Understanding What MRI Resolution Really Means
Resolution in Magnetic Resonance Imaging (MRI) is much more than just a number. It's a complex idea, vital for accurate medical diagnoses. Resolution determines the clarity and level of detail within the images, directly impacting a medical professional’s ability to identify subtle health issues. Understanding MRI resolution is, therefore, fundamental for anyone working with this powerful diagnostic tool.
Breaking Down the Components of Resolution
MRI resolution has three key components: spatial resolution, temporal resolution, and contrast resolution. Each contributes to the overall image quality and diagnostic capabilities.
-
Spatial Resolution: This is the ability to distinguish between two objects positioned close together. Think of the pixels in a digital camera. Higher spatial resolution means smaller pixels and a sharper, more detailed image. This allows medical professionals to visualize fine structures, such as tiny blood vessels or minute tissue changes.
-
Temporal Resolution: This refers to the ability to capture changes happening over time. It’s particularly important for dynamic processes like cardiac imaging or functional MRI (fMRI) studies of brain activity. High temporal resolution captures quick changes, giving a precise representation of these dynamic processes.
-
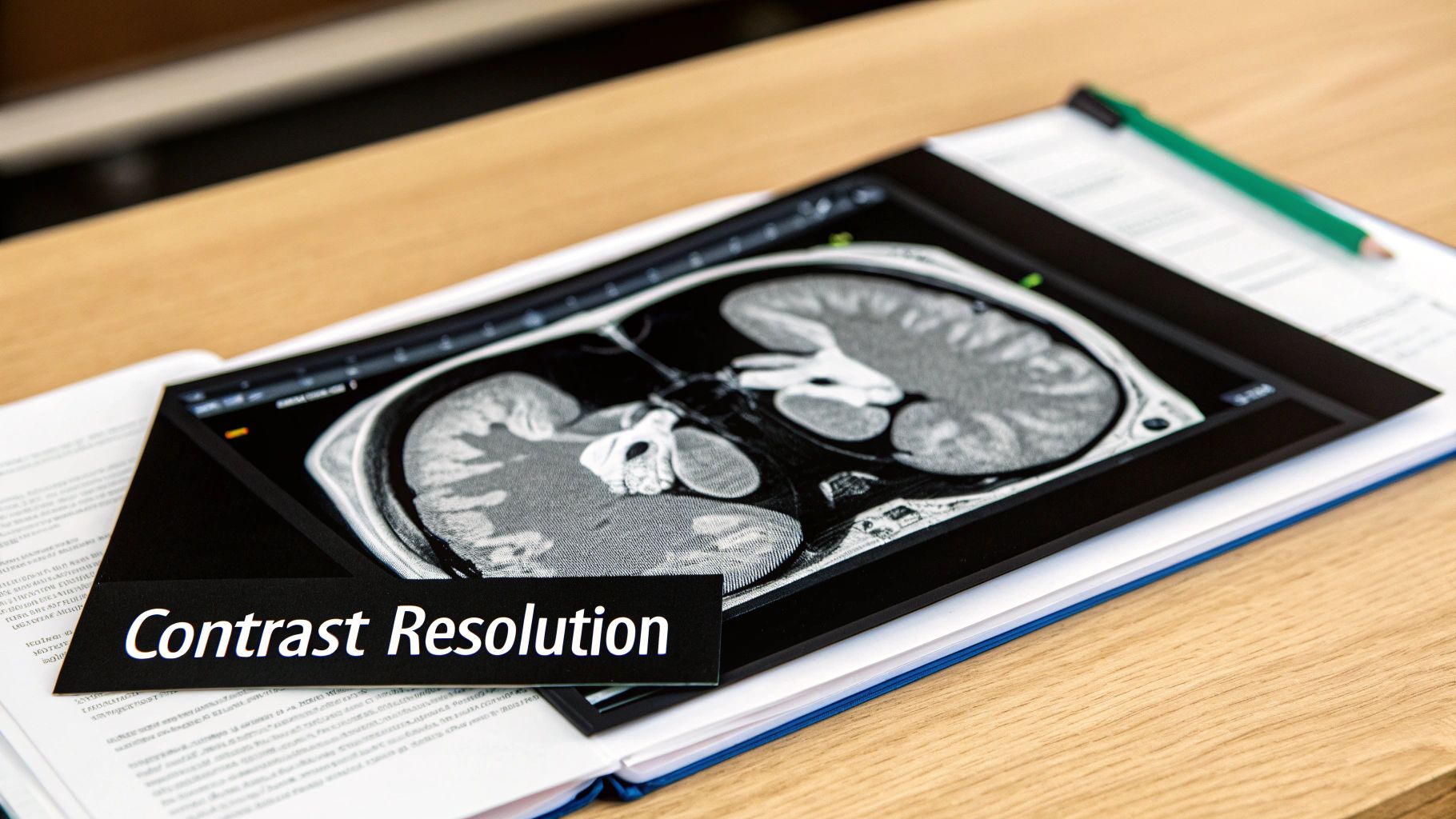
Contrast Resolution: This is the ability to differentiate between tissues based on their magnetic properties. Healthy tissue will have a different appearance than diseased tissue on an MRI scan because of differences in their composition. High contrast resolution highlights these differences, which is a significant aid in diagnosis.
These three components work together to create a diagnostically useful image. High spatial resolution, for instance, is essential for pinpointing small anatomical details, while high contrast resolution helps distinguish those details from the surrounding tissue. Temporal resolution is crucial for observing changes in organ function or blood flow.
The Impact of Tesla Ratings on Resolution
The magnetic field strength, measured in Tesla (T), plays a key role in MRI resolution. Higher Tesla ratings usually mean an improved signal-to-noise ratio, which can lead to better spatial and contrast resolution. This translates to clearer images and diagnoses doctors can be more confident in.
The Evolution of MRI Technology and Resolution
The development of MRI technology has greatly impacted the achievable resolution. 1.5T systems were once the standard. However, advancements in magnet technology saw the widespread adoption of 3T systems in the early 2000s. These 3T systems provided enhanced spatial resolution and faster imaging speeds, allowing for better visualization of small structures and thus improving diagnostic accuracy. Today, ultra-high-field MRI systems, such as 7T and beyond, are being explored for their potential to push resolution even further, primarily in research settings due to the technical hurdles involved. Explore this topic further here.
Practical Considerations for Resolution
While higher resolution is generally preferred, there are practical limitations to consider. Higher Tesla systems are often more costly to acquire and maintain. Some patients might also experience discomfort due to the stronger magnetic fields. Scan times can also be longer for high-resolution images. A balanced approach, therefore, is needed. The preferred resolution needs to be weighed against practical limitations, technology costs, and patient comfort. Understanding these factors is essential for making well-informed decisions about MRI protocols and getting the best image quality for a range of clinical needs.
How Tesla Ratings Transform Your Image Quality
The strength of the magnetic field, measured in Tesla (T), directly impacts the resolution of MRI scans. This isn't just a technical detail; it fundamentally alters the level of detail visible, impacting diagnostic confidence and patient outcomes. Let's explore how different Tesla ratings affect image quality in real-world clinical situations.
1.5T vs. 3T: A Clear Difference
The most frequently encountered field strengths in clinical settings are 1.5T and 3T. A 3T MRI system boasts a magnetic field twice the strength of a 1.5T system. This increased field strength results in a significantly enhanced signal-to-noise ratio (SNR). Imagine tuning into a radio station: a stronger signal (3T) delivers clearer "music" (image data) with less "static" (noise). This improved SNR substantially affects resolution.
For example, a 3T MRI can distinguish smaller structures and subtle tissue variations that a 1.5T MRI might overlook. This is particularly vital in neuroimaging, where pinpointing small lesions or anomalies is crucial for accurate diagnoses. The higher SNR of 3T can also facilitate shorter scan times, improving both patient comfort and operational efficiency.
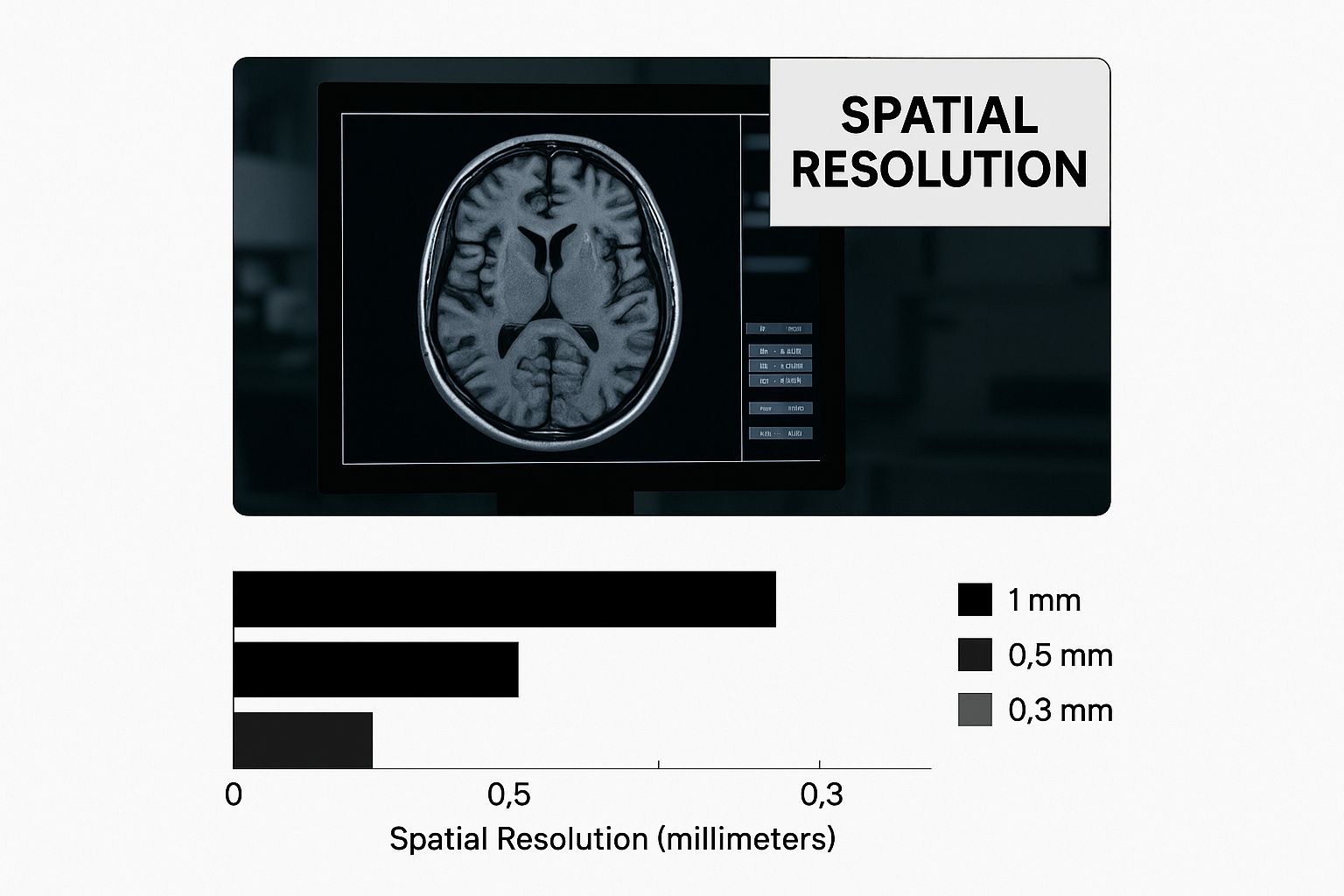
The infographic above depicts the spatial resolution of a brain scan displayed on a monitor. It illustrates the impressive increase in detail achieved with higher Tesla systems, providing clearer visualizations of complex brain structures. This enhanced visual clarity aids in detecting and characterizing even the smallest abnormalities.
Beyond 3T: Exploring Ultra-High Field Systems
While 3T remains the mainstay in many radiology departments, ultra-high-field systems like 7T are pushing the boundaries of MRI resolution. These systems offer even greater SNR, visualizing incredibly fine details. However, certain trade-offs must be considered.
- Increased Cost: Ultra-high-field MRI systems are significantly more expensive to acquire and maintain.
- Patient Comfort: Stronger magnetic fields can heighten patient anxiety and potentially cause peripheral nerve stimulation.
- Technical Complexity: Operating and maintaining these systems demands specialized expertise.
The decision to invest in ultra-high-field MRI depends on the specific clinical needs of the institution and the nature of the studies conducted.
To further illustrate the differences between MRI field strengths, let's look at the following comparison:
MRI Field Strength Comparison: Resolution and Performance
Detailed comparison of different Tesla ratings and their impact on resolution, scan time, and diagnostic capabilities
| Field Strength | Spatial Resolution | Scan Time | Best Applications | Limitations |
|---|---|---|---|---|
| 1.5T | Good | Moderate | General imaging, musculoskeletal, abdominal | Limited resolution for fine detail |
| 3T | Excellent | Moderate to Fast | Neuroimaging, cardiac, prostate, breast | Higher cost, potential for artifacts |
| 7T | Very High | Longer | Research, brain imaging, spectroscopy | Limited availability, patient comfort issues |
This table highlights the key differences between the common field strengths. While 1.5T remains a valuable tool for general imaging, 3T excels in specialized areas requiring high resolution. 7T, with its superior resolution, primarily serves research purposes and highly specialized applications.
Practical Implications and Hidden Costs
The advantages of improved resolution must be weighed against practical constraints and potential disadvantages. Higher Tesla systems aren't universally ideal. Some patients with implanted metallic devices are unsuitable for stronger magnetic fields. Scan times, while sometimes faster at 3T for certain applications compared to 1.5T, can lengthen with higher-resolution protocols. Moreover, the enhanced SNR at 3T can introduce susceptibility artifacts. These factors can substantially influence operational expenses and patient throughput.
These considerations require careful evaluation when determining the appropriate field strength for a specific clinical need. The optimal MRI resolution is a balance between image quality, patient-specific factors, and overall operational effectiveness.
Technical Parameters That Actually Matter
Beyond the glossy brochures and marketing hype, several crucial technical parameters significantly influence the resolution of Magnetic Resonance Imaging (MRI) and, consequently, its diagnostic capabilities. These factors extend beyond the commonly touted Tesla rating and are vital for radiologic technologists and clinicians to grasp. This section breaks down the critical parameters that can truly make a difference in patient outcomes, revealing how even subtle adjustments can dramatically enhance image quality without significantly impacting scan time or patient comfort.
Pulse Sequences: Tailoring the Scan
Pulse sequences are fundamental to MRI. They are precisely choreographed series of radiofrequency pulses and magnetic field gradients that dictate how signals are generated and acquired. Different pulse sequences highlight different tissue properties, and understanding these nuances is essential for optimizing MRI resolution.
For instance, spin echo (SE) sequences are renowned for their excellent contrast resolution, making them ideal for differentiating subtle variations between tissues. However, they can be time-consuming compared to other sequences.
Alternatively, gradient echo (GE) sequences provide faster scan times but may be more prone to artifacts. This makes them useful for dynamic imaging but potentially less suitable for high-resolution anatomical studies.
Matrix Size: The Pixel Grid
The matrix size in MRI is comparable to the pixel grid in a digital camera. A larger matrix (e.g., 512×512) means more data points are collected, leading to higher spatial resolution. This allows for the visualization of finer details and smaller structures.
However, a larger matrix also increases scan time, requiring a careful balance between resolution and practicality. A smaller matrix (e.g., 256×256) might suffice for routine examinations where the highest resolution isn’t critical.
Slice Thickness: Navigating the Depth Dimension
Slice thickness refers to the width of each image slice acquired in the scanning plane. Thinner slices provide enhanced resolution in the z-direction (depth), improving the ability to identify small lesions or subtle anatomical differences.
However, similar to matrix size, thinner slices can increase scan time. Thicker slices might be appropriate for some examinations but can potentially obscure finer details.
Field of View (FOV): Framing the Target
The field of view (FOV) defines the area captured within the image. A smaller FOV, focused tightly on the target area, offers higher resolution for that specific region. However, a FOV that’s too small can miss important surrounding structures.
A larger FOV captures a broader area but might compromise resolution. Therefore, optimizing the FOV necessitates carefully balancing the diagnostic objectives and anatomical context. Proper FOV selection can also significantly reduce image artifacts.
Studies indicate that optimizing technical parameters like matrix size and slice thickness can enhance diagnostic accuracy by up to 34% without extending scan time. Proper field of view selection has been shown to reduce image artifacts by an average of 67% across various anatomical regions. Explore this topic further here.
Interpreting Specifications and Making Informed Decisions
Understanding these technical parameters empowers radiologic technologists and clinicians to make well-informed decisions about MRI protocols, optimizing image quality while maintaining workflow efficiency. By tailoring these settings to the specific diagnostic needs of each patient, medical professionals can improve diagnostic confidence and ultimately contribute to better patient care.
Advanced Methods Pushing Resolution Boundaries
Magnetic field strength plays a vital role in the resolution of Magnetic Resonance Imaging (MRI). However, advancements in imaging techniques continually push the boundaries of what's achievable. These advanced methods offer ways to improve spatial, temporal, and contrast resolution without simply increasing Tesla ratings. This opens doors for more precise diagnoses and better patient care.
Parallel Imaging: Accelerating Acquisition Speed
Parallel imaging techniques, such as SENSE (SENSitivity Encoding) and GRAPPA (Generalized Autocalibrating Partially Parallel Acquisitions), utilize the unique spatial sensitivities of multiple receiver coils inside the MRI scanner. These techniques increase acquisition speed by acquiring less data than traditional methods. The full image is then reconstructed using the coil sensitivity information. This allows for higher resolution images in shorter scan times, increasing patient comfort and reducing motion artifacts.
Compressed Sensing: Exploiting Data Sparsity
Building on parallel imaging, compressed sensing further accelerates acquisition speed. This method is based on the principle that medical images are often sparse in certain domains (e.g., wavelet domain). This means a smaller number of coefficients can represent the essential information in the image. By acquiring a subset of data and using sophisticated algorithms, compressed sensing reconstructs high-resolution images from undersampled data, significantly reducing scan times without major image quality loss.
Emerging methods to boost resolution often involve newer equipment. Advanced Technologies can offer insights into the technological progress driving improvements in various fields, including medical imaging.
AI-Enhanced Reconstruction: Refining Image Quality
Artificial intelligence (AI) is rapidly changing medical imaging, including MRI. AI-enhanced reconstruction techniques use deep learning algorithms trained on large amounts of MRI data. This refines image quality and improves resolution. These algorithms identify and correct artifacts, enhance details, and even generate images from undersampled data. Healthcare facilities using AI-enhanced MRI reconstruction report 45% faster scan times and 28% better spatial resolution. Compressed sensing methods reduce motion artifacts by up to 73% in pediatric and claustrophobic patients. Learn more about advanced MRI techniques here.
Implementation and Clinical Impact
These advanced methods significantly improve MRI resolution but come with implementation challenges. Parallel imaging requires specialized hardware and software. Compressed sensing and AI-enhanced reconstruction need sophisticated algorithms and substantial computing power. However, the benefits for patient care are considerable. Higher resolution scans allow for more accurate diagnoses, leading to better treatment planning and improved patient outcomes.
Evaluating and Investing in New Technologies
When considering investing in these technologies, it's crucial to evaluate their potential benefits and practical limitations. Factors to consider include the institution's clinical needs, available technical expertise, and implementation and maintenance costs. The continuous advancement of these techniques promises to further revolutionize medical imaging, unlocking more diagnostic capabilities and expanding possibilities for patient care.
Matching Resolution Needs To Clinical Reality
Not every MRI requires the highest resolution. Understanding when prioritizing resolution is crucial, significantly impacting diagnostic accuracy and patient outcomes. This can mean the difference between early detection of a subtle pathology and missing it entirely. This section offers practical guidance on resolution requirements across various medical specialties, demonstrating how appropriate MRI resolution contributes to effective clinical practice.
Resolution Requirements Across Medical Specialties
Different medical specialties have varying resolution needs. For example, neurological microsurgery planning demands ultra-high precision, allowing surgeons to visualize intricate structures with exceptional clarity. Routine musculoskeletal imaging, however, may not require this level of detail, allowing for a more balanced approach. This balance ensures efficient resource use without compromising diagnostic quality.
To illustrate these varying needs, the following table summarizes typical resolution requirements for different medical specialties. It highlights the critical role of resolution selection in diagnostic imaging.
To help understand the varying resolution needs across different medical fields, let's take a look at the following table. This provides a comprehensive overview of resolution standards needed for different medical applications and anatomical regions.
| Medical Specialty | Typical Resolution | Key Structures | Critical Considerations | Scan Duration |
|---|---|---|---|---|
| Neurology | High (Sub-millimeter) | Brain tissue, cranial nerves, small vessels | Detection of small lesions, precise anatomical localization | Longer |
| Musculoskeletal | Moderate | Bones, joints, cartilage, ligaments, tendons | Visualization of tears, fractures, inflammation | Moderate |
| Oncology | Moderate to High | Tumor margins, lymph nodes, surrounding tissue | Accurate staging, treatment planning | Moderate to Longer |
| Cardiovascular | High (with Temporal Resolution) | Heart chambers, valves, blood flow | Assessment of cardiac function, detection of blockages | Moderate |
| Abdominal | Moderate | Organs, vessels, soft tissues | Identification of masses, infections, abnormalities | Moderate |
As this table demonstrates, the required resolution is highly dependent on the specific clinical application. Choosing the right resolution is key for balancing diagnostic accuracy with practical considerations like scan time.
Case Studies: Resolution’s Impact on Patient Outcomes
Real clinical scenarios demonstrate how MRI resolution directly influences patient outcomes. In one case, a high-resolution MRI revealed a small brain lesion missed on a lower-resolution scan. This early detection allowed for timely intervention, significantly improving the patient’s prognosis. In another case, using a higher resolution protocol for a routine musculoskeletal exam unnecessarily increased scan time and patient discomfort without providing any additional diagnostic information.
These examples underscore the importance of carefully considering resolution requirements based on the specific clinical context. The right protocol balances image quality with practical factors like scan time and patient comfort.
Balancing Quality and Efficiency
Successful radiology departments excel at balancing image quality with operational efficiency. This includes patient throughput, resource constraints, and overall workflow efficiency. Strategies for achieving this balance include:
- Developing standardized protocols for various examinations based on established diagnostic criteria
- Educating technologists on optimizing scan parameters for the desired resolution without excessive scan times
- Utilizing advanced imaging techniques like parallel imaging and AI-enhanced reconstruction to improve resolution and efficiency
- Regularly reviewing and updating protocols based on the latest clinical evidence and technological advancements
Patient Preparation and Equipment Maintenance
Patient preparation and equipment maintenance are vital for maximizing resolution. Patient motion significantly degrades image quality. Effective patient communication and immobilization techniques are essential to minimize motion artifacts. Regular equipment calibration and preventative maintenance ensure optimal performance and preserve resolution capabilities.
By implementing these strategies, radiology departments can maintain high image quality while maximizing patient comfort and operational efficiency. This balanced approach ensures the effective use of MRI technology for accurate diagnoses and improved patient care.
Your Practical Resolution Optimization Roadmap
Maximizing the resolution of MRI scans is an ongoing challenge in radiology. Acquiring the newest high-Tesla machine isn't the only solution. This roadmap offers practical strategies you can implement now to improve image quality without significantly impacting your budget or workflow.
Patient Preparation: The First Line of Defense
Patient movement is a primary source of image degradation. Even small movements can introduce motion artifacts, blurring critical details and affecting diagnostic accuracy. Patient preparation is the essential first step in resolution optimization.
-
Clear Communication: Explain the procedure clearly, highlighting the importance of staying still. Addressing patient concerns can significantly decrease involuntary movements during the scan.
-
Immobilization Techniques: Use cushions, straps, and headrests to comfortably stabilize patients. For especially difficult cases, consider breath-hold techniques or, with proper medical supervision, sedation.
-
Mock Scans: For anxious patients or those who struggle to stay still, a short “mock scan” can acclimate them to the environment and reduce anxiety, encouraging stillness during the actual procedure.
Equipment Optimization: Maintaining Peak Performance
Even the most sophisticated MRI system will generate subpar images if not properly maintained. Consistent equipment optimization is critical for preserving resolution.
-
Calibration and Quality Assurance: Implement a strong quality assurance program that includes regular calibration and phantom scans. This helps detect and rectify any deviations from optimal performance.
-
Preventative Maintenance: Follow the manufacturer's recommended maintenance schedule to prevent performance decline and ensure the longevity of your equipment. This includes checking coil integrity, gradient linearity, and other key components.
-
Software Updates: Maintain your MRI software with the latest updates. Software improvements often include algorithms that improve image reconstruction and artifact correction, improving resolution without hardware changes.
Protocol Refinement: Fine-Tuning for Success
Adjusting your MRI protocols is a budget-friendly way to achieve substantial resolution gains.
-
Pulse Sequence Selection: Each pulse sequence has advantages and disadvantages regarding resolution and scan time. For instance, spin echo (SE) sequences offer excellent contrast resolution, while gradient echo (GE) sequences provide faster scan times. Selecting the appropriate sequence is vital for balancing image quality with efficiency.
-
Matrix Size Optimization: A larger matrix size yields higher spatial resolution but also increases scan time. Experiment to find the best balance between matrix size and scan time for your clinical needs.
-
Slice Thickness Adjustment: Thinner slices improve resolution along the z-axis but also add to scan time. As with matrix size, optimizing slice thickness means balancing resolution needs with time constraints.
Advanced Techniques: Pushing the Limits
Incorporating advanced imaging techniques can drastically enhance resolution.
-
Parallel Imaging: Techniques like SENSE and GRAPPA increase acquisition speed, allowing for higher resolution images in shorter scan times. This is especially helpful for patients who have difficulty remaining still.
-
Compressed Sensing: This technique reconstructs high-resolution images from less data, further reducing scan times without compromising image quality.
-
AI-Enhanced Reconstruction: Deep learning algorithms are increasingly being implemented to refine image quality, enhance detail, and correct artifacts, boosting resolution without requiring longer scans.
To complement your optimization roadmap with growth strategies, you may find the information on Stripe Referral Programs helpful. The Stripe Referral Program Guide offers useful insights into revenue growth.
A Holistic Approach to Resolution
Optimizing MRI resolution requires a comprehensive strategy encompassing patient preparation, equipment maintenance, and protocol refinement. By implementing these strategies, you can notably improve image quality, enhance diagnostic confidence, and ultimately improve patient care. Explore the potential of AI-driven medical imaging solutions with PYCAD at https://pycad.co to further elevate your MRI capabilities.






