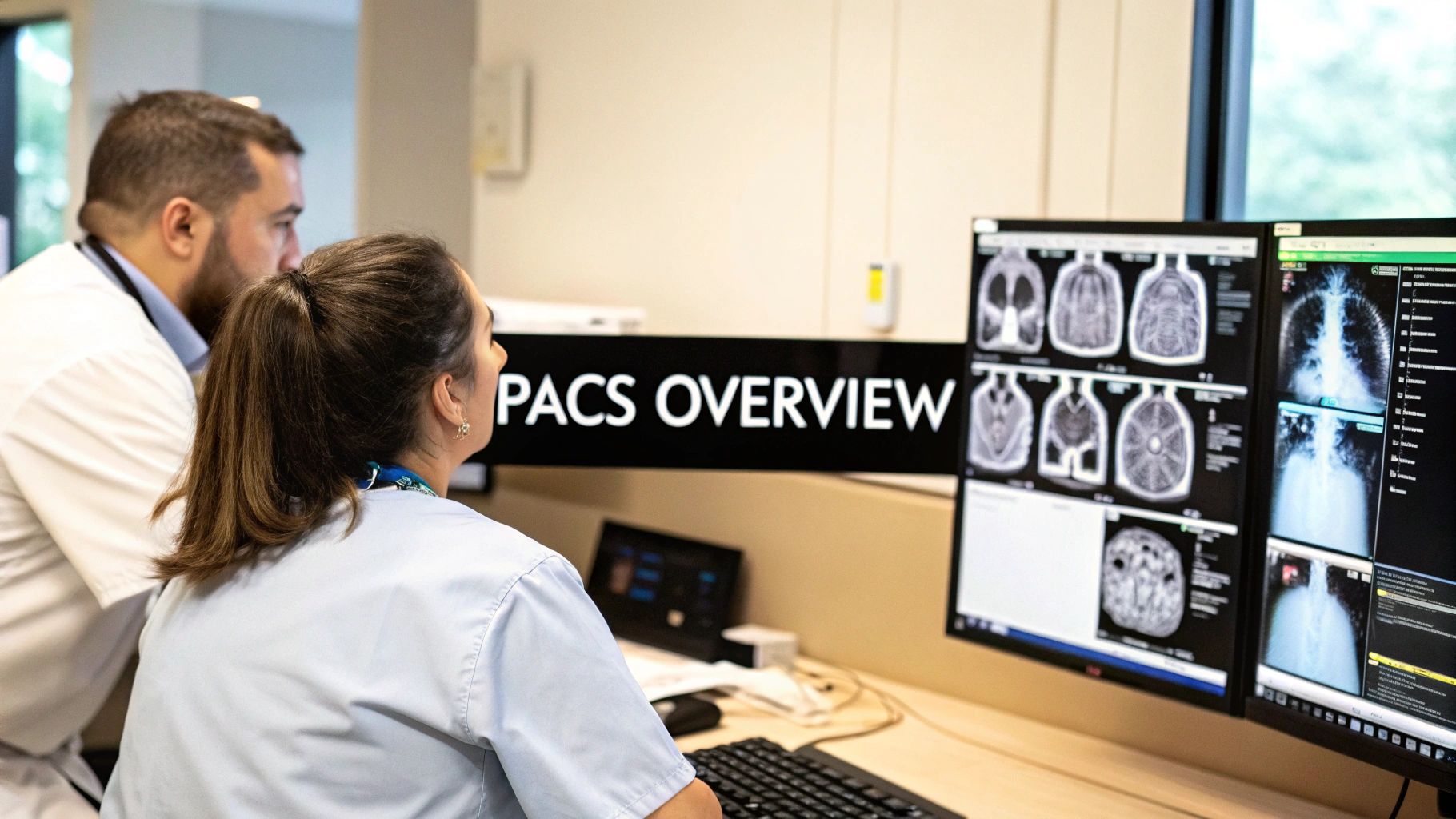
Think of a highly secure, incredibly powerful photo library, but instead of vacation pictures, it's filled with X-rays, CT scans, and MRIs. That's the essence of a PACS, which stands for Picture Archiving and Communication System. It's the digital heart of modern medical imaging, completely replacing the old, dusty film rooms and allowing doctors to access, review, and share patient scans instantly from any approved device.
The Digital Backbone of Modern Radiology
At its most basic level, a PACS is a specialized network of computers and software engineered to handle the massive data volumes that medical imaging produces. It’s hard to overstate how different things were before PACS became widespread. Radiology departments were literally warehouses of filing cabinets, crammed with heavy film jackets.
If a doctor needed to see a patient's previous X-ray for comparison, someone had to physically locate it, a process that could take minutes or even hours. Films could get lost, damaged, or misfiled. Sharing them with a specialist across town? That meant sending them by courier. This old manual system was sluggish, unreliable, and ripe for error.
PACS changes everything by digitizing that entire workflow. Now, when a patient has a scan, the images travel directly from the imaging machine to a central digital archive. From there, a radiologist can pull up crystal-clear images on a high-resolution monitor in seconds. No waiting, no couriers, no lost films.
From Physical Film to Instant Access
This shift from physical to digital isn't just a minor upgrade; it fundamentally reshapes how clinical teams work with patient information. The advantages ripple throughout the entire healthcare organization.
Here are a few of the most significant improvements:
- Immediate Availability: Clinicians can view images the moment the scan is complete. In an emergency, where every second is critical, this speed can be lifesaving.
- Simultaneous Access: Multiple specialists in different departments—or even different cities—can review the same study at the same time, collaborating in real-time on a tricky diagnosis.
- Elimination of Physical Storage: Hospitals have reclaimed huge amounts of real estate once dedicated to film libraries, cutting costs tied to storage, retrieval, and management.
- Enhanced Security: Digital files are far less prone to being lost or damaged than physical film. Plus, every access is tracked and controlled, protecting patient privacy.
To really understand what a PACS is, it helps to see it as a specialized component within the larger world of healthcare document management systems. While a PACS focuses exclusively on images, it's a key part of the broader move toward making all patient information digital, secure, and readily available.
To break it down further, here's a quick summary of what a PACS really does day-to-day.
PACS at a Glance Core Functions
| Function | Description | Real-World Impact |
|---|---|---|
| Archiving | Securely stores vast quantities of medical images and related data in a centralized digital repository. | A patient's entire imaging history (X-rays, MRIs, etc.) is available in one place, instantly. No more hunting for old films. |
| Communication | Transmits images from medical scanners (modalities) to workstations and other systems across a network. | An ER doctor can view a CT scan within minutes of it being taken, enabling rapid diagnosis for a trauma patient. |
| Viewing (Display) | Provides clinicians with specialized software on high-resolution monitors to view and manipulate images. | Radiologists can zoom, pan, and measure anatomical structures with precision, leading to more accurate interpretations. |
| Workflow Management | Automates and organizes the flow of imaging studies, from order entry to final report distribution. | The system automatically routes a new study to the next available radiologist, balancing workloads and reducing report turnaround time. |
These functions work together to create a cohesive system that supports clinicians from the moment an imaging exam is ordered until the final report is in the patient's chart.
Key Takeaway: A PACS is much more than a digital filing cabinet. It's an active communication network that connects imaging equipment, storage archives, and clinical workstations into a seamless ecosystem. This digital foundation is absolutely essential for delivering efficient, high-quality patient care in any modern medical setting.
How a PACS System Works: The Four Core Pillars
To really get what a PACS system does, you have to look past the simple definition and peek under the hood at how it operates. At its heart, a PACS is a digital assembly line for medical images, built on four distinct but tightly connected pillars. Each one is essential for turning a raw scan into a powerful diagnostic tool that shapes patient care.
Let's break down how this all fits together, moving from the moment an image is created to the second a doctor views it.
Pillar 1: Image Acquisition
Everything starts at the source—the imaging equipment itself. We're talking about the MRI scanners, CT machines, ultrasound wands, and digital X-ray units that capture the initial images. In the PACS world, we call these pieces of equipment modalities.
When a scan is finished, the modality doesn't just spit out a simple JPEG. It creates a complex digital file, often made up of hundreds or even thousands of individual image slices. These files are generated in a universal format called DICOM (Digital Imaging and Communications in Medicine). Think of DICOM as the universal language for medical imaging; it’s what ensures a scan from a Siemens CT machine can be perfectly read by software from any other vendor. This standardization is absolutely critical.
Once that DICOM file is ready, the modality sends it straight to the central PACS server over a secure network. This first step is like a photographer taking a picture and instantly uploading it to a secure cloud, making it immediately available for the next stage.
Pillar 2: PACS Archive and Storage
The second pillar is the PACS archive, which acts as both the system's central brain and its long-term memory. This is far more than just a big hard drive. It's a highly organized, secure digital vault built to store millions of medical images and all their related data, effectively replacing the massive, dusty film libraries of the past.
To balance speed with cost, archives almost always use a tiered storage approach:
- Short-Term Storage: Recent scans or active patient studies are kept on incredibly fast, high-performance servers for instant access. When a radiologist pulls up a scan from earlier today, it comes from this tier.
- Long-Term Storage: Older images that aren't needed as often are moved to more affordable, high-capacity storage. While it might take a few extra seconds to retrieve these, this strategy is essential for managing the immense data footprint of a hospital's imaging history, which can easily swell into petabytes.
The PACS archive is more than just a digital closet; it's an intelligent database. It meticulously links every image to the correct patient record, the radiologist's report, and other crucial clinical data, ensuring a complete and organized history is always just a click away.
Pillar 3: The Clinical Workstation
If the archive is the brain, then the clinical workstation is the high-powered command center where the real diagnostic work gets done. This isn't your average desktop PC. It's a specialized, high-performance machine hooked up to one or more medical-grade, high-resolution monitors designed for spotting the tiniest details.
These workstations run sophisticated viewing software that gives radiologists and other specialists a suite of powerful tools. They can do much more than just look at a picture:
- Zoom, pan, and rotate 3D anatomical models.
- Adjust brightness and contrast to make subtle abnormalities pop.
- Take precise measurements of tumors, fractures, or other findings.
- Compare a patient's current scan side-by-side with previous exams to track changes over time.
This is the digital evolution of the old-school lightbox, supercharged with an incredible array of tools that help clinicians make faster, more accurate diagnoses.
Pillar 4: Secure Network and Distribution
The final pillar holding everything together is the secure network—the digital superhighway that connects all the other components. Medical imaging files are huge; a single CT or MRI study can be hundreds of megabytes. Because of this, the network has to be fast, reliable, and, above all, secure.
This network infrastructure handles moving images from the modalities to the archive. It then distributes them on demand to clinical workstations, sends them to the Electronic Health Record (EHR) system, or even beams them to a remote specialist for a teleradiology consult. To comply with patient privacy regulations like HIPAA, strong encryption and strict access controls are baked in, protecting sensitive data at every single point.
The infographic below shows how this all flows together, from the initial scan to centralized storage and on-demand viewing.
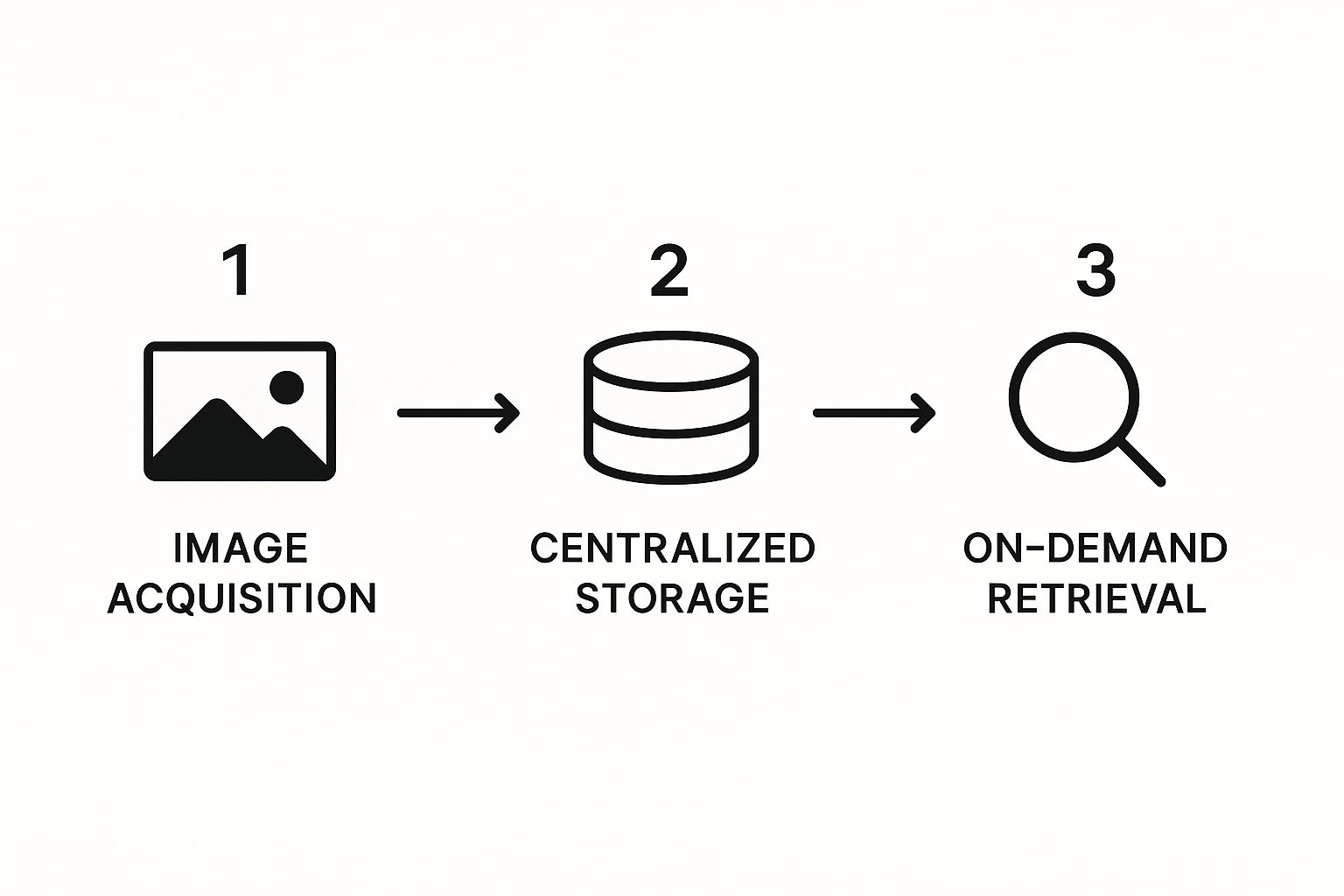
This visual really highlights how these four pillars work in sync to create a seamless and efficient cycle. Together, they form the robust foundation of any modern PACS, enabling the kind of fast, secure, and reliable communication that is non-negotiable in today's healthcare.
To really get a feel for what a modern Picture Archiving and Communication System (PACS) does, you have to rewind the clock. Before digital files and networks made everything instant, radiology was a completely different world—one filled with physical film, smelly chemicals, and massive libraries of patient records.

Picture a hospital basement lined with floor-to-ceiling shelves, all groaning under the weight of thousands of manila folders. Each of these "film jackets" held a patient's X-rays. When a doctor needed a prior exam for comparison, a file clerk had to physically hunt it down. This could take a few minutes, several hours, or if the film was misfiled or already checked out, it might not be found at all.
Need to get a specialist’s opinion across town? That wasn't just a click away. It meant packaging up the one-and-only original film and sending it by courier. This whole process was slow, clunky, and created constant bottlenecks that could delay a diagnosis. It was also expensive to maintain and carried the very real risk of films being lost or damaged in transit.
The Dawn of a Digital Idea
The first whispers of what would become a PACS system emerged in the early 1970s. The timing wasn't a coincidence; new digital imaging tools like CT scanners were just starting to appear. A few forward-thinkers saw the incredible potential of ditching physical film for electronic images.
But there was a huge roadblock. Each equipment manufacturer had its own proprietary system. They all spoke different digital languages. A CT scanner from one company couldn't talk to a viewing station from another. This digital "Tower of Babel" made the dream of a unified, interconnected system completely impossible.
The turning point: Before PACS could ever work, the medical world needed a universal translator. This desperate need for a common standard was the single biggest driver of the digital revolution in radiology.
The foundational work for this shift happened throughout the 1980s. Groups like the American College of Radiology (ACR) and the National Electrical Manufacturers Association (NEMA) teamed up to hammer out a common framework. Their early standards were critical first steps, but the real game-changer was still on the horizon.
DICOM: The Universal Language of Medical Imaging
That breakthrough moment finally came in 1993 with the introduction of the DICOM (Digital Imaging and Communications in Medicine) standard. This wasn't just another update; it was the key that unlocked the true power of digital medical imaging.
DICOM created a single, globally recognized rulebook for everything to do with a medical image:
- Image Data: How the pixels themselves are organized.
- Patient Information: A standard way to embed patient details directly into the file.
- Communication Protocols: A clear set of instructions for how to send and receive images across a network.
Suddenly, equipment from competing vendors could finally talk to each other. A GE scanner could send an exam to a Siemens workstation, which could then archive it on an Agfa server, all without a single hiccup. This seamless interoperability was the last piece of the puzzle. It made the Picture Archiving and Communication System a practical, scalable reality, setting the stage for the fast, efficient digital workflows we rely on in healthcare today.
For those interested, you can learn more about the complete history of medical imaging and see how this amazing collaboration between radiologists and engineers completely changed patient care.
What Are the Real-World Benefits of a PACS System?
It’s one thing to understand the technical nuts and bolts of a PACS, but it’s another thing entirely to see the impact it has on the ground. Moving away from film isn't just a simple tech upgrade; it’s a seismic shift that brings very real, tangible benefits to clinicians, hospital administrators, and, most importantly, the patients they serve. It smooths out clunky workflows, slashes costs, and helps doctors make better, faster decisions.
The first people to feel the difference are usually the radiologists and the physicians who refer patients for imaging. In the old days, a doctor might wait hours—or even days—for someone to track down a physical film and deliver it. Now, they have instant access to a patient's entire imaging history.
Imagine a cardiologist who needs to see if a patient's condition has worsened. They can pull up today's angiogram and instantly compare it side-by-side with one from two years ago. Seeing that complete story, that clear progression, is crucial for an accurate diagnosis.
A New Rhythm for Clinical Workflows
When hospitals first started switching to digital, a common worry was that the new technology would actually slow radiologists down. It turns out that fear was completely unfounded. The digital workflow doesn't just keep pace; it actually elevates the quality of care.
For instance, one large study analyzed over 5,500 radiology reports and found that the time it took to complete a report was basically the same after implementing PACS. But here’s what changed: radiologists could review a much larger number of historical images in the same amount of time. They were making more informed, context-rich decisions without losing speed—a perfect outcome for a busy hospital.
This move to digital imaging is a key piece of the puzzle in broader healthcare documentation automation efforts, making critical health data more accessible and efficient for everyone involved.
Clear Financial and Operational Wins
For the people managing the hospital's budget, the financial argument for PACS is rock-solid. The costs tied to physical film were massive, and they went far beyond just the price of the film itself.
Just think about all the expenses that simply vanish:
- Film and Chemicals: The endless cycle of buying expensive radiographic film and the hazardous chemicals for development? Gone.
- Physical Storage: Hospitals have reclaimed huge rooms that were once dedicated to dusty, overflowing film libraries. That space can now be used for patient care or other services that actually generate revenue.
- Staffing Costs: The army of file clerks needed to manage, retrieve, and courier films is no longer necessary. That staff can be reassigned to more valuable, patient-facing roles.
By taking the entire imaging process digital, a PACS turns what was once a major cost center into a lean, efficient operation. This frees up money that can be put back into what matters most: patient care.
Beyond just saving money, the system helps the whole department get more done. Radiologists can read studies from any secure workstation, whether they're in the hospital, at an outpatient clinic, or even at home. This makes it possible to balance workloads between different sites and opens the door for teleradiology services.
The Patient: The Ultimate Beneficiary
While the clinical and financial gains are impressive, the most important impact is always on the patient. At the end of the day, faster and more accurate diagnoses lead directly to better health outcomes.
When a patient is rushed to the ER after a car accident, a CT scan can be taken and read in minutes, not hours. That speed gives surgeons the information they need to act decisively, which can literally be the difference between life and death. For less urgent cases, it means less time spent worrying in a waiting room and a quicker start on the right treatment plan.
This table really highlights the night-and-day difference between the old way of doing things and the modern, patient-focused workflow that a PACS enables.
Film-Based Workflow vs. PACS-Based Workflow
| Feature | Traditional Film System | Modern PACS System |
|---|---|---|
| Image Access Time | Hours to days | Seconds to minutes |
| Collaboration | One person viewing a physical film at a time | Simultaneous, real-time access for multiple specialists anywhere |
| Image Quality | Prone to scratches, degradation, and chemical inconsistencies | Consistent, high-resolution digital quality with enhancement tools |
| Report Turnaround | Slow; depended on physical transport and manual steps | Fast; automated distribution to the EHR and referring physician |
| Data Integrity | High risk of lost or misfiled films | Secure, tracked, and backed-up digital archive with a full audit trail |
Ultimately, a PACS system closes the gap between imaging technology and hands-on patient care. It ensures that critical information gets to the right people quickly, securely, and reliably when they need it most.
7. The Future of PACS and Medical Imaging
The world of medical imaging isn't sitting still. What we think of as a PACS today is already changing, driven by the need for smarter, more connected tools that can keep up with the demands of modern healthcare. We're moving well beyond simple image storage and viewing. The future is about transforming the PACS into an intelligent hub that actively supports clinical decisions.

This evolution is happening in a rapidly growing market. Valued at roughly USD 3.12 billion in 2024, the global PACS market is expected to climb to USD 4.42 billion by 2030. This isn't just a number; it reflects a massive, worldwide push to digitize healthcare and weave PACS workflows into every aspect of patient care. You can explore the full research on the global PACS market to see the trends driving this growth.
Let's look at the key shifts making this future a reality.
The Rise of Cloud-Based PACS
One of the biggest game-changers is the move away from on-premise servers and into the cloud. For decades, hospitals had to build, manage, and cool enormous server rooms just to house their imaging data. This was not only expensive but also made it incredibly difficult to scale up or share information securely outside the hospital's network.
A Cloud-based PACS completely flips that script. It’s like ditching your personal DVD library for a Netflix subscription. Instead of owning and maintaining all the hardware, healthcare providers pay a service to manage their data securely in the cloud.
This brings some immediate, powerful benefits:
- Scalability on Demand: Need more storage? It's available instantly, without having to purchase and install new physical servers.
- Remote Accessibility: Radiologists and specialists can securely view images from their homes, a different clinic, or anywhere with an internet connection. This is the engine behind the growth of teleradiology.
- Reduced IT Burden: The cloud vendor takes care of maintenance, security, and backups. This frees up the hospital's internal IT team to work on other critical projects.
AI Integration: The Radiologist's Second Set of Eyes
Artificial intelligence (AI) is quickly becoming a non-negotiable part of the modern PACS. These AI algorithms are trained on millions of medical images, learning to spot patterns and potential issues that are sometimes too subtle for the human eye to detect on a first pass. It’s not about replacing radiologists—it’s about giving them an incredibly powerful assistant.
An AI-powered PACS can act like a digital triage nurse for the radiologist. It can analyze an incoming study, flag it for potential critical findings, and automatically move it to the top of a busy worklist.
Imagine an AI tool that scans a chest X-ray, detects a tiny, suspicious nodule, and highlights it for immediate attention. This ensures that the most urgent cases get read first, improving diagnostic accuracy and, ultimately, patient outcomes.
Vendor Neutral Archives for Long-Term Freedom
Another crucial innovation is the Vendor Neutral Archive (VNA). For years, hospitals were handcuffed to their PACS vendor. If you wanted to switch to a new system, you faced the nightmare of migrating a massive, proprietary archive of historical images—a task so complex and costly it was often impossible.
A VNA breaks these chains by creating a standardized, independent storage layer that is separate from the PACS viewing software. It’s a central vault that can communicate with any PACS or viewer, regardless of the manufacturer.
This gives healthcare organizations the freedom to choose the best viewing tools for their needs or switch PACS vendors without holding their data hostage. It's a strategic move that ensures long-term flexibility and future-proofs an institution's entire imaging infrastructure.
Common Questions About PACS Technology
As with any specialized technology, a few common questions always pop up about PACS. Answering these helps paint a clearer picture of how these systems fit into the day-to-day reality of a hospital or clinic and handle crucial tasks like keeping patient data safe. Let's tackle some of the most frequent ones.
How Is PACS Different From an EHR?
Think of it this way: a PACS and an Electronic Health Record (EHR) are like two different specialists on a patient's care team. They have separate jobs but work together constantly.
- The EHR (Electronic Health Record) is the patient's master digital file. It’s where you'll find all the text-based information—doctor's notes, lab results, prescriptions, and allergy lists.
- A PACS (Picture Archiving and Communication System) has one highly specialized job: managing the massive files that make up medical images.
These two systems are designed to communicate, not compete. A doctor reading a radiologist's written report in the EHR can typically click a link that instantly opens the actual X-ray or MRI from the PACS. This gives them the complete story—the expert interpretation alongside the visual evidence.
Is Patient Data Secure on a PACS System?
Absolutely. Security isn't just a feature; it's the bedrock of any modern PACS. These systems are built from the ground up to comply with strict regulations like HIPAA (Health Insurance Portability and Accountability Act).
A core security philosophy in PACS is the principle of "least privilege." This means every user gets only the bare minimum access they need to do their job, dramatically reducing the risk of unauthorized data exposure.
This is enforced through several layers of protection. Users need unique credentials to log in, and their access is strictly defined by their role. For example, a radiologist can view and diagnose images, while a system administrator might only have permission to manage user accounts without seeing any patient data. On top of that, all image data is encrypted, both when it's sitting in the archive and when it's being sent across the network.
Can Any Doctor Access Any Patient Image?
No, and for good reason. Access is very carefully controlled and tracked to protect patient confidentiality. A PACS works on a strict "need-to-know" basis.
A doctor's ability to pull up a study depends entirely on their role and their direct connection to a patient's care. An ER physician, for instance, will have immediate access to the CT scans of a trauma patient just wheeled in. However, that same physician can't just browse the imaging history of a patient in the oncology wing they have no connection to. This role-based access control is a fundamental safeguard that keeps private health information private.
At PYCAD, we specialize in integrating advanced AI to enhance the capabilities of medical imaging systems. If you're looking to optimize diagnostic accuracy and operational efficiency, explore our solutions at https://pycad.co.






