EHR interoperability is all about getting different healthcare IT systems to talk to each other—to exchange, understand, and actually use patient data without a hitch. It’s about weaving scattered pieces of information into a single, coherent patient story, giving caregivers the full picture right when it matters most.
The Vision of a Truly Connected Patient Journey
Imagine your entire medical history moving with you, instantly and securely available to any doctor, specialist, or hospital that needs it. That’s the real promise of interoperability—a future where critical health data flows as freely and reliably as compassion itself.
To really get a feel for its impact, let's look at two very different patient experiences.
First, the reality for many today. A patient with a chronic illness moves to a new town. Their medical records are stuck in different systems—one at their old family doctor's office, another at a specialist's clinic, and a third at the local hospital. The new care team has to chase down these records manually, a process that can drag on for weeks. Important details, like a past allergic reaction, might be lost in a blurry, faxed PDF, opening the door to dangerous mistakes. The patient ends up repeating expensive tests because their previous lab results and scans are locked away in another system. It’s a journey filled with friction, risk, and frustration.
From Fragmentation to Fluidity
Now, let's picture that same scenario, but this time powered by true interoperability. The patient walks into their new doctor's office. With a few secure clicks, the physician pulls up a complete, lifelong health record. It’s all there: past diagnoses, medication lists, high-resolution medical images, and even genetic test results.
This kind of immediate access changes everything:
- Safer Care: The system automatically flags a potential drug interaction based on the patient's complete medication history, preventing a serious adverse event.
- Smarter Decisions: The doctor instantly reviews a CT scan from six months ago, saving the patient from the cost and radiation of an unnecessary new test.
- Empowered Patients: Through a secure portal, the patient can see their own unified record, turning them into an active, informed participant in their own health.
- Better Coordination: Specialists, primary care providers, and ER doctors are all on the same page, working from a single source of truth to build a cohesive care plan.
This shift isn't just about technology; it's a fundamental change in philosophy. It’s about designing a system that puts the patient’s journey first, breaking down the walls between institutions to make healthcare safer, smarter, and more personal.
Think of it like modern banking. Years ago, you could only get cash from your specific bank branch. Today, you can use almost any ATM in the world. That’s exactly where we need to get with health information—making it securely available wherever and whenever care happens.
Platforms like the Google Healthcare API are crucial for building the infrastructure needed for this connected future. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms. This ensures that even the most complex visual data, like MRIs and CT scans, is part of this seamless exchange. You can see how we bring this to life in our portfolio.
Decoding the Language of Modern Health Data
For different health systems to truly collaborate, they need to speak the same digital language. Genuine interoperability of electronic health records relies on a set of universal translators—technical standards that give data a consistent structure and meaning, no matter where it comes from or where it's headed.
Without these standards, we're stuck in a digital Tower of Babel. Vital information gets lost in translation, and patient care suffers. Think of these standards as the grammar and vocabulary of health data. They’re the rules of the road that allow a lab system in one city to communicate flawlessly with an EHR in another. Getting to know these core languages is the first step toward building a truly connected healthcare ecosystem.
The Foundational Standards of Health Data
Three powerhouse standards form the backbone of health data exchange today, each built for a specific job. Understanding their unique roles is crucial to seeing how a patient's complete story—from clinical notes to complex imaging—gets pieced together.
- HL7 (Health Level Seven): This is the original workhorse, one of the most widely adopted standards for exchanging clinical and administrative data. Think of it as the formal, established language for sending structured messages like patient admissions, discharge summaries, and lab orders between different hospital departments.
- FHIR (Fast Healthcare Interoperability Resources): As the modern successor to older HL7 versions, FHIR is the new, agile language of health data. It functions a lot like the APIs that power your favorite mobile apps, using modern web technology to let systems quickly ask for and receive specific pieces of information—like a single allergy or a recent lab result.
- DICOM (Digital Imaging and Communications in Medicine): This is the undisputed global standard for all medical imaging. It's the "JPEG of medicine," making sure a CT scan, MRI, or X-ray keeps its diagnostic quality and patient data intact as it moves between scanners, storage systems, and viewing stations.
To really see the difference these standards make, let's compare the three main players.
Comparing Core Healthcare Interoperability Standards
This table breaks down the primary functions, typical use cases, and key advantages of the three foundational standards governing health data exchange.
| Standard | Primary Function | Common Use Case | Key Advantage |
|---|---|---|---|
| HL7 | Exchanges structured clinical and administrative messages between systems. | Sending patient admission/discharge info, lab orders, and results. | Mature, widely adopted, and deeply embedded in legacy hospital systems. |
| FHIR | Enables granular, real-time data access through modern web APIs. | Powering patient-facing mobile apps, pulling specific data into a clinical workflow. | Flexible, developer-friendly, and built on modern web standards (RESTful APIs). |
| DICOM | Manages the transmission, storage, and display of medical images. | Sharing a CT scan from a radiology department with a surgeon's workstation. | The universal standard for imaging, preserving diagnostic quality and metadata. |
Each standard plays a vital part, from the foundational messaging of HL7 to the specific, powerful language of DICOM. Together, they create the framework for a more connected and intelligent healthcare system.
The infographic below really brings this to life, showing the patient journey with and without this kind of seamless connection.
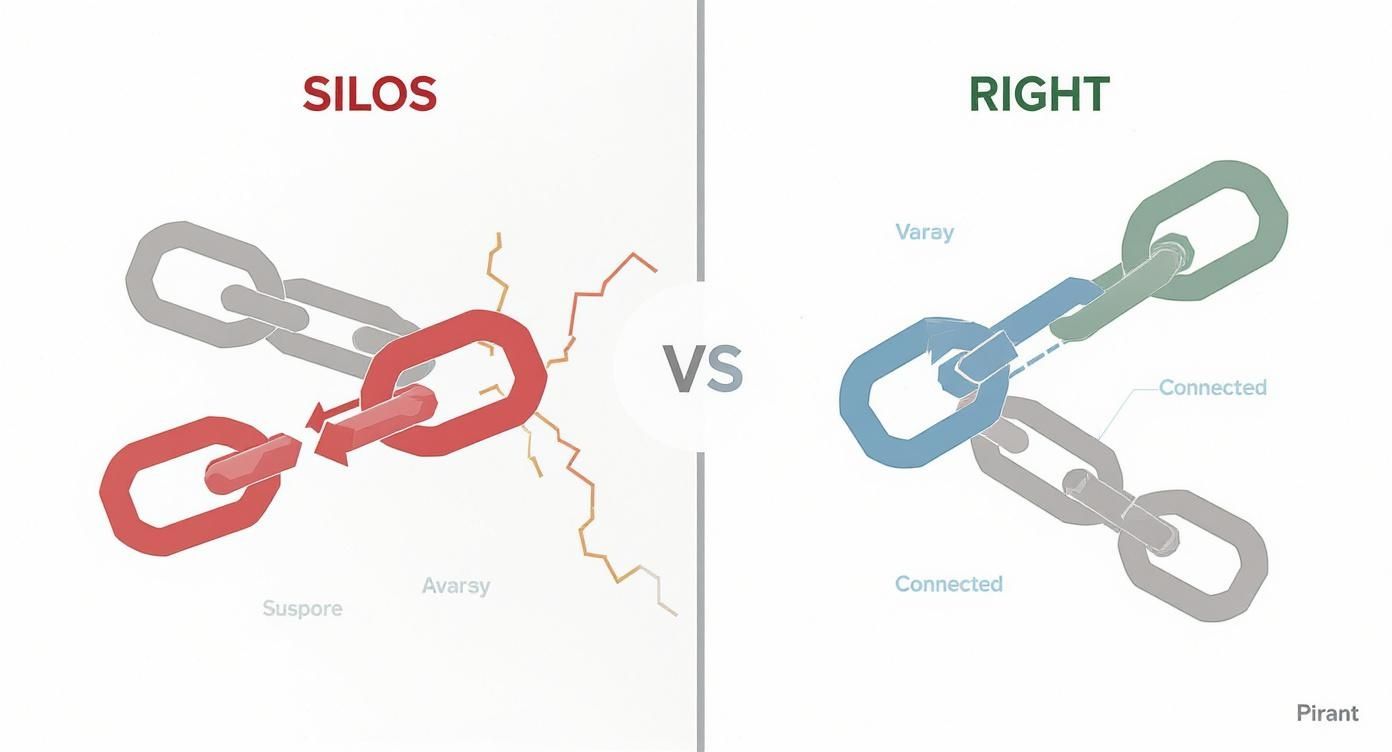
It’s a powerful contrast, isn't it? One side is fragmented and confusing, while the other is connected and fluid. That’s what interoperability does—it transforms patient care from a broken chain into a cohesive journey.
The Rise of FHIR as a Universal Connector
While all three standards are essential, FHIR has quickly become the star of the show. Its modern, API-first approach makes it incredibly easy for developers to create apps that securely pull data from different EHRs. This has unleashed a new wave of innovation, from patient-facing health apps to smart clinical decision support tools that were once just a dream.
The momentum behind FHIR is undeniable. It represents a collective shift toward open, accessible, and more granular data exchange, empowering both providers and patients with the right information at the right time.
The global healthcare community has certainly taken notice. By 2025, the adoption of FHIR APIs is set to become a global standard, with over 90% of EHR vendors worldwide supporting it as their baseline for data exchange. This movement is being pushed forward by regulations like the 21st Century Cures Act, which champion the need for open, patient-accessible data.
Making Complex Imaging Data Accessible
Even with a flexible standard like FHIR, medical imaging poses a unique problem. DICOM files are massive and complex, and they often require specialized software. This is where seamless integration becomes absolutely critical.
At PYCAD, we live and breathe this challenge. We specialize in building custom web DICOM viewers and integrating them into medical imaging web platforms. Our work ensures this vital visual data isn't locked away in isolated PACS systems. Instead, it becomes easily accessible to clinicians right within their primary workflow.
By creating intuitive, web-based viewers, we make sophisticated imaging data as interoperable as any other piece of the electronic health record. To get a deeper understanding of how these different systems connect, you might be interested in our article on data interoperability in healthcare. This is how we build a truly comprehensive patient view, where every piece of data—from a simple blood pressure reading to a detailed MRI—speaks the same language.
Overcoming the Barriers to Seamless Data Exchange

The vision of a truly connected patient journey is inspiring, but making it a reality isn't as simple as flipping a switch. Achieving true interoperability of electronic health records is a journey filled with real-world obstacles that demand tremendous effort, investment, and collaboration. These aren't just minor speed bumps; they're deep-rooted challenges that have slowed progress for years.
The first step toward dismantling these barriers is to understand them. We're not just talking about technical glitches. We're facing a complex mix of issues that touch on technology, finance, and even organizational culture. By looking these challenges straight in the eye, we can build practical, effective solutions that create lasting change.
Navigating Technical and Security Hurdles
At the core of the interoperability puzzle is a tangled web of technical complexities. Many healthcare organizations are still running on legacy systems—older software and hardware built long before seamless data sharing was even a goal. These systems often act like isolated islands, using proprietary data formats that make talking to modern platforms incredibly difficult and expensive.
Even with newer systems, the process of data mapping is a huge hurdle. Imagine trying to translate a novel between two languages where some words have no direct equivalent. That's what it’s like mapping information from one EHR's structure to another. Every single data point, from a lab result to a clinical note, must be precisely translated to preserve its meaning. It’s a painstaking process that's both slow and ripe for error.
Of course, with every connection comes a security risk. Understanding and implementing essential API security best practices is absolutely critical for safeguarding sensitive health information. Each link between systems creates a potential vulnerability, demanding rock-solid cybersecurity to protect patient privacy and maintain trust.
The Human and Financial Equation
Beyond the code and the servers, some of the biggest roadblocks are human and financial. Rolling out new interoperable systems requires a massive cultural shift within a healthcare organization. Staff need to be trained on entirely new ways of working, and old routines have to be completely rethought. This kind of change often meets resistance.
The price tag is just as intimidating. Upgrading or replacing old EHRs, buying integration engines, and dedicating IT staff to manage it all represents a major financial commitment. For smaller clinics or hospitals in rural areas, these costs can be a non-starter, creating a digital divide where only the biggest, best-funded institutions can afford to build a connected health ecosystem.
The journey to interoperability is a marathon, not a sprint. It demands persistent investment, a commitment to open standards, and a shared understanding that the ultimate goal—safer, more effective patient care—is worth the effort.
Despite all the progress we've made, full EHR interoperability is still a work in progress. Globally, only about 30% of providers have managed to achieve seamless data exchange across different systems. This disconnect is estimated to cost the U.S. healthcare system alone a staggering $30 billion every year from inefficiencies and repeated tests. Improving the interoperability of electronic health records isn't just a technical goal; it's a financial and clinical imperative.
At PYCAD, we're dedicated to solving a critical piece of this puzzle. We build custom web DICOM viewers and integrate them into medical imaging web platforms, making sure that complex visual data is never stuck in a silo. To see how we make this happen, check out our portfolio page.
Putting a Connected Health Ecosystem into Action
Knowing the barriers to interoperability is one thing; breaking them down is another. It takes a clear, actionable blueprint for change. Building a truly connected health ecosystem is a massive undertaking, but it’s absolutely possible with deliberate strategies designed to dismantle data silos piece by piece. The whole journey starts with a commitment to a few core principles and eventually scales up to advanced integrations that will fundamentally change how we deliver patient care.
This isn't just theory. It's about making conscious choices to adopt open standards, nurture collaboration, and place the free flow of patient data at the center of every tech decision. When we move from isolated systems to a unified network, we finally start to see what electronic health records were meant to be.
Start with Foundational Integration Tactics
The first real step is building a solid foundation with proven, effective tactics that make data sharing the default. Think of these as the essential building blocks for any organization that's serious about achieving the interoperability of electronic health records.
-
Embrace Standardized APIs: Modern healthcare depends on APIs, and FHIR (Fast Healthcare Interoperability Resources) has become the gold standard. When you prioritize EHRs and other systems that use FHIR, you’re ensuring that your data is structured for simple, secure, and precise exchange from the get-go.
-
Join a Health Information Exchange (HIE): An HIE is like a digital town square where different providers in a region can securely share patient information. Actively participating in one breaks down the walls between hospitals and clinics, giving a doctor a much more complete picture of a patient’s journey.
-
Implement a Master Patient Index (MPI): One of the most common—and dangerous—data errors is a simple case of mistaken identity. An MPI protocol establishes a single source of truth for patient identities across all your systems, finally making sure that "John Smith" in one department is correctly linked to "Jonathan Smith" in another.
These foundational steps lay the technical and organizational groundwork for the more advanced integrations to come. They help shift the entire mindset from "my data" to "our shared patient data."
Solving the Complex Puzzle of Medical Imaging
Nowhere are data silos more frustrating than in medical imaging. DICOM files are massive and complex, often trapping critical diagnostic information inside isolated Picture Archiving and Communication Systems (PACS). Making this visual data truly interoperable is a tough, specialized job—but a vital one.
This is a challenge we at PYCAD live and breathe. We build custom web DICOM viewers and integrate them into medical imaging web platforms, so radiologists, surgeons, and specialists can view and collaborate on images from anywhere, right inside their existing workflow.
True interoperability means every piece of the patient puzzle is accessible. When we make medical images as fluid as lab results, we complete the clinical picture and empower providers to make better, faster decisions.
To get this right, you need to explore a range of strategies and strong platforms, including specialized healthcare services that can build and integrate these critical systems. At PYCAD, our intense focus on imaging interoperability tackles a major pain point in modern healthcare.
You can see concrete examples of how we bring this vision to life on our portfolio page. These strategies aren't just about connecting software; they're about connecting care teams to create a safer, more efficient, and more human healthcare experience for everyone.
The Real-World Impact of Interoperable Records

We can talk about technical standards and integration strategies all day, but what does success actually look like out in the wild? The true measure of the interoperability of electronic health records isn't found in lines of code. It’s found in those quiet moments where a life is saved, a diagnosis is made faster, and a patient finally feels truly understood.
These are the stories that remind us why this isn’t just an IT project—it's about fundamentally changing how we deliver compassionate, effective care. When data flows freely and intelligently, the impact is immediate, personal, and profound.
From Potential Danger to Proactive Prevention
Picture this: a tourist on vacation suffers a sudden medical emergency. They're rushed to a local ER, unconscious and unable to share their medical history. In a disconnected system, this is a dangerous guessing game for the medical team. But with interoperable records, the ER physician can securely pull up that patient's home record in seconds.
The system immediately flags a life-threatening allergy to a common drug the doctor was just about to order. A tragedy is avoided, not by luck, but by design. This is the power of connected data in action—it’s a silent, digital guardian angel for every patient, no matter where they are.
This same principle is a game-changer for managing chronic conditions. Think about a patient with diabetes who sees a primary care doctor, an endocrinologist, and a podiatrist, all in different health systems.
Interoperability ensures that a blood sugar reading taken at one clinic is instantly visible to the others. It creates a collaborative shield, allowing the entire care team to work from a single, up-to-the-minute picture of the patient’s health.
This connected view helps them coordinate care, adjust treatments in near real-time, and catch the small problems before they become serious complications.
A Case Study in Coordinated Excellence
Beyond individual wins, the impact scales to entire communities. One regional health network was battling long wait times and fragmented care. They made a bold move to unify their systems across ten hospitals and dozens of outpatient clinics.
The results were stunning. By giving every provider access to a shared patient record, they saw incredible changes:
- Dramatically reduced wait times: ER doctors could instantly see a patient's history, cutting out the agonizing wait for faxed records from another facility.
- A sharp decline in redundant testing: Radiologists could easily access prior MRIs and CT scans, saving the system money and sparing patients unnecessary radiation.
- Higher care quality: Patient satisfaction scores soared as people felt their care was more coordinated and personal.
This network proved that the interoperability of electronic health records is a direct line to better, safer, and more efficient healthcare for an entire population.
For us at PYCAD, this is our core mission. We build custom web DICOM viewers and integrate them into medical imaging web platforms, turning isolated scans into shareable, actionable insights for clinicians.
These real-world examples are powerful proof that when we connect our systems, we connect our care. To see how our custom solutions bring this vision to life, feel free to explore our projects on our portfolio page.
Your Questions on EHR Interoperability Answered
The world of connected healthcare is full of complex ideas and technical acronyms. As we all strive for better interoperability of electronic health records, it's completely normal to have questions pop up along the way. This last section is all about giving you clear, straightforward answers to some of the most common ones.
Think of this as a final conversation to tie everything together. We'll demystify a few key concepts and offer some practical insights, leaving you with the confidence to champion a more integrated, intelligent future for healthcare.
What Is the Difference Between Interoperability and Integration?
It’s a great question, because these two words get thrown around a lot, sometimes even interchangeably. But they represent two very different ideas, and the distinction gets right to the heart of what we’re trying to achieve with patient data.
Data integration is mostly about collection. Imagine pouring different juices—apple, orange, grape—into one big punch bowl. Integration is the process of pulling data from various sources and consolidating it into a single, central location. It’s often a one-way street, focused on just getting everything in one place.
Interoperability, on the other hand, is a dynamic, two-way conversation. It’s the ability for different systems to not only exchange data but to actually understand and use that information meaningfully on the spot. It’s not just about having the data; it’s about making it instantly actionable for a doctor or a nurse.
Think of it this way: integration gathers all your books into one library. Interoperability ensures any visitor can instantly read and understand every book, no matter what language it was originally written in.
That ability to act on shared information in real-time is what makes true interoperability so powerful.
How Do Standards Like FHIR and DICOM Work Together?
This is another fantastic question because it highlights how specialized these tools really are. FHIR and DICOM aren't competitors; they're partners, each designed to handle a different—but equally critical—piece of a patient's story.
FHIR is the modern, flexible standard for just about all clinical and administrative data. It handles things like patient demographics, lab results, medication lists, and allergy information. Because it’s built on modern web technologies, it’s perfect for powering patient-facing mobile apps and enabling quick, specific data requests between different EHRs.
DICOM, meanwhile, is the undisputed heavyweight champion of medical imaging. It governs every single aspect of an MRI, CT scan, or X-ray, from the pixel-level data to the patient information embedded within the image file. Its sole purpose is to preserve the diagnostic quality and integrity of medical images as they move between machines and systems.
Here’s how they team up in a real-world scenario:
- A patient gets an MRI. The machine captures and saves the scan as a DICOM file.
- A radiologist opens that DICOM file in a specialized viewer to analyze it and write their diagnostic report.
- The text of that report, or maybe a simple link to the imaging study, is then sent from the radiology system to the primary care physician’s EHR using a lightweight FHIR message.
They perfectly complement each other. This is where expert integration becomes so important. At PYCAD, this is exactly what we do—we build custom web DICOM viewers and integrate them into medical imaging web platforms, creating a seamless bridge between complex imaging data and the broader clinical workflow.
What Is the Biggest Challenge for Smaller Clinics?
For smaller private practices and independent clinics, the journey toward interoperability often comes down to two massive hurdles: cost and a lack of dedicated IT resources. The financial and technical gap between a local clinic and a large hospital network can feel like a chasm.
Big health systems can pour money into custom software development and hire entire teams of IT specialists to manage complex EHR integrations. They have the scale to demand better tools from vendors and the capital to invest in the right infrastructure.
Smaller practices, however, run on much tighter margins. They often have to make do with off-the-shelf EHRs that might have limited data-sharing features. The price tag for custom development, migrating decades of data, and training staff on new systems can be simply out of reach. This resource gap is one of the main reasons that truly universal interoperability of electronic health records is still a work in progress.
This is precisely why the industry-wide push for open, standardized APIs like FHIR is so crucial. These standards are designed to lower the barrier to entry, making powerful data exchange tools more affordable and easier for everyone to implement. They are helping to level the playing field, ensuring that top-tier, connected care isn’t a luxury reserved for only the largest players.
At PYCAD, we’re passionate about breaking down these barriers, especially in the incredibly complex world of medical imaging. Our expertise in building secure, integrated platforms helps healthcare organizations of all sizes finally unlock the full potential of their data. To see how we've helped others achieve seamless data exchange, we invite you to explore our portfolio of work.