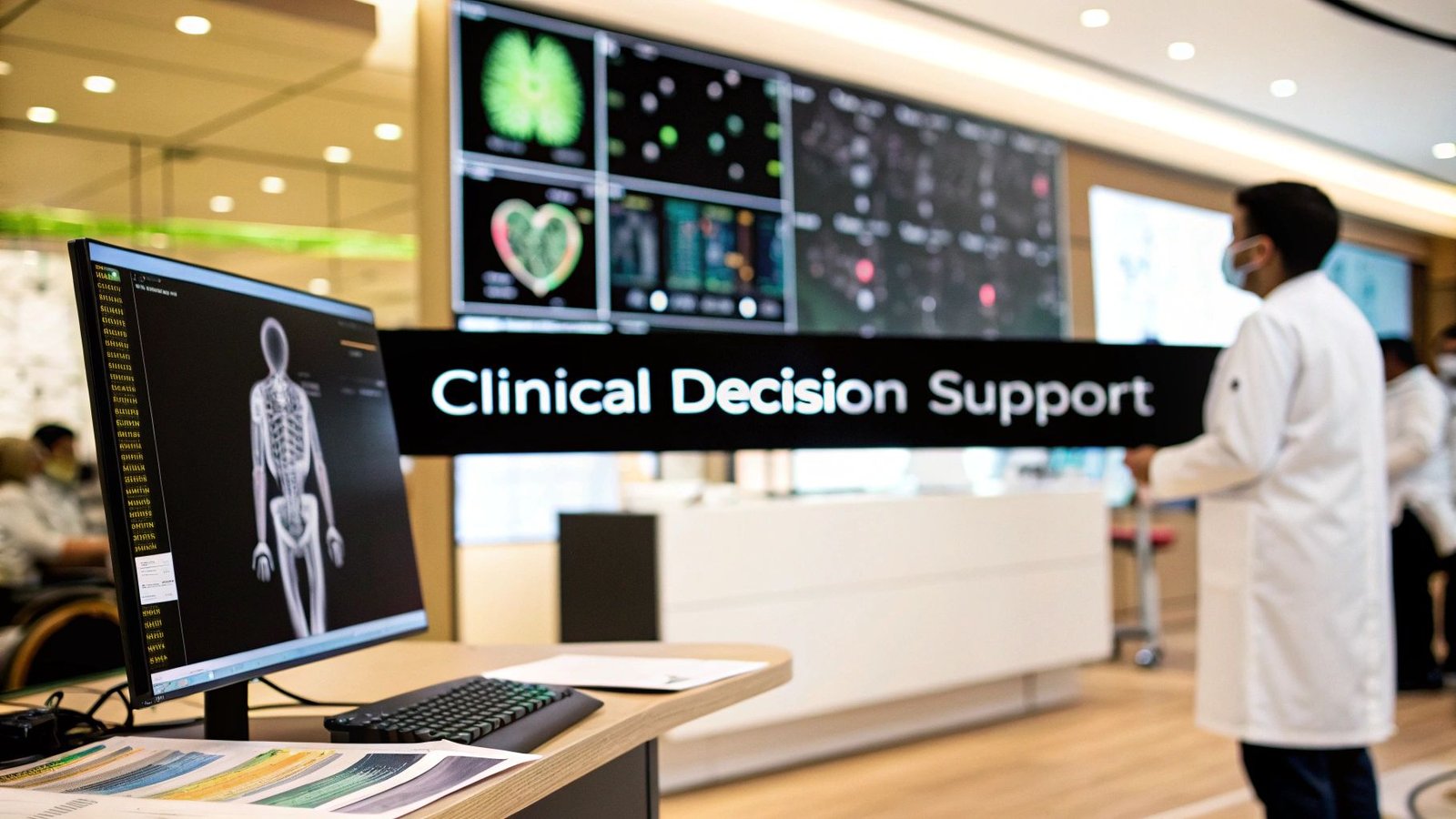
Think of a Clinical Decision Support System (CDSS) as an expert co-pilot for doctors and nurses. It’s a smart software tool that digs into a patient's electronic health record (EHR) in real-time, checking that information against a massive library of established medical knowledge. The goal? To offer up timely alerts, helpful reminders, and solid recommendations right when a clinician needs them most—without ever getting in the way.
It’s crucial to understand that a CDSS is designed to enhance a professional's judgment, not replace it.
Unpacking the Role of a CDSS in Modern Healthcare
Picture this: a doctor is treating an older patient with three different chronic conditions. Before writing a single prescription, they have to juggle the patient’s full medical history, a dozen recent lab results, and a long list of existing medications. It’s a mental marathon. In this scenario, a CDSS acts as an intelligent safety net.
This isn't some futuristic robot making diagnoses on its own. It's a practical, integrated tool that works inside the systems clinicians already use every day. At its heart, a CDSS gives healthcare professionals the critical insights they need for true data-driven decision making, which is fundamental to boosting both patient outcomes and hospital efficiency.
What Does a CDSS Actually Do?
The main purpose of any CDSS is to deliver the right information, to the right person, at exactly the right time. This simple idea powers some incredibly important functions.
To put it in perspective, here’s a breakdown of the core tasks a CDSS handles behind the scenes.
Core Functions of a Clinical Decision Support System
| Core Function | What It Does | Example |
|---|---|---|
| Error Prevention | Scans for potential mistakes before they happen. | Flagging a potentially dangerous drug interaction or alerting a doctor if a prescribed dose is too high for a patient's age and weight. |
| Guideline Adherence | Ensures care aligns with the latest evidence-based practices. | Reminding a clinician to recommend a specific cancer screening based on a patient’s unique risk factors. |
| Diagnostic Support | Helps broaden a clinician's perspective on possible diagnoses. | Suggesting a list of potential conditions based on a patient's reported symptoms and recent lab results. |
These functions help translate a mountain of complex data into clear, actionable steps.
A well-designed CDSS helps bridge the gap between the vast, ever-growing body of medical knowledge and the practical application of that knowledge at the point of care.
Market Growth and Adoption
It's no surprise that the demand for these systems is skyrocketing. As healthcare organizations double down on patient safety and efficiency, CDSS is becoming a must-have.
The global market is projected to climb from USD 2.25 billion in 2024 to USD 3.89 billion by 2030. That's a compound annual growth rate of 9.6%. This boom is largely driven by the near-universal adoption of EHRs and huge leaps in AI that are making these systems smarter and more intuitive than ever before.
By turning raw patient data into structured, contextual guidance, a clinical decision support system provides a crucial layer of intelligence that supports better, safer, and more consistent care across the board.
The Three Core Components of a CDSS
To really get a handle on what a clinical decision support system is, it’s best not to think of it as some mysterious black box. Instead, picture it as a highly coordinated team of three specialists working in perfect sync. Each one has a specific job, and it’s their seamless collaboration that transforms raw patient data into actionable clinical advice.
Think of it like an expert kitchen crew. You have the master cookbook, the head chef, and the waiter who presents the final dish.
This infographic lays out the basic structure, showing how these core components fit together.
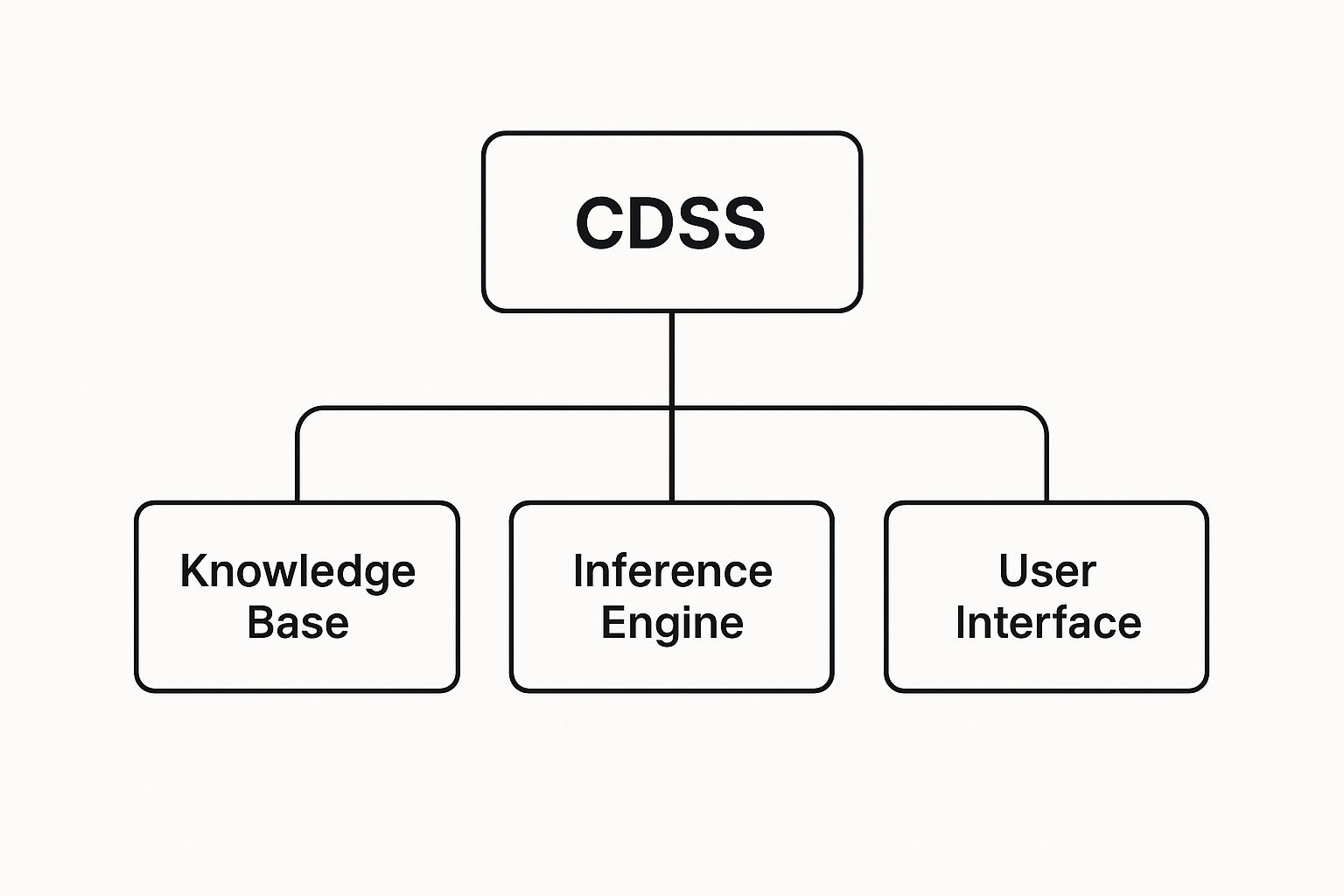
As you can see, these three elements—the knowledge base, the inference engine, and the user interface—are the foundational pillars holding the whole system up.
The Knowledge Base: The Master Cookbook
The first and most critical piece is the knowledge base. This is the system's "brain" or, to stick with our analogy, its master cookbook. It’s a massive, carefully organized digital library packed with the information the CDSS needs to make smart recommendations.
This isn't just a simple database. It’s a structured collection of clinical knowledge, often represented as a series of rules, associations, or logical statements that the system can interpret and act on.
So, what kind of information is inside?
- Clinical Guidelines: Evidence-based best practices from leading medical bodies.
- Medical Literature: Key findings from peer-reviewed journals and major clinical trials.
- Drug Information: Crucial details on dosages, contraindications, and potential interactions.
- Patient Data Patterns: Insights drawn from anonymized data trends across millions of past cases.
A good knowledge base is never static; it's constantly updated to reflect the latest medical research. This ensures the advice it gives is always current and trustworthy. It is the single source of truth for the entire system.
The Inference Engine: The Expert Chef
If the knowledge base is the cookbook, then the inference engine is the expert chef. This is the logical core of the CDSS, the part that does the actual "thinking." It takes the ingredients—a specific patient's data, pulled from their Electronic Health Record (EHR)—and applies the right recipes from the knowledge base.
The inference engine uses reasoning methods, most commonly if-then rules, to connect the dots between an individual patient's data and the established medical knowledge.
For example, an if-then rule might be programmed like this:
IF a patient is prescribed Medication A AND their chart shows a severe allergy to Medication B (which is in the same drug class), THEN trigger a high-priority alert for the prescribing clinician.
This is the component that analyzes the situation, spots potential problems or opportunities, and formulates a logical recommendation. In essence, it asks, "Given this unique patient's situation, what does our medical knowledge tell us to do?"
The Communication Mechanism: The Final Dish
Finally, the communication mechanism—often called the user interface—is what delivers the finished product. This component acts as the waiter, presenting the chef's creation (the system's insight) to the clinician in a clear, timely, and easy-to-understand way.
The success of the entire CDSS really hinges on this last step. Even the most brilliant insight is useless if it's confusing, disruptive, or arrives too late. One study revealed that clinicians ignore safety notifications between 49% and 96% of the time, often because poor interface design leads to "alert fatigue."
To be effective, communication mechanisms need to be well-designed. Common examples include:
- Alerts and Reminders: Pop-up boxes that flag critical issues like drug allergies or duplicate orders.
- Order Sets: Pre-configured groups of orders for specific conditions, like community-acquired pneumonia.
- Information Displays: Dashboards that visualize patient data or highlight relevant clinical guidelines.
- Filtered Data Views: Interfaces that only show the most relevant lab results or notes for the task at hand.
This final piece ensures the right information gets to the right person, in the right format, directly within their natural workflow. It's what makes the system a genuinely helpful partner in care.
How a CDSS Works in a Clinical Setting

It’s one thing to understand the building blocks of a CDSS, but it’s another to see it in action in a busy clinic. A CDSS isn't some clunky, separate program a doctor has to log into. Instead, it’s woven directly into the tools they use all day, every day—primarily the Electronic Health Record (EHR).
Think of it as a silent partner working in the background. As a physician charts new symptoms, orders a lab test, or writes a prescription, the CDSS is constantly scanning that information. It’s like a vigilant assistant, cross-referencing every new data point against the patient’s full medical history and a massive, evidence-based knowledge base. This all happens in a blink, delivering support right at the moment a decision is being made.
Passive vs. Active Support Systems
Not all support from a CDSS looks the same. The interventions generally fall into two camps: passive and active. A well-built system will blend both to give clinicians comprehensive backup without creating a ton of noise.
A passive CDSS is like having a digital medical library built right into the EHR. It doesn't interrupt the workflow but surfaces relevant information for the clinician to explore if they choose. For example, if a doctor opens the chart of a patient with Type 2 diabetes, a small, non-intrusive link might appear offering the latest treatment guidelines from the American Diabetes Association. It’s there if you need it, gone if you don’t.
An active CDSS, on the other hand, is much more direct. It jumps in proactively when it spots a potential problem that needs a second look. This is the system that generates those pop-up alerts and warning flags. It’s designed to be an unmissable safety net for high-risk scenarios, forcing a pause before the clinician can move forward.
An active CDSS is the digital equivalent of a colleague tapping you on the shoulder to say, "Wait, did you see the patient is allergic to that?" It’s a critical backstop against human error.
The real difference is in the delivery. Passive support offers optional resources, while active support demands attention for critical safety checks.
Common Triggers That Activate a CDSS
A CDSS is intentionally designed to stay quiet until it’s actually needed. This trigger-based approach keeps the advice relevant and timely. If the system fired off alerts constantly, it would create "alert fatigue"—a very real problem where clinicians become so overwhelmed with notifications that they start ignoring them all, even the important ones.
So, what wakes the system up?
- Prescribing a New Medication: This is probably the most common trigger. The moment a doctor enters a new prescription, the CDSS instantly checks for drug-drug interactions, drug-allergy conflicts, or even duplicate therapies. It can also flag a dose that seems off based on the patient's weight, age, or kidney function.
- Ordering a Lab or Imaging Test: The system might flag a duplicate order if the same CT scan was done last week. Or, it could suggest a more appropriate test based on the patient’s symptoms, potentially saving time and money.
- Entering a New Diagnosis: Charting a new condition can trigger reminders for standard care protocols. For example, diagnosing a patient with hypertension might prompt a suggestion to order a lipid panel and provide links to patient education on lifestyle changes.
- Reviewing Patient Vitals: A sudden, worrying change—like a sharp drop in blood pressure or a spiking fever—can trigger an alert. The system might suggest sepsis as a possible diagnosis to consider, prompting earlier intervention.
By tying these interventions to specific, everyday actions, a CDSS becomes a natural part of the care process. It turns the EHR from a static filing cabinet into an intelligent, dynamic partner that helps clinicians deliver safer and more effective care.
Real-World CDSS Applications in Healthcare

It’s one thing to understand the mechanics of a CDSS, but where do these systems really prove their worth? The answer is on the front lines of patient care—in busy hospitals, specialized clinics, and everyday doctor's offices.
These tools aren’t just theoretical concepts; they are actively making a difference in clinical efficiency and patient outcomes every single day. Let's look at a few concrete examples of how CDSS works in the real world.
A Second Set of Eyes in Medical Imaging
A radiologist’s workload is staggering. They might review hundreds of complex CT scans or MRIs in a single shift, where missing one tiny detail could change a patient's entire diagnosis. This is where a CDSS becomes an invaluable partner.
Think about a radiologist searching a chest CT scan for a pulmonary embolism. An AI-powered CDSS, built directly into their imaging software, analyzes the scan in the background. It flags suspicious areas that might point to a blood clot, guiding the radiologist's attention to potential issues that could otherwise be missed during a long, demanding day.
- Before CDSS: The diagnosis depends entirely on the radiologist’s expertise and visual search, which, while highly skilled, is still susceptible to human fatigue.
- After CDSS: The system acts as a safety net, highlighting critical findings and helping to prioritize the most urgent cases for review.
This doesn't mean the machine takes over. Far from it. The CDSS simply augments the radiologist's judgment, letting them focus their expertise and confirm findings with a much higher degree of confidence.
Preventing Errors in Medication Management
Medication errors are a serious, yet often preventable, source of patient harm. A CDSS acts as a critical safety net at the moment a prescription is written, protecting both doctors and their patients.
Picture a primary care doctor prescribing a new blood pressure medication for an elderly patient who is already on several other drugs.
As the doctor enters the prescription into the electronic health record (EHR), the CDSS instantly scans the patient's full medication list, allergies, and recent lab results. It might trigger an alert for a dangerous drug-drug interaction or warn that the dose is too high for someone with reduced kidney function.
This automated check is a powerful safeguard against adverse drug events. Without it, the physician would have to manually cross-reference everything—a time-consuming process that’s easy to get wrong in a fast-paced clinical setting.
Shifting the Focus to Proactive and Preventive Care
CDSS also plays a vital part in moving healthcare from a reactive "fix-it" model to one that is proactive and preventive. It works quietly behind the scenes to ensure patients get the routine care they need, based on established, evidence-based guidelines.
For instance, during a routine appointment, a doctor might be focused on the patient's immediate complaints. The CDSS, meanwhile, analyzes the patient’s complete profile—age, gender, medical history—and might generate a simple on-screen reminder: "Patient is a 52-year-old female, due for a routine mammogram screening."
This gentle nudge ensures that critical preventive screenings don't get overlooked. This function is fundamental to improving population health and fits perfectly into the landscape of value-based care.
The demand for these versatile tools is growing fast. The clinical decision support systems market is broken down by product type (like standalone vs. integrated systems) and by specific uses, such as flagging drug interactions or providing dosing support. North America is currently the biggest player, holding over 43% of the global market share in 2024, though major growth is anticipated in the Asia Pacific region as IT investment in healthcare ramps up.
At the end of the day, each of these examples reinforces a core truth about what a clinical decision support system is: it’s a technology built to empower human experts, helping them do their jobs more safely, accurately, and effectively.
How AI Is Supercharging Clinical Decision Support
The next big leap for clinical decision support is already happening, and it’s being fueled by Artificial Intelligence (AI) and Machine Learning (ML). While older systems were a huge step forward, they mostly ran on rigid, pre-programmed 'if-then' logic. AI-powered platforms are a fundamental shift away from that static model to something far more dynamic and intelligent.
Instead of just following a script, these modern systems actually learn. They can analyze millions of anonymized patient records, lab results, and medical images to find subtle patterns a human might never spot. This allows them to do more than just send simple alerts; they can offer predictive insights and deeply personalized recommendations.
From Rules to Real-Time Learning
The biggest difference comes down to adaptability. A traditional CDSS is like a detailed checklist—fantastic for making sure standard protocols are met, but it can't adjust to new information on its own. It needs human experts to manually feed it new guidelines and research to stay current.
An AI-powered CDSS, on the other hand, is more like having a seasoned clinical researcher working right alongside you. It learns continuously from the endless stream of new data, constantly sharpening its understanding. This machine learning capability turns the system from a static reference manual into an adaptive partner that gets smarter and more precise over time.
For example, an older system might flag a potential drug interaction based on a known rule. An AI-powered system can take it a step further by predicting a patient's risk of a rare side effect, comparing their unique mix of biomarkers to patterns it has identified across massive datasets.
The Power of Predictive Analytics
One of the most exciting ways AI is enhancing clinical decision support is through predictive analytics. This is the ability to forecast potential health problems before they happen, letting clinicians shift from reactive treatment to proactive care. It’s about seeing the storm clouds gather, not just reacting when the downpour starts.
Think about a patient in the ICU. An AI model can constantly monitor dozens of data streams—heart rate variability, breathing patterns, blood oxygen levels, and tiny changes in lab values. By recognizing the faint signals that often precede a crisis, the system can alert the care team to a high risk of sepsis hours before the patient shows obvious symptoms.
This predictive power is a game-changer. It gives clinicians a crucial head start, enabling earlier, more effective interventions that can significantly improve patient outcomes and even save lives.
Other powerful predictive uses include:
- Forecasting Hospital Readmissions: Pinpointing patients at high risk of returning to the hospital soon after discharge, which allows for focused follow-up care.
- Predicting Disease Progression: Modeling how a chronic condition like kidney disease might worsen based on a patient’s specific health data.
- Identifying High-Risk Surgical Patients: Analyzing pre-op data to flag patients who are more likely to face complications.
Making Truly Personalized Medicine a Reality
AI is also the engine driving truly personalized medicine. A traditional CDSS gives advice based on studies of the general population, but AI can customize that guidance for a single individual. By factoring in genomic data, lifestyle information, and even social determinants of health, the system helps answer the question: "What is the best course of action for this specific patient?"
For example, an AI-driven CDSS could analyze a patient's genetic markers to predict how they’ll respond to different chemotherapy drugs. This helps an oncologist choose the most effective treatment with the fewest side effects, moving beyond evidence-based medicine into truly individualized care plans.
This new level of detail makes what a clinical decision support system is something much more profound. It's no longer just a safety net; it becomes a powerful amplifier for clinical expertise. It takes on the monumental task of sifting through data and finding patterns, freeing up doctors to concentrate on the uniquely human side of medicine—empathy, communication, and complex, nuanced judgment. The AI doesn’t replace the clinician; it gives them deeper insights to provide better care than ever before.
The Highs and Lows of Clinical Decision Support
Bringing a clinical decision support system (CDSS) into a hospital or clinic is a big deal. It’s not just about installing new software; it's about fundamentally changing how clinicians work. While the potential is enormous, the road to getting it right is often bumpy. It pays to have a realistic grasp of both the incredible benefits and the very real roadblocks you'll likely encounter.
The promise of CDSS is easy to see. Imagine a system that acts as a second set of eyes, catching potential medication errors before they can cause harm. That’s the core value. Beyond that, it helps ensure every patient gets care that’s backed by the latest medical science, creating a more consistent, high-quality standard across the organization.
But making that a reality means tackling some serious technical, financial, and human-centered problems head-on.
The Wins: What a Great CDSS Can Do
At its heart, a CDSS is an intelligent safety net. Think about it: a system that automatically flags dangerous drug-drug interactions, checks for patient allergies, or questions an unusual dosage is a powerful tool for preventing harm. These adverse drug events are a huge source of preventable injury in healthcare, and CDSS is one of our best defenses.
But it’s not just about preventing mistakes. These systems are also fantastic for standardizing top-tier care. By embedding the latest clinical guidelines right into a doctor's daily workflow, a CDSS can nudge them toward best practices at the exact moment they’re making a decision. This leads to more consistent treatments and, ultimately, better patient outcomes. The time-saving aspect is a bonus—automated reminders and pre-built order sets mean less clicking and more focus on the patient.
The industry is betting big on this technology. The global CDSS market is expected to surge, with some projections putting it at USD 10.71 billion by 2030. This isn't just hype; it reflects a genuine push for safer, evidence-based medicine and smarter analytics. If you want to dig into the numbers, you can explore detailed projections about the future of the CDSS market.
The Hurdles: Common Challenges on the Ground
For all its potential, a clumsy CDSS implementation can create more problems than it solves. The most common complaint by far is alert fatigue. When clinicians are flooded with constant, low-priority pop-ups, they naturally start tuning them out. This creates a dangerous "boy who cried wolf" scenario where even the most critical warnings get ignored.
One study revealed a shocking statistic: clinicians ignore safety notifications between 49% and 96% of the time. The reason? Poorly designed alerts that just weren't relevant to the situation. This shows just how crucial it is to build a system that only speaks up when it truly matters.
Beyond alert fatigue, other major headaches include:
- Wrestling with Integration: Making a new CDSS play nice with an existing Electronic Health Record (EHR) system is often a messy, complicated, and expensive technical project.
- The Sticker Shock: The upfront cost for software, the integration work, and properly training the entire staff can be a major financial barrier. It requires serious buy-in from leadership.
- Winning Over the Users: If the system is slow, clunky, or feels like a roadblock, doctors will find a way to work around it. User-friendly design isn't just a nice-to-have; it's the single most important factor for getting people to actually use the tool.
Getting past these obstacles is the key to unlocking what a CDSS can really do. When done right, it stops being just another piece of software and becomes a trusted partner in providing exceptional patient care.
Your CDSS Questions, Answered
It's natural to have questions when we talk about bringing more technology into healthcare. Let's clear up some of the common ones about Clinical Decision Support Systems.
Is a CDSS Just Another Name for an Electronic Health Record (EHR)?
Not quite, though they work hand-in-hand. Think of the Electronic Health Record (EHR) as a patient’s comprehensive digital chart. It’s the repository—the digital filing cabinet—holding every lab result, doctor's note, and prescription.
A CDSS, on the other hand, is the smart assistant that reads that chart. It actively analyzes all that data to offer clinicians timely, relevant advice right when they need it. The EHR stores the information; the CDSS helps make sense of it.
Are These Systems Going to Replace Doctors or Nurses?
That’s a common concern, but the answer is a firm no. A CDSS is a tool designed to augment a clinician's judgment, not replace it. It’s like a super-powered assistant that can instantly cross-reference a patient's entire history against the latest medical guidelines—a task that would be impossible for a human to do in real-time.
This frees up doctors and nurses to focus on what they do best: applying their experience, communicating with patients, and handling the complex, nuanced art of medicine. Think of it as a co-pilot, not the pilot.
A well-designed CDSS doesn't take over; it provides an evidence-based safety net. It empowers clinicians to make even better, more confident decisions, which ultimately leads to safer and more effective patient care.
What's the Biggest Hurdle to Getting a CDSS Right?
Without a doubt, the biggest challenge is something called "alert fatigue." This is what happens when a system bombards clinicians with too many notifications, many of which are irrelevant or low-priority.
When people are overwhelmed with constant beeps and pop-ups, they start to tune them out. This is a huge problem because they might ignore a genuinely critical warning. In fact, studies have shown that clinicians can end up overriding safety alerts anywhere from 49% to 96% of the time, simply because the system is too "noisy."
The secret to a successful CDSS isn't just installing it; it's carefully calibrating it to make sure every alert is meaningful.
At PYCAD, we specialize in building the intelligent AI models that power the next generation of medical imaging tools. Discover how our expertise in data handling and model deployment can enhance your medical devices. Learn more at https://pycad.co.