Welcome to the Medical Imaging Data Scientist Interview Questions resource! This valuable compilation aims to assist both interviewers and candidates in preparing for job interviews within the rapidly evolving field of medical imaging and data science. As the healthcare industry increasingly relies on data-driven insights, there is a growing demand for skilled data scientists who can effectively work with medical imaging data.
Within this resource, you will find a comprehensive collection of interview questions covering a wide range of topics relevant to medical imaging and data science. These questions delve into fundamental concepts, techniques, and challenges in the field, as well as touch on ethical considerations and best practices.
Please note that while this compilation is not exhaustive, it serves as an excellent starting point to facilitate productive discussions during interviews. We strongly encourage users to contribute by suggesting improvements or adding new questions, thereby enriching this valuable resource.
Wishing you the best of luck as you embark on your interview journey in this exciting and ever-expanding field!
Q1: What is medical imaging and why is it important in healthcare?
Medical imaging refers to the process of creating visual representations of the interior of a body for clinical analysis and medical intervention. It encompasses a wide range of techniques, including X-rays, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and nuclear medicine, among others.
Medical imaging is crucial in healthcare for several reasons:
- Diagnosis: Medical imaging helps physicians identify and diagnose various health conditions, such as tumors, fractures, infections, and organ abnormalities, by providing a detailed view of the body’s internal structures.
- Treatment planning: It allows healthcare professionals to develop personalized treatment plans based on a patient’s specific condition and the location of the affected areas.
- Monitoring: Medical imaging enables doctors to monitor the progress of a treatment or intervention, assess its effectiveness, and make necessary adjustments.
- Screening: In some cases, medical imaging is used for early detection and prevention, such as mammography for breast cancer or CT scans for lung cancer screening in high-risk populations.
- Guidance: Medical imaging plays a critical role in guiding medical procedures, such as surgeries and biopsies, by providing real-time visual information that helps ensure accurate and precise interventions.
By offering a non-invasive and accurate way to visualize and assess the human body’s internal structures, medical imaging has become an indispensable tool in modern healthcare. It contributes significantly to improved patient care, more accurate diagnoses, and better treatment outcomes.
Q2: What are the different types of medical imaging techniques? Explain each briefly.
There are several types of medical imaging techniques, each with its specific applications and benefits. Here’s a brief explanation of some of the most common techniques:
- X-ray: X-ray imaging, or radiography, uses ionizing radiation to produce images of the body’s internal structures. It is particularly useful for visualizing bones and detecting fractures, infections, or tumors. X-rays can also be used to examine the chest and diagnose lung conditions like pneumonia or lung cancer.
- Computed Tomography (CT): CT scans use a series of X-ray images taken from different angles to create detailed cross-sectional images (slices) of the body. CT scans can visualize bones, soft tissues, and blood vessels, making them valuable for diagnosing and monitoring various conditions, such as tumors, internal bleeding, or head injuries.
- Magnetic Resonance Imaging (MRI): MRI uses powerful magnets and radiofrequency waves to generate detailed images of the body’s internal structures without ionizing radiation. It is particularly useful for visualizing soft tissues, such as the brain, spinal cord, muscles, and organs. MRI can help diagnose and monitor various neurological, musculoskeletal, and cardiovascular conditions.
- Ultrasound: Ultrasound imaging, or sonography, uses high-frequency sound waves to create real-time images of the body’s internal structures. It is a safe, non-invasive, and radiation-free technique often used for examining the fetus during pregnancy, diagnosing conditions in the abdomen and pelvis, and guiding needle biopsies.
- Nuclear Medicine: Nuclear medicine involves the use of small amounts of radioactive materials, or radiotracers, to examine the body’s functions and molecular processes. Techniques like Positron Emission Tomography (PET) and Single-Photon Emission Computed Tomography (SPECT) provide functional information and help diagnose, stage, and monitor diseases such as cancer, heart disease, and neurological disorders.
- Mammography: Mammography is a specialized type of X-ray imaging specifically designed for examining breast tissue. It is widely used for early detection and diagnosis of breast cancer and assessing breast abnormalities.
- Fluoroscopy: Fluoroscopy is a real-time X-ray imaging technique that allows healthcare professionals to observe the movement of body structures or instruments within the body during procedures, such as angiography, gastrointestinal exams, or catheter placements.
These are just a few examples of the many medical imaging techniques available today. Each technique has its unique strengths and limitations, and the choice of imaging modality depends on the specific clinical situation and the information needed for accurate diagnosis and treatment planning.
Q3: How do you handle missing or corrupted data in a dataset?
Handling missing or corrupted data is a crucial aspect of data preprocessing in any data science project, including medical imaging. Here are some common strategies to address this issue:
- Data imputation: Imputation is the process of estimating missing or corrupted data based on the available data. Common imputation methods include mean, median, or mode imputation, as well as more advanced techniques like k-nearest neighbors (k-NN) or regression imputation. The choice of imputation method depends on the nature of the data and the underlying assumptions about the missingness mechanism.
- Data deletion: If the proportion of missing or corrupted data is small and randomly distributed, you can consider deleting the affected instances (row deletion) or features (column deletion). However, this approach may lead to loss of valuable information, especially when the data is not missing at random or the proportion of missing data is significant.
- Interpolation: In time series or spatial data, missing values can be estimated by interpolating neighboring data points. Various interpolation methods, such as linear, polynomial, or spline interpolation, can be used depending on the data’s nature and structure.
- Data augmentation: In some cases, missing or corrupted data can be replaced or augmented by generating new data points based on the available data. This approach can be particularly useful in medical imaging, where data augmentation techniques such as rotation, scaling, or flipping can create new, valid images to compensate for the missing or corrupted data.
- Model robustness: Building models that can handle missing or corrupted data directly is another approach. Some machine learning algorithms, such as decision trees or random forests, can inherently handle missing values by splitting the data based on the presence or absence of a particular feature. Additionally, you can leverage techniques like robust regression or robust PCA to build models that are less sensitive to data corruption.
- Domain expertise: In some cases, domain knowledge can help identify plausible values for missing or corrupted data or guide the choice of an appropriate imputation method.
- Data quality assessment: It’s crucial to assess the impact of missing or corrupted data on the model’s performance and validity. Techniques like cross-validation, sensitivity analysis, or performance metrics can help evaluate the effectiveness of different data handling strategies.
Handling missing or corrupted data requires a careful evaluation of the dataset’s characteristics, the missingness mechanism, and the potential impact on the analysis. A combination of the above strategies may be necessary to achieve the best results in different situations.
Q4: What is DICOM? Explain its significance in medical imaging.
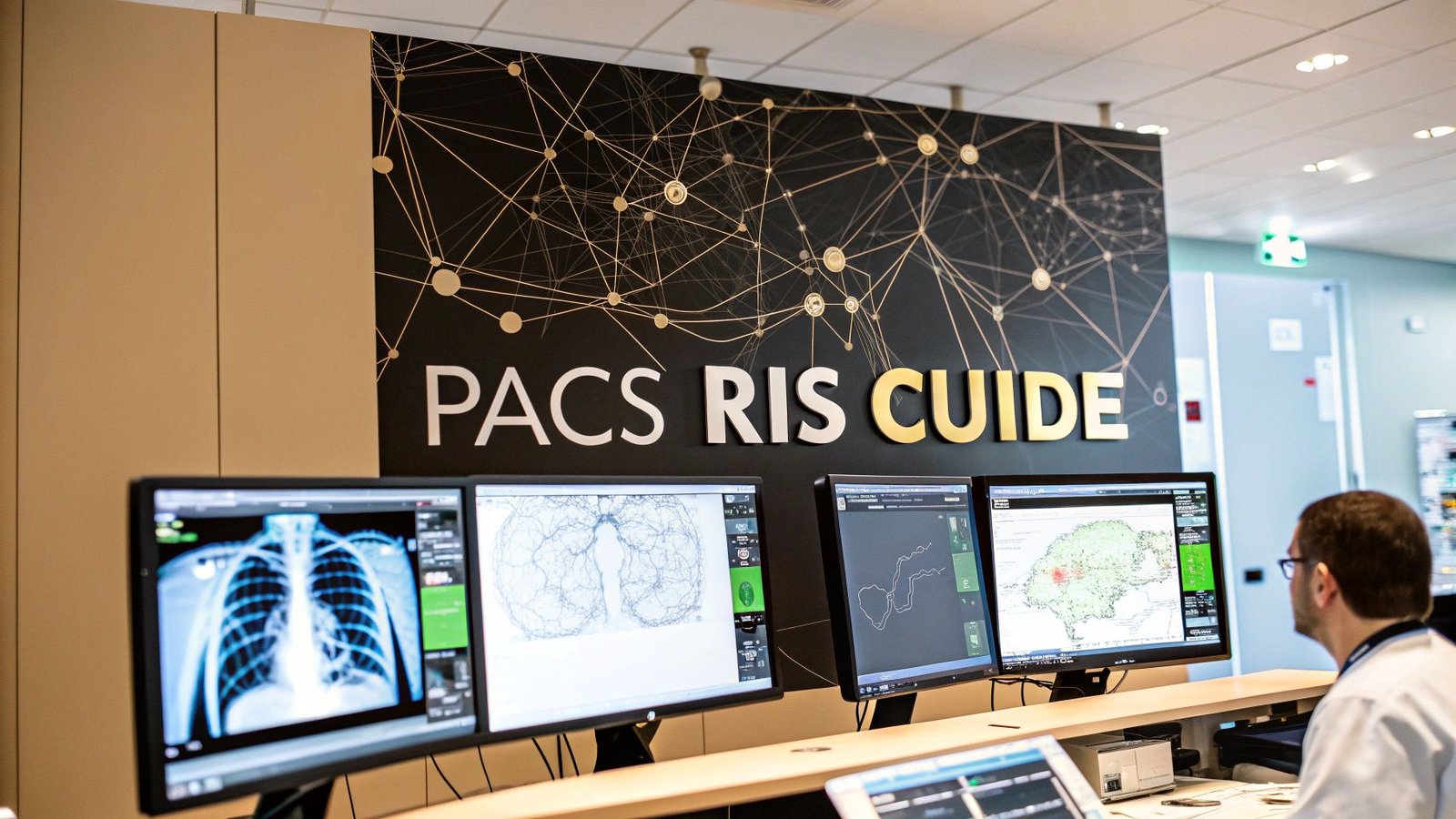
DICOM (Digital Imaging and Communications in Medicine) is a standard for transmitting, storing, retrieving, and sharing medical images and related information. Developed by the National Electrical Manufacturers Association (NEMA) and the American College of Radiology (ACR), DICOM is widely used in medical imaging to ensure interoperability between different imaging devices, PACS (Picture Archiving and Communication Systems), and healthcare information systems.
DICOM has several significant benefits in medical imaging:
- Interoperability: DICOM allows images and associated metadata produced by different manufacturers’ imaging devices (such as CT, MRI, or X-ray machines) to be seamlessly shared, viewed, and processed by other devices or software applications, regardless of the vendor.
- Standardization: DICOM provides a consistent structure for organizing and encoding medical images and associated information, such as patient demographics, imaging modality, and technical parameters. This standardization simplifies data management, exchange, and analysis across different healthcare systems and institutions.
- Data integrity: DICOM ensures the integrity and consistency of medical images and related information by defining specific rules for data encoding, compression, and transmission. This ensures that the image quality and diagnostic information are preserved during transfer and storage.
- Extensibility: DICOM is designed to be flexible and extensible, allowing it to evolve and accommodate new imaging modalities, data formats, and communication protocols as the field of medical imaging advances.
- Image processing and analysis: DICOM compatibility enables the use of various specialized software tools for processing and analyzing medical images, such as image segmentation, registration, or computer-aided diagnosis.
- Data security: DICOM incorporates various security measures, such as secure communication protocols and data encryption, to protect patient privacy and ensure the confidentiality of medical information.
Overall, DICOM plays a critical role in modern medical imaging by providing a standardized, interoperable, and secure framework for managing and exchanging medical images and related information. It enables more efficient and streamlined communication between different healthcare systems and devices, facilitates advanced image processing and analysis, and helps ensure patient privacy and data security.
Q5: Explain the concepts of precision, recall, and F1 score in the context of medical image analysis.
Precision, recall, and F1 score are performance metrics used to evaluate the effectiveness of classification models, including those applied to medical image analysis tasks like tumor detection, lesion segmentation, or disease classification. These metrics provide insights into the model’s accuracy, sensitivity, and overall performance.
- Precision: Precision (also known as positive predictive value) measures the proportion of true positive predictions (correctly identified cases) among all positive predictions made by the model. In the context of medical image analysis, precision indicates how many of the detected abnormalities are actual true abnormalities.Precision = (True Positives) / (True Positives + False Positives)High precision means that when the model predicts a positive case (e.g., a tumor), it is likely to be correct. However, precision does not account for false negatives (missed cases), which can be critical in medical imaging applications.
- Recall: Recall (also known as sensitivity or true positive rate) measures the proportion of true positive predictions among all actual positive cases in the dataset. In medical image analysis, recall indicates how many of the true abnormalities were correctly detected by the model.Recall = (True Positives) / (True Positives + False Negatives)High recall means that the model is effective at identifying positive cases (e.g., tumors) in the dataset. However, recall does not account for false positives (incorrect positive predictions), which can also be important in medical imaging applications.
- F1 score: The F1 score is the harmonic mean of precision and recall, providing a single metric that balances both false positives and false negatives. It is particularly useful when dealing with imbalanced datasets, as is often the case in medical imaging, where positive cases (e.g., tumors) might be rare compared to negative cases (healthy tissue).F1 score = 2 * (Precision * Recall) / (Precision + Recall)A high F1 score indicates that the model achieves a good balance between precision and recall, minimizing both false positives and false negatives. This is crucial in medical image analysis, where both types of errors can have significant clinical consequences.
When evaluating medical image analysis models, it is essential to consider precision, recall, and F1 score in conjunction with other performance metrics, such as accuracy, specificity, and area under the receiver operating characteristic (ROC) curve, to obtain a comprehensive understanding of the model’s performance and suitability for a given task.
Q6: How do you handle class imbalance in medical imaging datasets?
Class imbalance is a common issue in medical imaging datasets, where one class (e.g., healthy tissue) may be significantly more prevalent than another class (e.g., tumors or lesions). Handling class imbalance is crucial because it can lead to biased models that favor the majority class, resulting in poor performance on the minority class, which is often the class of interest. Here are some strategies to address class imbalance in medical imaging datasets:
- Resampling: Modify the dataset by oversampling the minority class, undersampling the majority class, or a combination of both. Oversampling can be done by duplicating instances from the minority class or generating synthetic examples using techniques like SMOTE (Synthetic Minority Over-sampling Technique). Undersampling involves removing instances from the majority class, either randomly or using some sampling strategy (e.g., Tomek links or neighborhood cleaning rule).
- Data augmentation: Augment the minority class by creating new instances using various image transformations, such as rotations, translations, scaling, or flipping. This approach can increase the diversity of the minority class examples, leading to more robust models.
- Weighted loss function: Assign higher weights to the minority class during the training process. This approach penalizes misclassifications of the minority class more severely, encouraging the model to pay more attention to these instances.
- Cost-sensitive learning: Modify the learning algorithm to incorporate class imbalance explicitly. In cost-sensitive learning, each misclassification is assigned a cost, and the learning algorithm aims to minimize the total cost. Higher costs are assigned to misclassifying the minority class, emphasizing the importance of correctly classifying these instances.
- Transfer learning: Leverage pre-trained models, such as deep neural networks, that have been trained on large, balanced datasets. By fine-tuning the pre-trained model on the imbalanced dataset, you can benefit from the learned features and mitigate the impact of class imbalance.
- Ensemble methods: Use ensemble techniques, such as bagging, boosting, or random under-sampling boosting (RUSBoost), to improve classification performance on imbalanced datasets. Ensemble methods can help reduce the bias towards the majority class by combining multiple base classifiers, each trained on a different subset of the data or with different sampling strategies.
- Evaluation metrics: Use appropriate evaluation metrics, such as precision, recall, F1 score, or area under the receiver operating characteristic (ROC) curve, that consider both false positives and false negatives. These metrics can provide a more comprehensive understanding of the model’s performance on imbalanced datasets than accuracy alone.
Handling class imbalance in medical imaging datasets requires a combination of these strategies, depending on the specific dataset and the desired classification performance. It is essential to carefully evaluate the impact of each strategy on the model’s performance and choose the most suitable approach for a given task.
Q7: What is the role of convolutional neural networks (CNNs) in medical image analysis?
Convolutional neural networks (CNNs) are a class of deep learning models designed to process grid-like data, such as images. They have shown exceptional performance in various image analysis tasks, including classification, segmentation, and object detection. In medical image analysis, CNNs play a significant role in automating the detection, diagnosis, and prognosis of various medical conditions by processing and analyzing medical images. Some key roles of CNNs in medical image analysis include:
- Image classification: CNNs can be used to classify medical images into different categories, such as normal vs. abnormal, or to identify specific diseases, such as pneumonia or diabetic retinopathy. By learning complex patterns and features from the images, CNNs can achieve high classification accuracy, aiding in the diagnosis process.
- Image segmentation: CNNs can be used for image segmentation tasks, such as delineating the boundaries of tumors, blood vessels, or organs in medical images. By capturing the spatial relationships between pixels, CNNs can accurately segment regions of interest, providing valuable information for treatment planning and monitoring.
- Object detection: CNNs can detect and localize multiple objects or regions of interest within a single medical image, such as nodules in a lung CT scan or lesions in a mammogram. This capability enables the identification and quantification of abnormalities, assisting in early detection and diagnosis of various conditions.
- Image registration: CNNs can be used to align and register medical images from different modalities or time points, allowing for a more comprehensive view of a patient’s anatomy and changes over time. This is particularly useful in tasks like monitoring disease progression or evaluating the effectiveness of treatments.
- Image synthesis: CNNs can be employed to generate synthetic medical images or to transform images between different modalities, such as converting an MRI scan to a CT scan. This can be useful for data augmentation, training models with limited data, or simulating images for treatment planning.
- Feature extraction: CNNs can automatically learn and extract high-level features from medical images, capturing complex patterns and structures. These features can be used as input for other machine learning algorithms, such as support vector machines or random forests, to improve their performance in classification or regression tasks.
In summary, convolutional neural networks play a critical role in medical image analysis by automating various tasks that traditionally required manual intervention from experts. By accurately detecting, classifying, and quantifying medical conditions from images, CNNs can assist healthcare professionals in making more informed decisions, ultimately leading to improved patient care and outcomes.
Q8: Explain the concept of transfer learning and its relevance in medical imaging tasks.
Transfer learning is a machine learning technique that leverages knowledge acquired from one task or domain (source) to improve the performance of a model on a different but related task or domain (target). In the context of deep learning, transfer learning typically involves using pre-trained neural networks, often trained on large, general-purpose datasets, as a starting point for training a model on a specific task or dataset.
Transfer learning is particularly relevant in medical imaging tasks for the following reasons:
- Limited labeled data: Medical imaging datasets often have a limited number of labeled examples, due to factors such as privacy concerns, data acquisition costs, or the need for expert annotation. Transfer learning can help overcome this limitation by leveraging the features learned from a large, pre-trained network, thereby reducing the need for extensive labeled data in the target task.
- Model performance: Pre-trained neural networks have already learned a variety of low-level features (e.g., edges, textures) and high-level features (e.g., shapes, patterns) from large-scale datasets. By fine-tuning these networks on the target medical imaging task, it is possible to achieve better performance compared to training a model from scratch, as the pre-trained network has already learned generalizable features that can be adapted to the specific task.
- Training efficiency: Transfer learning can significantly reduce the time and computational resources required to train a deep learning model for medical imaging tasks. By initializing the model with the pre-trained network’s weights, the training process can converge faster, requiring fewer iterations and less training data.
- Reduced overfitting: Using a pre-trained network as a starting point can help reduce the risk of overfitting, especially when dealing with limited training data. The pre-trained network has already learned generalizable features from a large dataset, and fine-tuning on the target task can make the model more robust and less prone to overfitting.
- Cross-modality learning: Transfer learning can be used to adapt a model trained on one imaging modality (e.g., natural images) to another modality (e.g., MRI or CT scans) by fine-tuning the pre-trained network on the target modality’s data. This can be useful in situations where labeled data is scarce or unavailable for a specific modality.
In summary, transfer learning is highly relevant in medical imaging tasks as it enables more efficient training, improved model performance, and reduced overfitting, especially in situations where labeled data is limited or scarce. By leveraging the knowledge acquired from pre-trained networks, transfer learning can help develop more accurate and robust models for various medical imaging applications.
Q9: What is the difference between supervised, unsupervised, and semi-supervised learning?
These three terms represent different learning paradigms in machine learning, each with its distinct approach to learning from data.
- Supervised learning: In supervised learning, the model is trained on a labeled dataset, which contains both input features and corresponding output labels (or target values). The goal is to learn a mapping from the input features to the output labels so that the model can make accurate predictions for new, unseen data. Supervised learning is widely used for tasks such as classification (e.g., categorizing images into different classes) and regression (e.g., predicting continuous values like house prices).Key aspects of supervised learning:
- Requires a labeled dataset (input-output pairs).
- Learns a mapping from input features to output labels.
- Commonly used for classification and regression tasks.
2. Unsupervised learning: In unsupervised learning, the model is trained on an unlabeled dataset, which contains input features but no output labels. The goal is to discover underlying patterns or structures in the data without any guidance from labeled examples. Unsupervised learning is often used for tasks such as clustering (e.g., grouping similar data points together) and dimensionality reduction (e.g., reducing the number of features while preserving important information).Key aspects of unsupervised learning:
- Requires an unlabeled dataset (input features only).
- Discovers patterns or structures in the data without guidance from labels.
- Commonly used for clustering and dimensionality reduction tasks.
3. Semi-supervised learning: Semi-supervised learning is a hybrid approach that combines elements of both supervised and unsupervised learning. The model is trained on a dataset that contains a mix of labeled and unlabeled data, with the majority often being unlabeled. The goal is to leverage both the labeled data for learning the input-output mapping and the unlabeled data for discovering underlying structures, ultimately improving the model’s performance compared to using only the labeled data. Semi-supervised learning is particularly useful when labeled data is scarce or expensive to obtain.Key aspects of semi-supervised learning:
- Requires a mix of labeled and unlabeled data.
- Combines aspects of supervised and unsupervised learning.
- Useful when labeled data is scarce or expensive to acquire.
In summary, the main difference between supervised, unsupervised, and semi-supervised learning lies in the type of data they require and the learning objectives they pursue. Supervised learning focuses on learning input-output mappings from labeled data, unsupervised learning aims to discover patterns or structures in unlabeled data, and semi-supervised learning combines both approaches to leverage the advantages of each, especially when labeled data is limited.
Q10: What are some common preprocessing techniques used in medical image analysis?
Preprocessing is a crucial step in medical image analysis, as it helps to standardize and enhance the quality of the input images, ultimately improving the performance of subsequent analysis tasks. Some common preprocessing techniques used in medical image analysis include:
- Resizing and resampling: Medical images can have varying resolutions and dimensions. Resizing and resampling the images to a consistent size or spacing is essential for ensuring compatibility with analysis algorithms, especially deep learning models, which often require fixed input dimensions.
- Intensity normalization: Medical images may exhibit varying intensity ranges and contrasts due to differences in acquisition protocols or devices. Intensity normalization scales the pixel values to a standard range, such as [0, 1] or [0, 255], enhancing the contrast and enabling more meaningful comparisons between images.
- Histogram equalization: This technique improves the contrast of images by spreading the intensity values more evenly across the entire range. Histogram equalization can enhance the visibility of subtle structures and improve the performance of image segmentation and feature extraction algorithms.
- Noise reduction: Medical images can be affected by various types of noise, such as Gaussian noise, salt-and-pepper noise, or speckle noise. Noise reduction techniques, such as Gaussian filtering, median filtering, or anisotropic diffusion, can help remove or reduce noise while preserving important image features.
- Image registration: In some cases, it is necessary to align and register medical images from different modalities (e.g., MRI and CT) or time points (e.g., pre- and post-treatment). Image registration techniques, such as rigid, affine, or deformable registration, can help to align the images, allowing for more accurate comparisons and analyses.
- Segmentation: Preprocessing may involve segmenting regions of interest (ROIs) in the images, such as tumors, organs, or blood vessels, to focus the analysis on these specific areas. Segmentation techniques can range from simple thresholding methods to more complex approaches like active contours or deep learning-based methods.
- Data augmentation: To increase the diversity and size of the training dataset, data augmentation techniques can be applied to create new instances of images by applying various transformations, such as rotations, translations, scaling, or flipping. This can help improve the robustness and generalization of machine learning models, especially in situations with limited data.
- Feature extraction: In some cases, preprocessing may involve extracting relevant features from the images, such as texture, shape, or intensity descriptors. These features can then be used as inputs for machine learning algorithms, particularly in cases where deep learning models may not be feasible or appropriate.
The choice of preprocessing techniques depends on the specific medical image analysis task, the characteristics of the input images, and the desired outcomes. Careful selection and application of preprocessing techniques can significantly improve the quality of the input images and enhance the performance of subsequent analysis algorithms.
Q11: Describe the process of data augmentation and why it’s important in medical image analysis.
Data augmentation is a technique used to increase the size and diversity of a training dataset by creating new instances through the application of various transformations to the original data. In the context of medical image analysis, data augmentation typically involves applying image transformations, such as rotations, translations, scaling, flipping, or elastic deformations, to generate new, altered versions of the original medical images.
Data augmentation is important in medical image analysis for several reasons:
- Limited data: Medical imaging datasets often have a limited number of samples, as acquiring and annotating medical images can be time-consuming, costly, and subject to privacy concerns. Data augmentation helps to artificially expand the size of the dataset, making it more suitable for training machine learning models, particularly deep learning models, which often require large amounts of data to achieve good performance.
- Variability: Medical images can exhibit a wide range of variability due to differences in patient anatomy, imaging modalities, and acquisition protocols. Data augmentation helps introduce additional variability into the training dataset, allowing the model to learn more robust and generalizable features that can better handle variations in real-world data.
- Overfitting: When training data is limited, machine learning models, especially deep learning models, are prone to overfitting, where the model learns to perform well on the training data but fails to generalize to unseen data. Data augmentation helps mitigate overfitting by increasing the diversity of the training data, forcing the model to learn more general features and making it less likely to memorize specific training examples.
- Imbalanced data: Medical imaging datasets often suffer from class imbalance, where one class (e.g., healthy tissue) is significantly more prevalent than another class (e.g., tumors). Data augmentation can be used to balance the dataset by generating more instances of the underrepresented class, reducing the risk of biased models that favor the majority class.
The process of data augmentation in medical image analysis typically involves the following steps:
- Select transformations: Choose appropriate image transformations based on the specific medical imaging task and the nature of the data. Common transformations include rotation, translation, scaling, flipping, and elastic deformation. It is essential to ensure that the chosen transformations maintain the clinical relevance and integrity of the medical images.
- Apply transformations: Apply the selected transformations to the original images in the dataset, generating new, altered instances. This process can be performed offline, creating an expanded dataset before training, or online, applying the transformations on-the-fly during the training process.
- Train the model: Use the augmented dataset to train the machine learning model, allowing it to learn more robust and generalizable features from the increased size and diversity of the data.
In summary, data augmentation is a crucial technique in medical image analysis that helps address challenges such as limited data, variability, overfitting, and class imbalance. By creating new instances through the application of image transformations, data augmentation can improve the robustness and generalization of machine learning models, ultimately leading to better performance in medical image analysis tasks.
Q12: What is image segmentation? Explain its significance in medical imaging.
Image segmentation is the process of dividing an image into multiple regions or segments, each of which consists of a group of pixels with similar characteristics or properties. The goal is to separate objects or regions of interest (ROIs) from the background or other objects in the image, simplifying the image for further analysis or interpretation.
In the context of medical imaging, image segmentation plays a crucial role in various applications, such as:
- Quantitative analysis: Segmentation enables the quantification of anatomical structures, lesions, or abnormalities in medical images, such as measuring the size, volume, or shape of tumors, organs, or blood vessels. This information can be valuable for diagnosis, treatment planning, and monitoring of disease progression.
- Visualization: Segmentation can improve the visualization of medical images by highlighting specific regions or structures of interest, making it easier for clinicians to interpret the images and identify abnormalities.
- Image-guided interventions: In image-guided surgery or therapy, segmentation is used to delineate anatomical structures or target regions, providing guidance for the intervention and helping to minimize damage to surrounding healthy tissue.
- Treatment planning: In radiation therapy or other treatments, segmentation of organs, tumors, or other structures is essential for determining the appropriate dose distribution and planning the treatment to maximize therapeutic effects while minimizing side effects.
- Computer-aided diagnosis: Segmentation is often a prerequisite for computer-aided diagnosis systems, which use the segmented regions or structures to automatically detect, classify, or assess abnormalities in medical images.
Various image segmentation techniques can be applied to medical imaging tasks, ranging from traditional methods like thresholding, region growing, or edge detection, to more advanced approaches like active contours or level sets. In recent years, deep learning-based methods, particularly convolutional neural networks (CNNs) and their variants, have shown significant success in medical image segmentation tasks, often outperforming traditional methods in terms of accuracy and efficiency.
In summary, image segmentation is a critical step in medical imaging, enabling the extraction of meaningful information from complex images and supporting various applications, such as quantitative analysis, visualization, image-guided interventions, treatment planning, and computer-aided diagnosis. The choice of segmentation technique depends on the specific medical imaging task and the desired outcomes, with deep learning-based methods emerging as a promising approach for many applications.
Q13: Describe the role of edge detection in medical image analysis.
Edge detection is an image processing technique that identifies the boundaries or edges between different regions in an image. These boundaries typically correspond to areas where there is a significant change in pixel intensity or color, indicating a transition between different objects or structures. In medical image analysis, edge detection plays an important role in various tasks, such as:
- Image segmentation: Edge detection can be used as a precursor to or part of segmentation algorithms, helping to separate regions of interest (ROIs), such as organs, tissues, or lesions, from the background or other structures in the image. By identifying the boundaries between different regions, edge detection can aid in defining the shapes and outlines of the objects or structures of interest.
- Feature extraction: Edge information can be used as a feature for machine learning algorithms, particularly in tasks where the boundaries between structures are relevant, such as organ or tumor boundary delineation. By capturing the local changes in intensity or color, edge features can provide valuable information about the structure and geometry of the objects in the image.
- Image enhancement: Edge detection can be used to improve the visibility of structures in medical images, especially in cases where the edges are weak or blurred. By emphasizing the boundaries between different regions, edge detection can help enhance the overall contrast and clarity of the image, making it easier for clinicians to interpret and analyze the image.
- Registration: In medical image registration tasks, where the goal is to align multiple images (e.g., from different time points or modalities), edge information can be used as a feature to guide the registration process. By matching the edges in the images, the registration algorithm can achieve a more accurate and robust alignment of the structures of interest.
Various edge detection techniques can be applied to medical image analysis, ranging from simple gradient-based methods, such as the Sobel or Prewitt operators, to more advanced techniques, such as the Canny edge detector or the Laplacian of Gaussian (LoG) operator. Some deep learning-based methods, such as convolutional neural networks (CNNs), can also implicitly learn to detect edges as part of their feature extraction process.
In summary, edge detection plays a significant role in medical image analysis, contributing to tasks such as image segmentation, feature extraction, image enhancement, and registration. By identifying the boundaries between different regions or structures, edge detection can provide valuable information about the geometry and organization of the objects in the image, supporting various clinical applications and improving the overall quality of the image analysis.
Q14: What are some common challenges faced in medical image analysis?
Medical image analysis is a complex and critical task, as it often deals with high-dimensional and heterogeneous data, and its outcomes can significantly impact diagnosis, treatment, and patient care. Some common challenges faced in medical image analysis include:
- Data quality: Medical images can be affected by various factors, such as noise, artifacts, low resolution, or poor contrast, which can hinder the visibility of structures or features and make the analysis more challenging.
- Limited data: Acquiring and annotating medical images can be time-consuming, expensive, and subject to privacy concerns. As a result, medical image datasets are often limited in size, which can make it difficult to train and evaluate machine learning models, particularly deep learning models that typically require large amounts of data.
- Variability: Medical images can exhibit a wide range of variability due to differences in patient anatomy, imaging modalities, acquisition protocols, or devices. This variability can make it challenging to develop robust and generalizable analysis algorithms that can handle the diverse range of real-world data.
- Class imbalance: Medical imaging datasets often suffer from class imbalance, where one class (e.g., healthy tissue) is significantly more prevalent than another class (e.g., tumors). This imbalance can lead to biased models that favor the majority class, resulting in poor performance on the underrepresented class.
- Segmentation: Accurate segmentation of regions of interest (ROIs), such as tumors, organs, or blood vessels, is often a crucial step in medical image analysis. However, segmentation can be challenging due to factors such as overlapping structures, weak boundaries, or similar intensities between the target region and surrounding tissue.
- Registration: Aligning and registering medical images from different modalities (e.g., MRI and CT) or time points (e.g., pre- and post-treatment) can be difficult due to differences in image characteristics, such as intensity, resolution, or contrast, as well as potential deformations or changes in the patient’s anatomy.
- Interpretability: Machine learning models, especially deep learning models, can be highly complex and difficult to interpret, making it challenging to understand the underlying features or decision-making processes of the models. This lack of interpretability can be a barrier to clinical adoption, as clinicians need to trust and understand the analysis results to make informed decisions.
- Computational resources: Medical image analysis, particularly deep learning-based methods, can be computationally intensive, requiring significant processing power, memory, and storage resources. This can be a challenge, especially in resource-constrained settings or when working with large-scale or high-resolution medical images.
- Validation: Validating the performance and reliability of medical image analysis algorithms can be challenging due to the limited availability of annotated data and the need for expert validation. In addition, the performance metrics used for evaluation should be carefully chosen and clinically relevant to ensure that the algorithms are suitable for the intended application.
Addressing these challenges often requires the development of innovative and robust analysis algorithms, careful selection of preprocessing and data augmentation techniques, and close collaboration between computer scientists, clinicians, and other stakeholders to ensure that the algorithms are clinically relevant, interpretable, and applicable to real-world medical imaging tasks.
Q15: How do you evaluate the performance of a model in medical image analysis?
Evaluating the performance of a model in medical image analysis is crucial for understanding the effectiveness and reliability of the model in real-world clinical applications. The choice of evaluation metrics depends on the specific task, such as classification, segmentation, or registration. Here are some commonly used evaluation metrics for different medical image analysis tasks:
- Classification: In classification tasks, such as detecting the presence of a tumor or classifying a disease stage, the performance of a model is often evaluated using the following metrics:
- Accuracy: The proportion of correctly classified instances out of the total instances.
- Sensitivity (Recall): The proportion of true positive instances (e.g., correctly identified tumors) among the actual positive instances.
- Specificity: The proportion of true negative instances (e.g., correctly identified healthy tissue) among the actual negative instances.
- Precision: The proportion of true positive instances among the instances classified as positive.
- F1 Score: The harmonic mean of precision and recall, providing a balanced measure of both metrics.
- Area Under the Receiver Operating Characteristic (ROC) Curve (AUC-ROC): A plot of sensitivity versus 1-specificity, with the area under the curve representing the model’s ability to distinguish between positive and negative instances.
2. Segmentation: In segmentation tasks, such as delineating tumor boundaries or separating organs, the performance of a model is often evaluated using metrics that measure the overlap or similarity between the predicted segmentation and the ground truth (manually annotated) segmentation:
- Intersection over Union (IoU, also known as Jaccard Index): The ratio of the intersection of the predicted and ground truth regions to their union.
- Dice Coefficient (also known as Sørensen-Dice or F1 Score for segmentation): The ratio of twice the intersection of the predicted and ground truth regions to the sum of the areas of the predicted and ground truth regions.
- Hausdorff Distance: The maximum of the minimum distances between points on the predicted and ground truth boundaries, measuring the worst-case error in the boundary localization.
- Mean Surface Distance: The average of the minimum distances between points on the predicted and ground truth boundaries, providing a measure of the average error in the boundary localization.
3. Registration: In registration tasks, where the goal is to align multiple images (e.g., from different time points or modalities), the performance of a model is often evaluated using metrics that measure the similarity between the registered images or the accuracy of the alignment:
- Target Registration Error (TRE): The average distance between corresponding landmarks (e.g., anatomical points) in the registered images, providing a measure of the alignment accuracy.
- Mutual Information (MI): A measure of the statistical dependence between the intensities of the registered images, with higher MI indicating a better alignment.
- Normalized Cross-Correlation (NCC): A measure of the similarity between the registered images, with higher NCC indicating a better alignment.
In addition to these metrics, other factors should be considered when evaluating the performance of a model in medical image analysis, such as:
- Validation strategy: Using a proper validation strategy, such as k-fold cross-validation or a holdout validation set, is crucial to obtain a reliable estimate of the model’s performance on unseen data.
- Clinical relevance: The chosen evaluation metrics should be clinically relevant and aligned with the specific goals of the medical imaging task. For example, in some cases, it might be more important to prioritize sensitivity (detecting all true positive cases) over precision (reducing false positive cases).
- Interpretability: The model’s ability to provide interpretable and explainable results
Q16: Explain the difference between semantic segmentation and instance segmentation.
Semantic segmentation and instance segmentation are two related tasks in computer vision and image analysis, with the primary goal of partitioning an image into meaningful regions or segments. However, they differ in their objectives and granularity of the segmentation:
- Semantic Segmentation: In semantic segmentation, the goal is to assign a class label to each pixel in the image, such that pixels belonging to the same class (e.g., a specific object, structure, or background) share the same label. The output of semantic segmentation is a dense classification map where each pixel is assigned a class label. However, semantic segmentation does not differentiate between individual instances of the same class. For example, in a medical image with multiple tumors, semantic segmentation would label all tumor pixels with the same class label, without distinguishing between the different tumors.
- Instance Segmentation: Instance segmentation is a more fine-grained task that aims to not only assign a class label to each pixel but also separate individual instances of objects or structures within the same class. In other words, instance segmentation seeks to distinguish and label different occurrences of the same class separately. In the example of a medical image with multiple tumors, instance segmentation would not only label the tumor pixels but also differentiate between the individual tumors, assigning a unique instance label to each tumor.
The choice between semantic and instance segmentation depends on the specific goals and requirements of the image analysis task. Semantic segmentation is generally sufficient when the primary objective is to classify regions or structures in an image, whereas instance segmentation is needed when it is important to identify and analyze individual instances of objects or structures within the same class.
Various techniques can be applied to both semantic and instance segmentation tasks, with deep learning-based methods, particularly convolutional neural networks (CNNs) and their variants, demonstrating significant success in recent years. Some common deep learning architectures for semantic segmentation include Fully Convolutional Networks (FCNs), SegNet, and U-Net, while popular instance segmentation architectures include Mask R-CNN and YOLACT.
Q17: What is U-Net and how is it used in medical imaging?
U-Net is a convolutional neural network (CNN) architecture specifically designed for biomedical image segmentation tasks. It was first introduced by Ronneberger, Fischer, and Brox in their 2015 paper, “U-Net: Convolutional Networks for Biomedical Image Segmentation.” The U-Net architecture is well-suited for segmenting small datasets with limited annotated images, which is a common challenge in medical imaging.
The U-Net architecture has an encoder-decoder structure, resembling the shape of the letter “U,” which is the origin of its name. The key components of the U-Net architecture are:
- Contracting Path (Encoder): The contracting path consists of multiple convolutional and max-pooling layers that gradually downsample the input image, capturing the context and high-level features of the image. Each convolutional layer is typically followed by a rectified linear unit (ReLU) activation function, and the feature maps are downsampled using max-pooling layers.
- Expanding Path (Decoder): The expanding path consists of multiple up-convolution (also known as deconvolution or transposed convolution) and convolutional layers that gradually upsample the feature maps back to the original input image resolution. This path focuses on precise localization and capturing the fine-grained details of the structures in the image. The up-convolution layers are also followed by ReLU activation functions.
- Skip Connections: One of the key features of the U-Net architecture is the use of skip connections between the corresponding layers of the contracting and expanding paths. These connections pass the feature maps from the contracting path directly to the expanding path, allowing the network to retain high-resolution details and spatial information, which is crucial for accurate segmentation.
- Final Layer: The final layer of the U-Net is a convolutional layer with a softmax or sigmoid activation function that produces the segmentation map, assigning a class label to each pixel in the image.
In medical imaging, U-Net has been widely adopted for various segmentation tasks due to its ability to produce accurate and precise segmentations, even with limited training data. Examples of its applications in medical imaging include segmenting tumors, organs, blood vessels, and other structures in images from modalities such as MRI, CT, ultrasound, and histopathology. The U-Net architecture has also inspired several variations and improvements, such as the V-Net, TernausNet, and Attention U-Net, which have been designed to address specific challenges or incorporate additional features for medical image segmentation tasks.
Q18: Describe the process of image registration in medical imaging.
Image registration is a critical process in medical imaging that involves aligning and superimposing two or more images, often acquired from different imaging modalities (e.g., MRI, CT, PET), time points (e.g., pre- and post-treatment), or perspectives. The goal of image registration is to establish spatial correspondences between the images, enabling the analysis and integration of complementary information from the different images. Image registration is widely used in various medical applications, such as image-guided surgery, treatment planning, monitoring disease progression, and studying the structure and function of the human body.
The process of image registration generally consists of the following steps:
- Image acquisition: Obtain the images to be registered, which can come from different imaging modalities, time points, or perspectives. These images are often referred to as the “fixed” (or “reference”) image and the “moving” (or “source”) image. The goal is to align the moving image to the fixed image.
- Preprocessing: Perform preprocessing on the images to enhance their quality and facilitate the registration process. Common preprocessing steps include noise reduction, intensity normalization, resampling, and cropping.
- Feature extraction (optional): In some registration methods, particularly feature-based registration, it is necessary to identify and extract salient features or landmarks from the images, such as corners, edges, or anatomical structures. These features serve as the basis for establishing correspondences between the images.
- Transformation model: Choose an appropriate transformation model that defines how the moving image will be spatially transformed to align with the fixed image. Transformation models can be classified as:
- Rigid transformations: Preserve distances and angles (e.g., translation, rotation).
- Affine transformations: Preserve parallelism but not necessarily distances and angles (e.g., scaling, shearing).
- Non-rigid or deformable transformations: Allow for local deformations and warping (e.g., B-spline, thin-plate splines).
- Similarity metric: Choose a suitable similarity metric to quantify the degree of alignment between the fixed and moving images. The choice of similarity metric depends on the image modalities and the specific registration task. Common similarity metrics include:
- Sum of Squared Differences (SSD): Measures the squared intensity differences between the images.
- Normalized Cross-Correlation (NCC): Measures the correlation between the intensities of the images.
- Mutual Information (MI): Measures the statistical dependence between the intensities of the images.
- Optimization: Find the optimal transformation parameters that maximize (or minimize) the chosen similarity metric, effectively aligning the moving image with the fixed image. This optimization process can be performed using various optimization algorithms, such as gradient descent, conjugate gradient, or Powell’s method.
- Resampling and interpolation: Apply the optimal transformation to the moving image using resampling and interpolation techniques, such as nearest-neighbor, linear, or spline interpolation, to generate the registered image.
- Post-processing and evaluation: Perform post-processing steps, if necessary, such as smoothing or masking, and evaluate the quality of the registration using visual inspection, quantitative metrics (e.g., Target Registration Error), or expert validation.
Different registration methods, such as intensity-based, feature-based, or deformable registration, may emphasize or modify some of these steps depending on the specific requirements and challenges of the registration task. The choice of registration method, transformation model, similarity metric, and optimization algorithm should be carefully considered based on the nature of the images, the desired level of accuracy, and the computational resources available.
Q19: What is the role of Generative Adversarial Networks (GANs) in medical imaging?
Generative Adversarial Networks (GANs) are a class of deep learning models introduced by Ian Goodfellow and his colleagues in 2014. GANs consist of two neural networks, a generator and a discriminator, that are trained together in a game-theoretic adversarial process. The generator learns to create synthetic data samples, while the discriminator learns to distinguish between real and synthetic data samples. As the training progresses, the generator becomes better at generating realistic samples, and the discriminator becomes better at identifying them, resulting in a generator capable of producing high-quality synthetic data.
In medical imaging, GANs have found numerous applications, including but not limited to:
- Data Augmentation: Medical imaging datasets are often limited in size due to privacy concerns, the high cost of data acquisition, and the need for expert annotations. GANs can generate synthetic yet realistic medical images, which can be used to augment the training data, improving the performance and generalization of machine learning models.
- Image Synthesis: GANs can be used to synthesize medical images with specific attributes, such as simulating the appearance of a disease or the effect of a treatment. This can be useful for generating hypothetical scenarios, studying disease progression, or creating educational materials.
- Image-to-Image Translation: GANs can perform image-to-image translation tasks, such as converting images from one modality to another (e.g., MRI to CT), reconstructing high-resolution images from low-resolution inputs (super-resolution), or generating synthetic contrast-enhanced images from non-contrast images. These capabilities can be useful for improving image quality, reducing radiation exposure, or facilitating multimodal image analysis.
- Segmentation: GANs can be used for segmentation tasks, where the goal is to delineate specific structures or regions in medical images. In this context, GANs have been employed to generate more accurate and precise segmentations by incorporating adversarial training in the form of adversarial loss, which encourages the segmentation model to produce results that are indistinguishable from the ground truth segmentations.
- Anomaly Detection: GANs can be used to detect anomalies or abnormalities in medical images by learning the distribution of normal anatomy and identifying deviations from this distribution. This can be helpful for identifying tumors, lesions, or other pathological structures in medical images.
- De-identification: GANs can be used to generate synthetic medical images that preserve the relevant clinical information while removing personally identifiable information (PII) or other sensitive attributes. This can be useful for maintaining patient privacy and sharing medical images for research purposes without violating data protection regulations.
Several GAN architectures have been specifically designed or adapted for medical imaging applications, such as pix2pix, CycleGAN, 3D-GAN, and MedGAN. Despite their success and versatility, GANs also present challenges in medical imaging, such as mode collapse, training instability, and the need for careful evaluation of the generated images to ensure their clinical validity and usefulness.
Q20: Explain the concept of feature extraction in medical imaging.
Feature extraction is a critical step in medical image analysis that involves identifying and extracting meaningful and informative features or attributes from the images. These features serve as a compact and representative description of the image content, capturing relevant patterns, structures, or properties that can be used for various tasks, such as classification, segmentation, registration, or retrieval. Feature extraction helps reduce the dimensionality of the data, mitigates the effects of noise and variations, and enhances the efficiency and performance of machine learning models.
There are two main types of feature extraction techniques used in medical imaging:
- Handcrafted Features: These are traditional features that are manually designed and engineered by domain experts to capture specific image properties, such as intensity, texture, shape, or local structures. Examples of handcrafted features include:
- Intensity-based features: Mean, standard deviation, and histogram-based features that describe the distribution of pixel intensities.
- Texture-based features: Haralick features, Gabor filters, and Local Binary Patterns (LBP) that describe the spatial patterns and variations in pixel intensities.
- Shape-based features: Geometrical and topological properties of segmented structures, such as area, perimeter, compactness, and curvature.
- Edge-based features: Gradient magnitude, gradient direction, and edge maps derived from edge detection algorithms, such as Sobel, Canny, or Laplacian of Gaussian (LoG).
- Transform-based features: Features obtained from transformed image representations, such as Fourier Transform, Wavelet Transform, or Principal Component Analysis (PCA).
- Learned Features: With the advent of deep learning, feature extraction has shifted towards automatically learning the most relevant features directly from the data, without relying on expert knowledge or manual engineering. Convolutional Neural Networks (CNNs) are the most common deep learning models used for feature extraction in medical imaging. The hierarchical structure of CNNs allows them to learn increasingly complex and abstract features at different levels of the network, starting from low-level features, such as edges or textures, to high-level features, such as shapes or semantic structures.
In medical imaging, feature extraction plays a crucial role in various applications, such as detecting and diagnosing diseases, predicting treatment outcomes, or analyzing the structure and function of the human body. The choice of feature extraction technique depends on the specific problem, the nature of the images, the desired level of interpretability, and the computational resources available. While handcrafted features offer more interpretability and control over the extracted features, learned features can potentially capture more complex and abstract patterns that are not readily identifiable by human experts or traditional methods. In some cases, combining handcrafted and learned features can provide complementary information and improve the overall performance of the medical image analysis task.
Q21: How do you approach handling large datasets in medical imaging projects?
Handling large datasets in medical imaging projects can be challenging due to the high resolution of medical images, the diverse range of imaging modalities, and the need for efficient storage, processing, and analysis of the data. Here are some strategies for managing large datasets in medical imaging projects:
- Data Storage and Organization: Use efficient storage formats, such as HDF5, NIfTI, or DICOM, which are designed to store and organize large volumes of medical imaging data. Make sure to organize your data in a structured and consistent manner, using a standardized directory structure and file naming convention that facilitates easy access and retrieval of the data.
- Data Compression: Compress your data using lossless or lossy compression techniques to reduce storage space and accelerate data transfer. For instance, you can use gzip, bzip2, or specialized image compression algorithms like JPEG 2000. Keep in mind that lossy compression techniques can affect image quality, so choose an appropriate level of compression based on the specific requirements of your project.
- Data Preprocessing: Preprocess your data to reduce its dimensionality and complexity, while preserving the relevant information. Common preprocessing techniques include resizing, resampling, cropping, intensity normalization, and noise reduction. This can significantly reduce computational resources required for processing and analyzing the data.
- Batch Processing: When training machine learning models or performing data analysis, process the data in smaller batches rather than loading the entire dataset into memory. This can help prevent memory overflow issues and make the computations more efficient.
- Parallel and Distributed Computing: Utilize parallel and distributed computing techniques, such as multi-threading, multi-processing, or distributed computing frameworks (e.g., Apache Spark, Dask) to accelerate data processing and analysis tasks. This can help you take advantage of multiple CPU cores, GPUs, or clusters of machines to handle large datasets more efficiently.
- Hardware Acceleration: Use specialized hardware, such as GPUs or TPUs, to accelerate the training and inference of deep learning models, which can significantly reduce the computational time and resources needed to process large datasets.
- Data Augmentation: When working with large datasets, data augmentation techniques can be employed to increase the diversity of the training data without the need for additional data acquisition. Techniques like rotation, flipping, scaling, and elastic deformation can help improve the performance and generalization of machine learning models.
- Transfer Learning: Leverage pre-trained models and transfer learning techniques to reduce the amount of data and computational resources needed for training new models. By initializing your model with weights learned from a related task or domain, you can take advantage of the existing knowledge and fine-tune your model with a smaller subset of your large dataset.
- Active Learning: Use active learning techniques to iteratively select the most informative and representative samples from your large dataset for annotation and model training. This can help reduce the amount of data and resources needed for training, while still maintaining high performance.
- Model Selection and Evaluation: When dealing with large datasets, consider using efficient model selection and evaluation techniques, such as k-fold cross-validation or hold-out validation, to estimate the performance of your model and avoid overfitting.
By combining these strategies, you can effectively handle large datasets in medical imaging projects, ensuring efficient storage, processing, and analysis of the data while optimizing the performance of your machine learning models.
Q22: What are some ethical considerations in medical image analysis?
Ethical considerations in medical image analysis are essential to ensure that the development and deployment of these technologies are responsible, safe, and beneficial to patients and healthcare providers. Some key ethical concerns include:
- Data Privacy and Security: Medical images contain sensitive and personally identifiable information (PII) that must be protected to ensure patient privacy. Techniques such as data anonymization, de-identification, encryption, and access control should be implemented to prevent unauthorized access and data breaches. Compliance with data protection regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR), is also crucial.
- Informed Consent: Patients should be informed about the use of their medical images for research, development, or clinical purposes, and their consent should be obtained before their data is used. This includes explaining the purpose of the data collection, the potential risks and benefits, and any potential data sharing or commercialization.
- Bias and Fairness: Medical image analysis models should be trained and validated on diverse and representative datasets to minimize biases and ensure fairness in their performance across different patient populations, imaging modalities, and clinical settings. Unintended biases in the data or the model can lead to unequal treatment or misdiagnosis, disproportionately affecting certain groups of patients.
- Transparency and Explainability: Medical image analysis models should be transparent and interpretable, enabling healthcare providers to understand the rationale behind their predictions and decisions. This can help build trust, facilitate model validation, and enable human oversight in the clinical decision-making process. Techniques such as feature visualization, saliency maps, and model-agnostic explanation methods can be used to improve the explainability of complex models, such as deep learning networks.
- Accuracy and Validation: Medical image analysis models should be rigorously validated on independent datasets and in real-world clinical settings to ensure their accuracy, reliability, and generalizability. This includes using appropriate performance metrics, such as sensitivity, specificity, and area under the receiver operating characteristic (ROC) curve, as well as conducting clinical trials and comparative studies with existing diagnostic methods.
- Accountability and Responsibility: Clear lines of accountability and responsibility should be established for the development, deployment, and use of medical image analysis models, including addressing potential errors, adverse outcomes, or malfunctions. This includes establishing a robust system for monitoring, reporting, and addressing any issues that may arise in the clinical implementation of these technologies.
- Collaboration and Communication: Effective collaboration and communication between developers, researchers, healthcare providers, regulatory authorities, and patients are essential to ensure the responsible development and deployment of medical image analysis technologies. This includes sharing best practices, guidelines, and lessons learned, as well as engaging in interdisciplinary research, education, and public dialogue on the ethical, legal, and social implications of these technologies.
By addressing these ethical considerations, medical image analysis technologies can be developed and deployed in a manner that respects patient privacy, ensures fairness and accuracy, promotes transparency and accountability, and ultimately benefits patients and healthcare providers.
Q23: How do you ensure patient privacy when working with medical imaging data?
Ensuring patient privacy when working with medical imaging data is crucial to comply with data protection regulations and maintain trust with patients and healthcare providers. Here are some strategies to protect patient privacy in medical imaging projects:
- Data De-identification: Remove any personally identifiable information (PII) from the medical images and associated metadata. This includes patient names, identification numbers, birth dates, addresses, and any other information that could be used to identify an individual directly or indirectly.
- Data Anonymization: Replace or obfuscate sensitive information with pseudonyms, random identifiers, or other forms of synthetic data that cannot be linked back to the original patient. This process should be irreversible to prevent the re-identification of the patient from the anonymized data.
- Data Encryption: Encrypt medical images and associated data at rest and in transit using strong encryption algorithms, such as AES or RSA, to protect against unauthorized access, data breaches, and interception during data transfer.
- Access Control: Implement strict access control policies and authentication mechanisms to restrict access to medical imaging data to only authorized personnel. This may include role-based access control, multi-factor authentication, and regular audits of access logs to monitor for any unauthorized access or potential security breaches.
- Data Use Agreements: Establish data use agreements or data sharing agreements with collaborators, partners, or third-party service providers that outline the terms and conditions for data access, use, storage, and disposal. These agreements should emphasize the importance of patient privacy and require adherence to applicable data protection regulations and best practices.
- Secure Data Storage: Store medical imaging data on secure servers, using appropriate physical and logical security measures, such as firewalls, intrusion detection systems, and regular security updates and patches. Consider using secure cloud storage services that comply with data protection regulations and offer additional security features, such as encryption, access control, and data backup.
- Data Minimization: Only collect, store, and process the minimum amount of data necessary to achieve the specific goals of your medical imaging project. Limiting the amount of sensitive data you work with can help reduce the potential risks and consequences of a data breach or privacy violation.
- Informed Consent: Obtain informed consent from patients before using their medical imaging data for research, development, or clinical purposes. This includes providing clear and transparent information about the purpose of the data collection, the potential risks and benefits, and the measures taken to protect their privacy.
- Privacy-preserving Techniques: Explore privacy-preserving techniques, such as federated learning, differential privacy, or homomorphic encryption, which allow you to train machine learning models or perform data analysis without accessing the raw patient data directly. These techniques can help maintain patient privacy while still enabling the development and deployment of medical image analysis technologies.
- Compliance with Regulations: Ensure compliance with relevant data protection regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or the General Data Protection Regulation (GDPR) in the European Union. Familiarize yourself with the specific requirements of these regulations and implement the necessary safeguards and procedures to protect patient privacy.
By adopting these strategies, you can effectively protect patient privacy while working with medical imaging data, ensuring compliance with data protection regulations and maintaining trust with patients and healthcare providers.
Q24: What is the difference between 2D, 3D, and 4D medical imaging?
Medical imaging is used to capture visual representations of anatomical structures, physiological functions, and pathological conditions of the human body. The dimensionality of the image refers to the number of spatial dimensions that are represented in the image. Here is a brief explanation of the differences between 2D, 3D, and 4D medical imaging:
- 2D Medical Imaging: 2D medical imaging refers to images that have only two spatial dimensions, such as length and width. Common examples of 2D medical imaging include X-ray images, ultrasound images, and photographs of tissue samples. 2D images are flat and do not contain information about depth or volume.
- 3D Medical Imaging: 3D medical imaging refers to images that have three spatial dimensions, such as length, width, and depth. 3D medical images can be reconstructed from a series of 2D images acquired at different angles or depths, or they can be obtained directly from volumetric imaging modalities such as CT (computed tomography) or MRI (magnetic resonance imaging). 3D medical images provide a more detailed and accurate representation of anatomical structures and can be used for surgical planning, diagnosis, and research.
- 4D Medical Imaging: 4D medical imaging refers to images that have four dimensions, adding the dimension of time to the three-dimensional space. 4D medical imaging is used to capture the dynamic changes in physiological processes over time, such as cardiac function, respiratory motion, or blood flow. 4D medical imaging can be obtained from modalities such as 4D ultrasound, cardiac MRI, or dynamic CT scans. 4D imaging can provide important information about the functional status of organs and tissues and can be used for diagnosis, treatment planning, and monitoring of disease progression.
In summary, the difference between 2D, 3D, and 4D medical imaging lies in the number of spatial dimensions represented in the image. 2D images are flat and have only two spatial dimensions, 3D images have three spatial dimensions, and 4D images add the dimension of time to the three-dimensional space. Each type of imaging has its unique strengths and limitations, and the choice of imaging modality depends on the specific clinical application and the information needed for diagnosis, treatment, or research.
Q25: Explain the concept of multi-modal medical imaging and its benefits.
Multi-modal medical imaging involves combining data from different imaging modalities to create a more comprehensive and accurate representation of the human body. This approach can provide complementary information about the anatomical and functional characteristics of organs and tissues, improving diagnostic accuracy and treatment planning. Here are some benefits of multi-modal medical imaging:
- Improved Diagnostic Accuracy: Multi-modal imaging can provide a more comprehensive and accurate assessment of anatomical and functional abnormalities compared to single-modality imaging. By combining data from multiple modalities, such as CT, MRI, and PET (positron emission tomography), radiologists and clinicians can better visualize the location, size, shape, and metabolic activity of tumors or other pathological conditions. This can lead to more accurate diagnosis, staging, and treatment planning.
- Enhanced Functional Imaging: Different imaging modalities can provide unique information about the functional characteristics of organs and tissues. For example, functional MRI (fMRI) can be used to measure brain activity, while PET can be used to measure metabolic activity. By combining these modalities, researchers can obtain a more comprehensive picture of the functional changes associated with various diseases or treatments.
- Reduced False-Positive and False-Negative Results: Multi-modal imaging can help reduce the incidence of false-positive and false-negative results that can occur with single-modality imaging. For example, combining PET with CT or MRI can help distinguish between benign and malignant lesions that may be difficult to differentiate with single-modality imaging alone.
- Improved Treatment Planning: Multi-modal imaging can provide more precise information about the location and extent of tumors or other pathological conditions, allowing for more accurate treatment planning. For example, combining CT and MRI can provide detailed information about the tumor’s location and size, while PET can provide information about the metabolic activity of the tumor. This can help clinicians determine the appropriate treatment approach, such as surgery, radiation therapy, or chemotherapy.
- Reduced Radiation Exposure: Multi-modal imaging can also help reduce radiation exposure to patients by using lower doses of radiation for each imaging modality. For example, combining CT with PET or MRI can reduce the amount of radiation exposure compared to using CT alone.
In summary, multi-modal medical imaging involves combining data from different imaging modalities to provide a more comprehensive and accurate assessment of anatomical and functional abnormalities. This approach can improve diagnostic accuracy, enhance functional imaging, reduce false-positive and false-negative results, improve treatment planning, and reduce radiation exposure.
Q26: How do you handle overfitting in machine learning models for medical imaging?
Overfitting occurs when a machine learning model learns the training data too well, including noise and irrelevant features, resulting in poor performance on new, unseen data. Overfitting is a common problem in machine learning models for medical imaging, where the data may be complex, high-dimensional, and heterogeneous. Here are some strategies to prevent and mitigate overfitting in machine learning models for medical imaging:
- Regularization: Regularization techniques, such as L1 and L2 regularization, can be used to penalize the model’s complexity and prevent overfitting. These techniques add a regularization term to the loss function, which encourages the model to learn simpler and more generalizable patterns.
- Data Augmentation: Data augmentation techniques, such as random rotations, translations, and scaling, can be used to increase the size and diversity of the training dataset. This can help the model learn more robust and invariant features and reduce overfitting.
- Dropout: Dropout is a regularization technique that randomly drops out a fraction of the model’s neurons during training, preventing the model from relying too much on specific features or neurons. This can help the model learn more generalizable features and reduce overfitting.
- Early Stopping: Early stopping is a technique that stops the training process when the model’s performance on a validation dataset starts to degrade, preventing it from overfitting the training data. This can help determine the optimal number of epochs or training iterations that maximize the model’s performance without overfitting.
- Ensemble Methods: Ensemble methods, such as bagging and boosting, can be used to combine multiple models trained on different subsets of the training data or with different hyperparameters. This can help reduce the variance and bias of the individual models and improve the overall performance and robustness of the ensemble.
- Cross-Validation: Cross-validation is a technique that partitions the training data into multiple folds and trains the model on different combinations of the folds, validating its performance on the remaining fold. This can help estimate the model’s generalization error and prevent overfitting by reducing the risk of selecting a specific subset of the training data that fits the model too well.
- Hyperparameter Tuning: Hyperparameter tuning involves optimizing the model’s hyperparameters, such as learning rate, regularization strength, and network architecture, to find the best combination that maximizes the model’s performance on a validation dataset. This can help prevent overfitting by finding the optimal balance between model complexity and generalization.
By adopting these strategies, you can prevent and mitigate overfitting in machine learning models for medical imaging, improving their performance and generalizability on new, unseen data.
Q27: What is the role of reinforcement learning in medical imaging?
Reinforcement learning is a subfield of machine learning that focuses on teaching an agent to make decisions by interacting with an environment and receiving feedback in the form of rewards or penalties. In medical imaging, reinforcement learning can be used to develop intelligent systems that learn to analyze medical images and make decisions based on clinical outcomes. Here are some examples of the role of reinforcement learning in medical imaging:
- Automated Diagnosis: Reinforcement learning can be used to train models that automatically diagnose medical conditions based on medical imaging data. The agent can learn to recognize patterns and features in the images and use them to make accurate diagnoses based on the rewards or penalties received for each prediction.
- Automated Treatment Planning: Reinforcement learning can be used to develop models that automatically plan treatment strategies based on medical images and patient-specific information. The agent can learn to optimize the treatment plan by selecting the most effective and efficient options based on the rewards or penalties received for each decision.
- Image Segmentation: Reinforcement learning can be used to develop models that segment medical images into different anatomical structures or regions of interest. The agent can learn to identify the boundaries and characteristics of each structure based on the rewards or penalties received for each segmentation.
- Optimized Imaging Protocols: Reinforcement learning can be used to develop models that optimize imaging protocols for different clinical scenarios, such as reducing radiation exposure or contrast agent usage. The agent can learn to balance the trade-offs between image quality, patient safety, and efficiency based on the rewards or penalties received for each protocol.
- Active Learning: Reinforcement learning can be used to develop models that actively select the most informative images or regions of interest for annotation or analysis. The agent can learn to prioritize the most relevant and informative data based on the rewards or penalties received for each selection.
In summary, reinforcement learning can be used to develop intelligent systems that learn to analyze medical images and make decisions based on clinical outcomes. These systems can automate diagnosis, treatment planning, image segmentation, imaging protocol optimization, and active learning, improving the efficiency and accuracy of medical imaging analysis and decision-making.
Q28: Describe the concept of Radiomics and its significance in medical imaging.
Radiomics is a field of medical imaging that involves the extraction and analysis of quantitative features from medical images to help diagnose, classify, and predict disease outcomes. Radiomics uses advanced machine learning algorithms to identify and quantify imaging biomarkers, such as texture, shape, and intensity, that are associated with specific diseases or conditions. Here are some key concepts and significance of radiomics in medical imaging:
- Quantitative Imaging Biomarkers: Radiomics aims to extract quantitative imaging biomarkers that can provide more objective and accurate information about disease characteristics, prognosis, and response to treatment than traditional qualitative or subjective assessments. These biomarkers can be used to differentiate between benign and malignant lesions, predict disease progression, and assess treatment response.
- Non-Invasive and Reproducible: Radiomics is a non-invasive and reproducible method that uses existing medical images to extract relevant information about disease characteristics. This avoids the need for invasive procedures or additional imaging studies and reduces patient discomfort and radiation exposure. Moreover, the quantitative features extracted by radiomics are reproducible and can be validated across different imaging modalities and institutions.
- Personalized Medicine: Radiomics enables personalized medicine by providing individualized information about disease characteristics and treatment response based on the patient’s unique imaging data. This can help tailor treatment options and monitor disease progression in real-time, improving patient outcomes and quality of life.
- Integration with other -omics data: Radiomics can be integrated with other -omics data, such as genomics, proteomics, and metabolomics, to provide a comprehensive picture of disease characteristics and mechanisms. This can help identify new targets for drug development and precision medicine approaches.
- Challenges: Radiomics also presents several challenges, such as standardization of image acquisition and analysis protocols, feature selection and validation, and integration with clinical data. These challenges require collaborative efforts among radiologists, clinicians, and data scientists to develop robust and clinically relevant radiomics models.
In summary, radiomics is a field of medical imaging that aims to extract and analyze quantitative imaging biomarkers to help diagnose, classify, and predict disease outcomes. Radiomics offers non-invasive, reproducible, and personalized medicine approaches and can be integrated with other -omics data for a comprehensive understanding of disease mechanisms. While radiomics presents several challenges, its potential benefits for clinical decision-making and patient care are significant.
Q29: Explain the importance of data normalization in medical imaging projects.
Data normalization is an essential preprocessing step in medical imaging projects that involves scaling the input data to a common range or distribution. The purpose of data normalization is to remove variations in the data that are not related to the underlying biological or physiological processes and to improve the performance and interpretability of machine learning models. Here are some key reasons why data normalization is important in medical imaging projects:
- Consistent Scale: Medical imaging data can have different scales and ranges, depending on the imaging modality and acquisition parameters. Data normalization ensures that the input data is on a consistent scale and range, allowing machine learning models to compare and learn from the data more accurately.
- Avoids Bias: Normalizing the data removes the influence of any variations in the data that are not biologically or physiologically relevant, such as differences in pixel intensity between different scanners, imaging protocols, or patients. This can prevent bias in the model and improve its generalization performance on new, unseen data.
- Improves Convergence: Normalizing the data can help machine learning models converge faster and more stably during training by reducing the range of the input data and avoiding the saturation of activation functions. This can save computational resources and time and improve the reliability of the model.
- Facilitates Interpretability: Normalizing the data can help facilitate the interpretation of machine learning models by making the input data more meaningful and comparable across different modalities or datasets. This can help clinicians and researchers understand the underlying mechanisms and features associated with specific diseases or conditions and identify potential biomarkers.
- Avoids Overfitting: Normalizing the data can help prevent overfitting by reducing the influence of irrelevant or noisy features in the data that may be more prominent in some samples than others. This can improve the model’s generalization performance and reduce the risk of overestimating the model’s accuracy.
In summary, data normalization is an essential preprocessing step in medical imaging projects that helps remove variations in the data that are not related to the underlying biological or physiological processes and improves the performance and interpretability of machine learning models. Data normalization ensures a consistent scale, avoids bias, improves convergence, facilitates interpretability, and avoids overfitting.
Q30: What are some applications of deep learning in medical imaging?
Deep learning is a subset of machine learning that involves the use of deep neural networks with multiple layers to learn representations of data. In medical imaging, deep learning has shown great promise in improving the accuracy and efficiency of various tasks, including image classification, segmentation, registration, and analysis. Here are some examples of the applications of deep learning in medical imaging:
- Automated Diagnosis: Deep learning can be used to develop models that automatically diagnose medical conditions based on medical imaging data, such as CT scans, MRI scans, and X-rays. These models can learn to recognize patterns and features in the images that are associated with specific diseases or conditions and make accurate diagnoses.
- Image Segmentation: Deep learning can be used to develop models that segment medical images into different anatomical structures or regions of interest. These models can learn to identify the boundaries and characteristics of each structure and enable more accurate and efficient diagnosis and treatment planning.
- Medical Image Registration: Deep learning can be used to develop models that align and register multiple medical images of the same patient taken at different times or with different modalities. These models can learn to extract relevant features and match them across images, improving the accuracy and consistency of the registration process.
- Virtual Biopsy: Deep learning can be used to develop models that simulate a biopsy procedure by analyzing medical images and predicting the biopsy results. These models can learn to identify suspicious lesions and estimate the likelihood of malignancy, reducing the need for invasive procedures and improving patient outcomes.
- Drug Discovery: Deep learning can be used to develop models that analyze medical images and identify new drug targets and pathways for drug discovery. These models can learn to identify subtle changes in the images that are associated with specific diseases or conditions and suggest potential drug candidates.
- Radiomics: Deep learning can be used to develop models that extract and analyze quantitative features from medical images to help diagnose, classify, and predict disease outcomes. These models can learn to identify imaging biomarkers that are associated with specific diseases or conditions and improve the accuracy and objectivity of diagnosis and prognosis.
In summary, deep learning has shown great promise in improving the accuracy and efficiency of various tasks in medical imaging, including automated diagnosis, image segmentation, medical image registration, virtual biopsy, drug discovery, and radiomics. These applications can lead to more personalized and effective medical care and better patient outcomes.
Q31: How do you deal with noisy or low-quality medical images?
Medical images may often be of poor quality, which can be caused by several factors, such as the limitations of the imaging equipment, patient movement, and artifacts from image reconstruction. The presence of noise or other distortions in the images can adversely affect the performance of machine learning models used in medical image analysis. Here are some strategies for dealing with noisy or low-quality medical images:
- Image Preprocessing: Image preprocessing can help remove noise or other artifacts from medical images before being fed into machine learning models. Techniques such as image filtering, noise reduction, and artifact removal can be applied to improve image quality and consistency.
- Data Augmentation: Data augmentation techniques such as rotation, translation, and flipping can help increase the diversity and quality of the training dataset. This can help the machine learning models learn more robust and resilient features, making them less susceptible to noisy and low-quality images.
- Transfer Learning: Transfer learning involves using pre-trained models that have already learned useful features from large datasets to classify or segment new medical images. This approach can help reduce the impact of noisy or low-quality images by using the learned features to extract more robust and informative features from the images.
- Ensemble Learning: Ensemble learning involves combining the predictions of multiple machine learning models to obtain more accurate and robust results. This approach can help reduce the impact of noisy or low-quality images by averaging the predictions of multiple models that have learned different features and patterns in the data.
- Selective Sampling: Selective sampling involves selecting only high-quality images for training and testing the machine learning models. This approach can help reduce the impact of noisy or low-quality images by focusing on the most informative and representative samples.
- Expert Knowledge: Expert knowledge from radiologists or other medical professionals can be used to guide the machine learning models to focus on the most relevant features in the images. This can help reduce the impact of noise or other distortions by focusing on the most informative and clinically relevant features.
In summary, dealing with noisy or low-quality medical images requires a combination of image preprocessing techniques, data augmentation, transfer learning, ensemble learning, selective sampling, and expert knowledge. These strategies can help improve the performance and reliability of machine learning models used in medical image analysis, despite the presence of noisy or low-quality images.
Q32: Describe some common performance metrics used in medical imaging tasks.
Performance metrics are essential to evaluate the accuracy and effectiveness of machine learning models used in medical imaging tasks. These metrics provide quantitative measures of the model’s performance and help compare different models and techniques. Here are some common performance metrics used in medical imaging tasks:
- Accuracy: Accuracy is a measure of the proportion of correctly classified or segmented images out of the total number of images in the dataset. Accuracy can be a useful metric when the classes or regions of interest are well balanced in the dataset.
- Sensitivity and Specificity: Sensitivity and specificity are measures of the model’s ability to correctly identify positive and negative cases, respectively. Sensitivity is the proportion of true positive cases (i.e., correctly identified cases) out of all positive cases, while specificity is the proportion of true negative cases (i.e., correctly identified non-cases) out of all negative cases. Sensitivity and specificity are particularly useful in medical imaging tasks where the cost of false negatives or false positives is high.
- Precision and Recall: Precision and recall are measures of the model’s ability to correctly identify positive cases and avoid false positives, respectively. Precision is the proportion of true positive cases out of all cases identified as positive by the model, while recall is the proportion of true positive cases out of all actual positive cases. Precision and recall are useful in medical imaging tasks where the goal is to avoid unnecessary treatments or procedures while accurately identifying cases.
- F1 Score: The F1 score is a harmonic mean of precision and recall and is used as a single metric to evaluate the model’s overall performance. The F1 score is particularly useful in medical imaging tasks where there is an imbalance between the number of positive and negative cases.
- Dice Similarity Coefficient (DSC): The DSC is a measure of the similarity between two sets of segmented regions of interest. The DSC is calculated as twice the intersection of the two sets divided by their sum. The DSC is commonly used in medical imaging tasks to evaluate the overlap or agreement between manual and automated segmentations.
- Receiver Operating Characteristic (ROC) Curve: The ROC curve is a graphical representation of the model’s performance across different threshold values. The ROC curve plots the true positive rate (sensitivity) against the false positive rate (1-specificity) for different threshold values, and the area under the curve (AUC) is used as a metric of the overall performance. The ROC curve and AUC are useful in medical imaging tasks where the cost of false negatives and false positives varies.
In summary, accuracy, sensitivity and specificity, precision and recall, F1 score, DSC, and ROC curve are common performance metrics used in medical imaging tasks. These metrics provide quantitative measures of the model’s performance and help compare different models and techniques. The choice of the appropriate metric depends on the specific task and the balance between the cost of false negatives and false positives.
Q33: The rest of the answer is here.
Natural language processing (NLP) is a field of artificial intelligence that deals with the processing and analysis of human language. In medical imaging, NLP can be used to extract and analyze text-based clinical data, such as medical reports, electronic health records (EHRs), and other clinical notes. NLP can help improve the accuracy, efficiency, and interpretability of medical imaging tasks by enabling the integration of text-based information with image-based information. Here are some examples of the role of NLP in medical imaging:
- Radiology Report Analysis: Radiology reports contain a wealth of information about the patient’s condition, including the type of imaging study, the findings, and the impression. NLP can be used to extract relevant information from radiology reports and integrate it with image-based data to improve the accuracy and efficiency of diagnosis and treatment planning.
- Clinical Decision Support: NLP can be used to analyze EHRs and other clinical notes to provide clinical decision support for medical imaging tasks. NLP can help identify relevant patient information, such as medical history, medications, and allergies, and provide personalized recommendations for imaging studies and interpretation.
- Image Annotation: NLP can be used to annotate medical images with relevant clinical information, such as anatomical structures, findings, and diagnoses. This can help improve the interpretability and utility of medical images for clinicians and researchers.
- Automated Report Generation: NLP can be used to generate automated reports from medical images and other clinical data. This can help improve the efficiency and consistency of reporting and reduce the burden on radiologists and other healthcare professionals.
- Quality Assurance: NLP can be used to analyze radiology reports and other clinical notes to identify quality issues, such as missed findings, incorrect interpretations, and discrepancies between reports. This can help improve the accuracy and reliability of medical imaging tasks and reduce the risk of adverse events.
In summary, NLP has a significant role in medical imaging by enabling the integration of text-based clinical data with image-based data to improve the accuracy, efficiency, and interpretability of medical imaging tasks. NLP can be used for radiology report analysis, clinical decision support, image annotation, automated report generation, and quality assurance. NLP is a promising area of research that can help advance the field of medical imaging and improve patient outcomes.
Q34: Explain the concept of computer-aided diagnosis (CAD) in medical imaging.
Computer-aided diagnosis (CAD) is a technique that uses machine learning algorithms and other computational methods to assist radiologists and other healthcare professionals in the diagnosis and interpretation of medical images. CAD systems analyze medical images and provide quantitative and qualitative information to support the decision-making process. Here are some key features of CAD in medical imaging:
- Automated Image Analysis: CAD systems use machine learning algorithms to analyze medical images and identify abnormal features or structures. These algorithms can be trained on large datasets of medical images and learn to recognize patterns and features that are associated with specific diseases or conditions.
- Decision Support: CAD systems provide decision support to radiologists and other healthcare professionals by highlighting regions of interest and providing quantitative and qualitative measurements of the abnormal features or structures. This can help improve the accuracy and efficiency of diagnosis and treatment planning.
- Integration with Clinical Data: CAD systems can integrate with clinical data, such as medical histories, laboratory results, and other diagnostic tests, to provide a more comprehensive assessment of the patient’s condition. This can help improve the specificity and sensitivity of diagnosis and reduce the risk of false positives and false negatives.
- Personalized Medicine: CAD systems can help support personalized medicine by providing patient-specific information that can guide treatment decisions. For example, CAD systems can help identify biomarkers that are associated with specific diseases or conditions and suggest targeted therapies based on the patient’s individual characteristics.
- Quality Assurance: CAD systems can provide quality assurance by reviewing radiology reports and identifying discrepancies or missed findings. This can help improve the accuracy and consistency of medical imaging interpretation and reduce the risk of adverse events.
CAD systems have been used in a wide range of medical imaging applications, including mammography, lung cancer screening, cardiovascular imaging, and neuroimaging. CAD systems have shown great promise in improving the accuracy and efficiency of medical imaging interpretation and enabling more personalized and effective medical care.
In summary, CAD is a technique that uses machine learning algorithms and other computational methods to assist radiologists and other healthcare professionals in the diagnosis and interpretation of medical images. CAD systems provide automated image analysis, decision support, integration with clinical data, personalized medicine, and quality assurance. CAD is a promising area of research that can help improve the accuracy and efficiency of medical imaging interpretation and enable more personalized and effective medical care.
Q35: Describe the difference between image classification, object detection, and image segmentation.
Image classification, object detection, and image segmentation are three fundamental tasks in computer vision, including medical imaging. Here are the main differences between these three tasks:
- Image Classification: Image classification is the task of assigning a label or class to an entire image based on its content. In medical imaging, image classification can be used to identify the presence or absence of a specific disease or condition based on the entire image. Image classification algorithms usually take an input image and produce a single output label or class.
- Object Detection: Object detection is the task of identifying and localizing one or more objects of interest within an image. In medical imaging, object detection can be used to identify specific anatomical structures or lesions within an image. Object detection algorithms usually take an input image and produce a set of bounding boxes around the detected objects, along with the corresponding class labels.
- Image Segmentation: Image segmentation is the task of partitioning an image into multiple regions or segments based on its content. In medical imaging, image segmentation can be used to identify and isolate specific anatomical structures or lesions within an image. Image segmentation algorithms usually take an input image and produce a pixel-wise label map, where each pixel is assigned to a specific segment or class.
In summary, image classification, object detection, and image segmentation are three fundamental tasks in computer vision, including medical imaging. Image classification is the task of assigning a label or class to an entire image, object detection is the task of identifying and localizing one or more objects of interest within an image, and image segmentation is the task of partitioning an image into multiple regions or segments based on its content. These tasks have different goals, and the choice of the appropriate task depends on the specific application and the level of detail required.
Q36: How do you handle false positives and false negatives in medical image analysis?
False positives and false negatives are common challenges in medical image analysis. False positives occur when the algorithm detects a lesion or abnormality that is not present, while false negatives occur when the algorithm misses a lesion or abnormality that is present. Here are some strategies to handle false positives and false negatives in medical image analysis:
- Improve Data Quality: One of the main causes of false positives and false negatives is poor image quality, such as noise, artifacts, or motion blur. Improving the quality of the imaging acquisition can help reduce the incidence of false positives and false negatives. This can be achieved by optimizing the imaging protocol, improving the equipment, or implementing motion correction techniques.
- Optimize Algorithm Parameters: The performance of machine learning algorithms in medical image analysis is highly dependent on the choice of algorithm parameters. Optimizing the parameters of the algorithm, such as the learning rate, regularization, or thresholding, can help reduce the incidence of false positives and false negatives. This can be achieved by using grid search or other optimization techniques.
- Incorporate Clinical Information: Incorporating clinical information, such as medical history, laboratory results, or other diagnostic tests, can help reduce the incidence of false positives and false negatives. This can help provide a more comprehensive assessment of the patient’s condition and reduce the risk of misdiagnosis.
- Ensemble Methods: Ensemble methods involve combining multiple machine learning algorithms to improve performance and reduce the incidence of false positives and false negatives. This can be achieved by using bagging, boosting, or other ensemble techniques.
- Iterative Refinement: Iterative refinement involves iteratively improving the performance of the algorithm by incorporating feedback from the clinician or radiologist. This can help identify false positives and false negatives and refine the algorithm’s performance over time.
In summary, false positives and false negatives are common challenges in medical image analysis. Strategies to handle false positives and false negatives include improving data quality, optimizing algorithm parameters, incorporating clinical information, using ensemble methods, and iterative refinement. These strategies can help improve the accuracy and reliability of medical image analysis and reduce the risk of misdiagnosis.
Q37: What is the significance of multi-task learning in medical imaging?
Multi-task learning is a machine learning technique that enables the joint learning of multiple related tasks using a single model. In medical imaging, multi-task learning has gained increasing attention due to its ability to improve the accuracy and efficiency of medical image analysis. Here are some of the significant benefits of multi-task learning in medical imaging:
- Improved Generalization: Multi-task learning can improve the generalization of machine learning models by allowing them to learn shared representations across multiple tasks. This can help reduce the risk of overfitting and improve the performance of the model on new, unseen data.
- Data Efficiency: Multi-task learning can improve data efficiency by enabling the transfer of knowledge between related tasks. This can be particularly useful in medical imaging, where datasets are often small and expensive to obtain. By jointly learning multiple tasks, multi-task learning can help improve the efficiency of data utilization and reduce the need for large amounts of labeled data.
- Robustness to Variability: Multi-task learning can improve the robustness of machine learning models to variability in the data, such as differences in imaging protocols, modalities, or patient populations. By jointly learning multiple tasks, multi-task learning can help the model learn features that are relevant across multiple domains and reduce the sensitivity to variability in the data.
- Clinical Relevance: Multi-task learning can improve the clinical relevance of machine learning models by enabling the joint learning of multiple clinically relevant tasks. For example, in medical imaging, multi-task learning can be used to jointly learn the detection and segmentation of a lesion, which are both clinically relevant tasks.
- Interpretability: Multi-task learning can improve the interpretability of machine learning models by enabling the identification of shared and task-specific features. This can help improve the transparency and trustworthiness of machine learning models in medical imaging and facilitate their adoption in clinical practice.
In summary, multi-task learning is a powerful technique in medical imaging that enables the joint learning of multiple related tasks using a single model. Multi-task learning can improve the generalization, data efficiency, robustness, clinical relevance, and interpretability of machine learning models in medical imaging. Multi-task learning is a promising area of research that can help advance the field of medical imaging and improve patient outcomes.
Q38: Explain the role of recurrent neural networks (RNNs) in medical imaging.
Recurrent neural networks (RNNs) are a class of neural networks that can process sequential data by maintaining a memory of previous inputs. In medical imaging, RNNs have been used in a variety of applications, including image and video analysis, time series prediction, and natural language processing. Here are some of the roles of RNNs in medical imaging:
- Temporal Data Analysis: RNNs are particularly useful for analyzing temporal data, such as time series data or videos. In medical imaging, RNNs can be used to analyze medical images acquired over time, such as dynamic contrast-enhanced MRI or cardiac MRI. RNNs can capture the temporal dynamics of the images and enable the identification of changes or abnormalities over time.
- Sequence Labeling: RNNs can be used for sequence labeling tasks, such as image captioning or medical report generation. In medical imaging, RNNs can be used to generate reports based on medical images, such as identifying the location, size, and characteristics of a lesion.
- Data Augmentation: RNNs can be used for data augmentation by generating new sequences based on existing ones. In medical imaging, RNNs can be used to generate synthetic medical images that are similar to real ones, which can help increase the size of the dataset and improve the performance of machine learning algorithms.
- Feature Extraction: RNNs can be used for feature extraction by learning representations of sequential data. In medical imaging, RNNs can be used to extract features from medical images and enable the classification or segmentation of the images based on their content.
- Disease Progression Modeling: RNNs can be used to model disease progression over time, such as the progression of Alzheimer’s disease or cancer. In medical imaging, RNNs can be used to model the progression of a disease based on medical images acquired at different time points and predict the future development of the disease.
In summary, RNNs are a powerful class of neural networks that can process sequential data and enable the analysis of temporal dynamics in medical imaging. RNNs can be used for a variety of tasks, including temporal data analysis, sequence labeling, data augmentation, feature extraction, and disease progression modeling. RNNs are a promising area of research that can help advance the field of medical imaging and improve patient outcomes.
Q39: Describe the importance of collaboration between data scientists and medical professionals in medical imaging projects.
Collaboration between data scientists and medical professionals is critical in medical imaging projects. Medical imaging is a complex and interdisciplinary field that requires expertise in both medicine and data science. Here are some of the reasons why collaboration between data scientists and medical professionals is essential in medical imaging projects:
- Clinical Relevance: Medical professionals have in-depth knowledge of medical imaging modalities, protocols, and clinical workflows. They can provide insights into the clinical relevance of the imaging data and help ensure that the analysis is clinically relevant.
- Data Interpretation: Medical professionals are experts in interpreting medical images and can provide valuable feedback on the accuracy and reliability of the analysis. They can help identify false positives and false negatives, ensure that the analysis is consistent with clinical practice, and provide guidance on the interpretation of the results.
- Data Labeling: Medical professionals can provide expert labeling of the imaging data, which is critical for the training and validation of machine learning algorithms. They can ensure that the labeling is accurate, consistent, and clinically relevant.
- Domain Expertise: Medical professionals bring domain expertise to medical imaging projects that data scientists may not have. They can provide valuable insights into the anatomy, physiology, and pathology of the human body and help identify relevant imaging features and biomarkers.
- Ethical Considerations: Medical professionals are well-versed in the ethical considerations of medical research and can help ensure that the project adheres to ethical standards, such as patient privacy and informed consent.
In summary, collaboration between data scientists and medical professionals is essential in medical imaging projects. Medical professionals bring clinical relevance, data interpretation, data labeling, domain expertise, and ethical considerations to medical imaging projects, while data scientists bring expertise in data science and machine learning. Collaboration between these two groups can help ensure that medical imaging projects are clinically relevant, accurate, and ethically sound and can help advance the field of medical imaging for the benefit of patients.
Q40: What are some recent advances and trends in medical image analysis?
Medical image analysis is a rapidly evolving field with many recent advances and emerging trends. Here are some of the recent advances and trends in medical image analysis:
- Deep Learning: Deep learning has revolutionized medical image analysis by enabling the development of highly accurate and efficient machine learning algorithms. Convolutional neural networks (CNNs) and recurrent neural networks (RNNs) are commonly used in medical image analysis, and new architectures are continuously being developed.
- Multi-Modal Imaging: Multi-modal imaging involves the integration of data from multiple imaging modalities, such as MRI, CT, PET, and ultrasound. Multi-modal imaging can provide complementary information and improve the accuracy and reliability of medical image analysis.
- Multi-Task Learning: Multi-task learning involves the joint learning of multiple related tasks using a single model. Multi-task learning can improve the generalization, data efficiency, and robustness of machine learning models in medical image analysis.
- Transfer Learning: Transfer learning involves the transfer of knowledge from one task to another. Transfer learning can improve the efficiency and accuracy of machine learning models in medical image analysis, particularly in cases where labeled data is scarce.
- Data Augmentation: Data augmentation involves the generation of synthetic data based on existing data. Data augmentation can help increase the size of the dataset and improve the performance of machine learning algorithms in medical image analysis.
- Explainable AI: Explainable AI involves the development of machine learning models that are transparent and interpretable. Explainable AI can help improve the trustworthiness and acceptance of machine learning models in medical imaging and facilitate their adoption in clinical practice.
- Federated Learning: Federated learning involves the training of machine learning models on distributed data sources, such as multiple hospitals or clinics. Federated learning can help improve the privacy and security of medical imaging data and enable the development of machine learning models that are robust to variability in the data.
In summary, medical image analysis is a rapidly evolving field with many recent advances and emerging trends. Deep learning, multi-modal imaging, multi-task learning, transfer learning, data augmentation, explainable AI, and federated learning are some of the recent advances and trends in medical image analysis that are helping to improve the accuracy, efficiency, and reliability of medical imaging for the benefit of patients.
In summary, medical image analysis is a rapidly evolving field with many recent advances and emerging trends. Deep learning, multi-modal imaging, multi-task learning, transfer learning, data augmentation, explainable AI, and federated learning are some of the recent advances and trends in medical image analysis that are helping to improve the accuracy, efficiency, and reliability of medical imaging for the benefit of patients.
🚀 Introducing MONAIGPT
— your new go-to #AI-powered documentation assistant for #MONAI Core! 🎯 Get quick answers, detailed explanations, and on-demand code snippets. Test the demo now and revolutionize your MONAI experience! #MedicalImaging #GPT3 🌐
Try a demo here.