Imagine a dedicated, expert assistant for every radiologist—one who has meticulously analyzed millions of scans to catch even the faintest signs of trouble. This isn't a glimpse into the future; it's the reality of a mammogram with CAD (Computer-Aided Detection), a genuine breakthrough in women's health that is fundamentally changing how we approach early breast cancer detection.
The Second Expert Eye in Every Mammogram

In the ongoing mission to find breast cancer earlier and more accurately, technology has become an essential partner. A mammogram with CAD brings a sophisticated 'second pair of expert eyes' to the review process. This powerful synergy between human expertise and machine intelligence enhances a radiologist's ability to spot potential concerns with much greater confidence.
This guide will walk you through the evolution of this incredible tool, from its early days of simple algorithms to the advanced deep learning systems we see today. We'll explore its real-world impact on patient outcomes and see how the concept of a 'second expert eye' is being brought to life by advanced AI diagnostic tools like Diagnoo, which are designed to support clinicians every step of the way.
Uniting Hope and Technology
At its heart, CAD technology is about elevating a radiologist's skill, not replacing it. Think of it as a safety net that meticulously scans every image for patterns that the human eye might overlook during a manual review. This is especially vital when you consider that approximately 43 million mammography procedures are performed in the U.S. each year.
The integration of CAD serves several critical functions in modern radiology:
- Highlighting Suspicious Areas: The software automatically flags regions of interest—like tiny microcalcifications or subtle masses—that deserve a closer look.
- Improving Detection Rates: By drawing attention to these subtle abnormalities, CAD can increase the chances of finding cancers at their earliest, most treatable stages.
- Providing Confidence: It serves as a verification tool, giving radiologists an added layer of assurance in their diagnostic decisions and confirming their findings.
This technology empowers radiologists to work more effectively, blending their irreplaceable clinical judgment with the analytical power of AI. It’s a partnership that directly translates to better patient care and more hopeful outcomes.
The Role of Advanced Visualization
Of course, for these AI-driven insights to be valuable, they have to be presented clearly and seamlessly within the radiologist's existing workflow. This is where advanced viewing platforms make all the difference. For a deeper dive into this topic, feel free to explore our detailed guide on https://pycad.co/computer-aided-diagnosis/.
This critical last step is where we at PYCAD come in. We specialize in building custom web DICOM viewers and integrating them into medical imaging web platforms, making sure the vital information from a mammogram with CAD is displayed intuitively. By fusing powerful analytics with thoughtful, user-centric design, we help create a diagnostic environment where technology truly serves the expert. You can see examples of our work on our portfolio page.
It's a journey that shows how hope and technology can come together, making early detection more powerful than ever before.
From Simple Flags to Intelligent Insights
To really get a feel for the power of a modern mammogram with CAD, it helps to look back at where it all started. This technology has come an incredibly long way, transforming from a simple digital assistant into a true diagnostic partner for radiologists.
Think of the earliest CAD systems as a basic spell-checker for medical images. They ran on a fixed set of rules, hand-coded by engineers to spot obvious red flags. These systems were told to search for specific things, like unusual density patterns or well-defined shapes that didn’t quite look normal.
It was a helpful first step, but this rule-based logic had its fair share of problems. The systems were notoriously "noisy," often creating a high number of false alarms by flagging harmless features that just happened to meet their rigid criteria. The technology pointed us in the right direction, but it lacked the sophistication to grasp the subtle complexities of breast tissue.
The Leap to Learning-Based AI
The real game-changer came with the rise of deep learning and artificial intelligence. Today’s AI-CAD is a different beast entirely. It's less like a spell-checker and more like a seasoned co-pilot who has learned from millions of hours of flight time.
These advanced systems aren't just following a checklist. They are trained on immense datasets of mammograms, teaching themselves to recognize the incredibly subtle patterns, textures, and asymmetries that are often invisible to the human eye. This is the fundamental split:
- Traditional CAD: Followed explicit, pre-programmed rules.
- Modern AI-CAD: Learns from vast amounts of real-world data.
This learning-based approach allows the AI to develop a deep, almost intuitive sense of what might be a malignancy—much like a radiologist does over decades of experience.
Seeing the Unseen
This incredible knack for pattern recognition is where modern AI makes its mark. It can pinpoint early-stage cancers that might otherwise go unnoticed, especially in dense breast tissue or other complex cases. And this isn't just theory; the data backs it up.
Studies show that artificial intelligence–aided computer-assisted detection (AI-CAD) can dramatically improve the detection of cancers radiologists initially missed. One analysis of nearly 6,500 mammograms found that AI-CAD correctly identified 5 out of 9 cancers missed in the first reading—a 17.9% boost in detection. While this sensitivity came with more false positives, it proves the AI’s power to catch what the human eye might miss, as you can learn more about from the study's findings.
By processing millions of images, AI systems build a deep, data-driven intuition for spotting anomalies. They don't just see pixels; they see context, history, and the subtle language of pathology written within the image.
This isn't about just flagging dots on a screen. It's about adding a layer of insight that complements the radiologist's own expertise. The AI might draw attention to an area that seems unremarkable at first, but which shares subtle traits with thousands of confirmed cancer cases it has analyzed before.
Of course, presenting these powerful insights effectively is a challenge in itself. At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms because we know that even the best AI is useless without a clear, intuitive interface for the clinician. You can see how we approach user-focused design on our portfolio page. This journey from simple flags to intelligent insights isn't just an upgrade—it's a monumental step forward, making the mammogram a more powerful tool for early detection than ever before.
How AI Is Changing Patient Stories for the Better
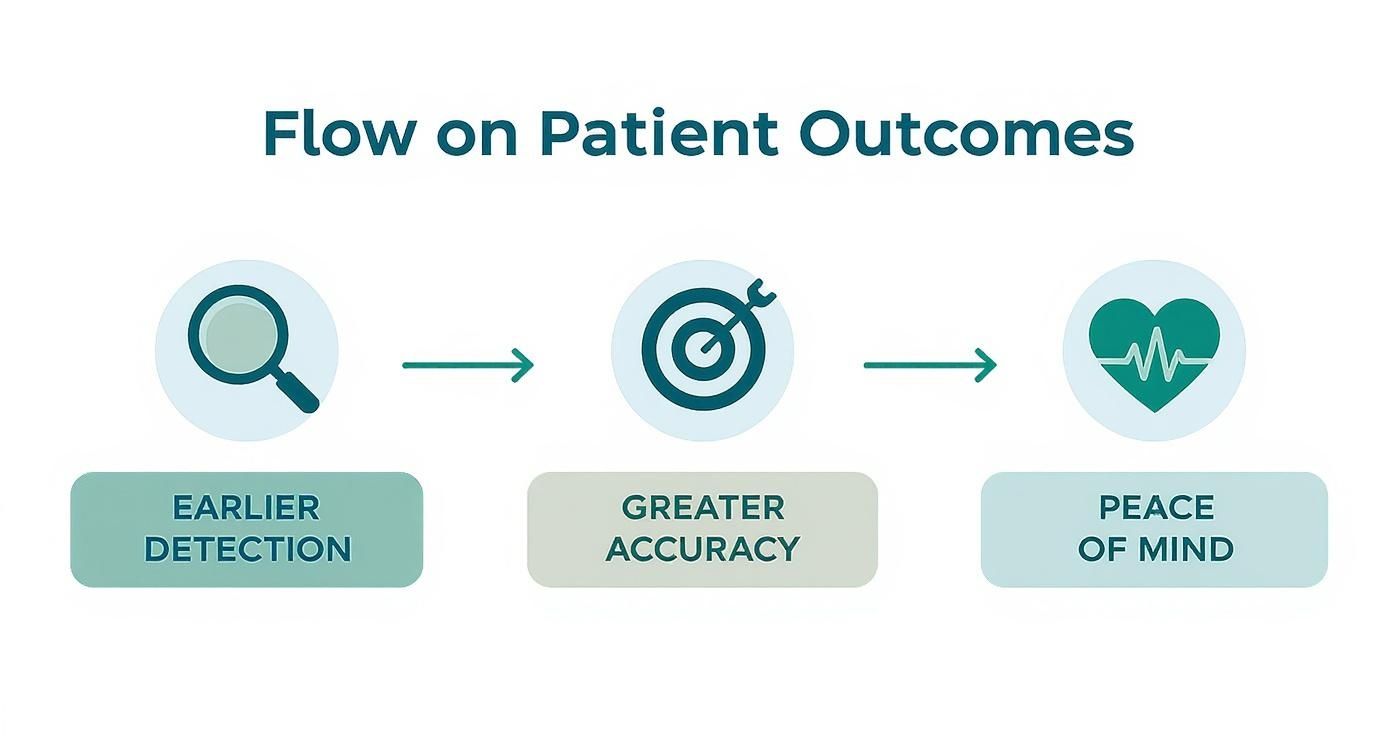
When a patient hears their exam is a mammogram with CAD, it offers a powerful sense of reassurance. It means their screening is getting a second, incredibly diligent look, marrying the seasoned expertise of a radiologist with the analytical power of artificial intelligence. This isn't just a technical upgrade; it's a fundamental shift toward better clinical outcomes—finding cancer earlier, with more certainty, and giving patients invaluable peace of mind.
The clinical proof backing AI's impact is not just promising; it's tangible and growing every day. The data clearly shows that these sophisticated systems are making a real difference, particularly when the diagnostic path gets tricky and every tiny detail counts.
Finding Cancers Hiding in Plain Sight
One of the biggest hurdles in mammography is reading images of dense breast tissue. On a mammogram, dense tissue shows up as white, the very same color as a potential tumor. This creates a natural camouflage that can easily mask the earliest, most treatable signs of cancer. This is precisely where AI’s incredible ability to see subtle textural differences becomes a game-changer.
AI algorithms, after learning from millions of diverse mammograms, can spot microscopic patterns and asymmetries that are often invisible to the human eye. This directly tackles one of the most significant weaknesses in traditional screening, helping to drive down the rate of false negatives—when a cancer is there but gets missed. By highlighting these incredibly subtle areas, AI acts as a safety net, ensuring even the faintest whispers of malignancy get the radiologist's full attention.
We’re not just talking theory here; the evidence is compelling. A major study from South Korea's national screening program, involving 24,543 women, put this to the test. Radiologists working with AI achieved a cancer detection rate of 5.70 per 1,000 exams. That's a 13.8% jump compared to the 5.01 per 1,000 rate for radiologists reading on their own—a statistically significant improvement. You can explore the full study findings to see the data for yourself.
The Radiologist and AI: A Powerful Partnership
It's crucial to see AI for what it is: a brilliant co-pilot, not an autopilot. This technology is designed to enhance and support the irreplaceable judgment of a radiologist, never to replace it. While AI is a master of detection, it can sometimes raise a flag for a benign feature, leading to a false positive.
This is where the human expert is absolutely essential. The radiologist brings clinical judgment, patient history, and years of medical wisdom to the table. They are the ultimate authority, discerning a true cause for concern from a technological false alarm.
This synergy creates a powerful diagnostic duo, playing to each other's strengths:
- AI's Power: Unwavering, data-driven pattern recognition that never gets tired and catches what might otherwise be missed.
- Radiologist's Wisdom: Deep contextual understanding, clinical experience, and the nuanced decision-making that only a human can provide.
This collaborative future of breast imaging requires tools built for the task. At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms, creating a seamless workspace where radiologists can intuitively interact with AI findings. A well-designed viewer makes all the difference, presenting AI-generated data in a way that supports, rather than complicates, the diagnostic process. You can see how we prioritize user-centric design in our portfolio of work.
Ultimately, a mammogram with CAD means a radiologist is armed with the best information possible. This blend of human intellect and machine precision is actively rewriting patient stories, turning uncertainty into clarity and leading to better, more hopeful outcomes every single day.
Weaving AI Into the Clinical Workflow
Bringing a powerful mammogram with CAD system into a clinic isn’t just about flipping a switch on new software. It’s about carefully weaving this technology into the daily rhythm of the diagnostic process. When done right, you create a workflow that’s not just faster, but fundamentally smarter. This is where the true power of AI comes alive, transforming raw data into life-saving insights.
At the heart of this entire operation are the industry standards that allow everything to communicate. Medical images, like mammograms, are created and shared using the DICOM (Digital Imaging and Communications in Medicine) standard. Think of it as the universal language for medical imaging, ensuring a scan from one machine can be read on any other. These images live inside a PACS (Picture Archiving and Communication System), which is essentially the digital heart of a radiology department. If you want to dive deeper into this foundational piece, our guide on effective PACS integration strategies is a great place to start.
No More Jumping Through Hoops
So, how does the radiologist actually see what the AI found? The real breakthrough comes from moving beyond clunky, separate reports. The goal is to eliminate any friction—no toggling between windows, no cross-referencing a text file. The best systems overlay the AI’s analysis directly onto the mammogram, right inside the radiologist's preferred viewing software.
This creates a single, powerful view. The expert sees the original image and the AI's highlighted areas of concern all at once, in a single glance. This is where a one-size-fits-all approach falls short and custom solutions become essential.
This smooth, integrated process isn't just about efficiency; it's about better patient outcomes. It’s about finding cancer earlier and more accurately, which ultimately gives patients much-needed peace of mind.
The takeaway here is simple: a fluid workflow is a clinical advantage. It directly links the elegance of the technology to the quality of patient care.
The Power of a Purpose-Built Workspace
A generic DICOM viewer shows you an image. A purpose-built platform, on the other hand, turns the radiologist's monitor into an intelligent command center. At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms to create this exact kind of intuitive experience. Our goal is to make the technology feel less like a tool and more like a trusted colleague. You can view our projects on our portfolio page.
A well-designed workflow doesn't just present data; it tells a story. It allows the radiologist to interact with AI findings fluidly, drilling down into areas of concern, comparing with prior studies, and making a final judgment with all the evidence in one place.
A truly connected system brings everything together, making the entire clinical ecosystem smarter. Here’s a look at how the pieces connect in a seamless flow:
- The Scan: A mammogram is taken, and the resulting DICOM image is sent straight to the PACS.
- The Analysis: The AI-CAD system automatically pulls the new image, analyzes it for potential anomalies, and generates its findings.
- The View: The radiologist opens the study in a custom DICOM viewer. They see the original mammogram, but with the AI's suggestions displayed as an interactive layer on top.
- The Report: After reviewing the AI's marks—either accepting or dismissing them—the radiologist completes their final report. These findings are then sent to the reporting software and linked to the patient's electronic health record (EHR).
This beautifully simple process saves precious minutes, slashes the risk of human error, and keeps the focus exactly where it needs to be: on the patient. By building a workflow that is as intelligent as the AI itself, we create an environment where technology and human expertise can work together in perfect sync to deliver the best possible care.
Choosing and Implementing a CAD System
Deciding to bring a mammogram with CAD system into your practice is a big step—one that holds the promise of better patient outcomes and greater diagnostic confidence for your team. This isn't just about buying new software; it's about fundamentally enhancing the way you work, blending human expertise with powerful artificial intelligence. Making the right choice means having a clear plan, from rigorously evaluating a system’s performance to making sure it fits perfectly within your daily clinical workflow.
The journey starts with a hard look at the clinical performance data. A vendor’s claim of "high accuracy" isn't enough; you need to dig into the details. Sensitivity tells you how well the AI spots actual cancers, while specificity reveals how good it is at correctly identifying healthy tissue. A system that’s highly sensitive but has low specificity can create a storm of false positives, leading to unnecessary anxiety for patients and a heavier workload for radiologists. The sweet spot is finding a system that achieves a strong balance between the two.
Validating for Equity and Performance
Beyond the top-line numbers, it’s absolutely essential to see how an AI performs on data that mirrors your own patient community. An algorithm trained mostly on one demographic might not be as reliable for others. A truly great system is one that delivers consistent, high-quality results for all patients, no matter their age, ethnicity, or breast density. This commitment to validation ensures the technology you adopt becomes a tool for closing health disparities, not making them wider.
Major recent studies have driven this point home. The ASSURE study, for example, examined AI-powered screening workflows and found that combining advanced AI with 3D mammography boosted the cancer detection rate by a remarkable 21.6% over 3D mammography alone. What’s more, the study confirmed these gains across diverse populations, including over 150,000 Black women. For women with dense breasts, the improvement in detection was even higher at 22.7%. This is the kind of real-world, validated performance that builds trust and makes a tangible difference. You can discover more about these powerful findings and see what this technology is capable of.
Your Implementation Checklist
Once you’ve picked the right system, a well-thought-out implementation plan is what will turn its potential into reality. A smooth rollout encourages your team to embrace the new technology and ensures it becomes an asset from day one.
Here’s a practical checklist to guide you through the process:
- Technical Infrastructure Assessment: First, make sure your PACS, network, and viewing workstations can handle the data from the new CAD system. A technical bottleneck can quickly frustrate users and kill momentum.
- Workflow Redesign: Think through exactly how the AI will analyze images and how its findings will be presented to your radiologists. At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms to make this step feel effortless. Our goal is to present AI insights in a way that feels natural and intuitive, as you can see on our portfolio page.
- Comprehensive Staff Training: Don’t just train the radiologists—include your technologists and administrative staff. When everyone understands their part in the new process, it builds a culture of confidence and teamwork.
- Regulatory and Compliance Review: Confirm the system you've chosen has all the necessary regulatory clearances. Understanding the requirements is non-negotiable. For a deep dive into how devices like these get to market, the FDA approval process for medical devices is a must-read.
- Phased Go-Live and Feedback Loop: Think about starting with a pilot program before a full-scale launch. This lets you collect feedback from your first users, iron out any wrinkles, and fine-tune the workflow for the best possible clinical value.
Navigating the regulatory path is a critical step in bringing any new medical device into clinical use. Ensuring a system has proper clearance is not just a box to check—it's a foundational element of patient safety and provider confidence.
For anyone looking to get a firmer grasp on this specific area, we’ve put together a detailed guide on the https://pycad.co/medical-device-fda-approval-process/ that offers some incredibly useful insights. By following a structured approach, you can confidently choose and roll out a CAD solution that elevates your clinical capabilities, integrates smoothly, and truly empowers your team to deliver the best possible care.
Your Mammogram with CAD Questions, Answered
New technology always brings questions, especially when it involves something as personal as a mammogram. It’s completely natural for both patients and clinicians to wonder how tools like Computer-Aided Detection (CAD) fit into the picture. We're here to offer clear, simple answers to demystify the process of having a mammogram with CAD and build your confidence in it.
The key thing to remember is that this technology isn't meant to replace the human expert. It’s designed to empower them. This is all about the powerful partnership between a skilled radiologist and intelligent software, working together for earlier, more accurate detection.
Will a CAD Mammogram Feel Different for Me as a Patient?
Not in the slightest. From your perspective as a patient, the experience is exactly the same as a standard mammogram. The advanced analysis is all software-based and happens completely behind the scenes after your images are taken.
You won’t feel or see anything different during the exam itself. The technology is designed to give your radiologist a deeper look at the images without changing the familiar screening procedure for you one bit. The focus remains, as always, on your comfort and safety.
If AI Is Used, Does a Radiologist Still Read My Mammogram?
Absolutely. This is the most important point to understand. A qualified radiologist always makes the final diagnosis. The AI is a powerful decision-support tool—think of it as an incredibly vigilant assistant—but it never replaces the deep knowledge and clinical judgment of a medical expert.
The AI acts as a second set of eyes, methodically scanning the images and flagging any subtle areas that might need a closer look. It’s the radiologist who then applies their years of training and experience to interpret those findings, separating what’s important from what isn’t, and ensuring the final report is as accurate as possible.
How Reliable Is the AI in Detecting Breast Cancer?
Modern AI systems for mammography are remarkably reliable. Major clinical studies have confirmed they significantly improve cancer detection rates, especially when it comes to finding those very subtle, early-stage cancers that can be difficult to spot.
But no single tool is perfect. AI can sometimes flag a benign area (a 'false positive'), which is precisely why the radiologist's oversight is non-negotiable. They are the seasoned experts who can tell the difference between a true concern and a false alarm, ensuring the highest level of accuracy and preventing unnecessary stress or follow-ups.
This partnership plays to the strengths of both human and machine intelligence. It creates a diagnostic process with checks and balances, making it far more robust than either could be on its own.
What Is the Difference Between CAD and a DICOM Viewer?
That's a great question that gets right to the heart of how these tools work in the real world. Let’s break it down with an analogy.
Think of the CAD system as the powerful 'engine' that analyzes the mammogram image (which is in a standard format called DICOM) to produce its findings. The DICOM viewer, on the other hand, is the 'dashboard' where the radiologist sees everything. A basic viewer just shows the image.
But a custom, integrated DICOM viewer—like the ones we develop at PYCAD—is much more. We build custom web DICOM viewers and integrate them into medical imaging web platforms. This means the CAD 'engine's' findings appear directly on the 'dashboard.' The radiologist sees the AI's highlighted areas right on top of the mammogram, all in one seamless workspace. It’s the difference between just looking at a picture and truly interacting with intelligent data.
At PYCAD, we believe the best medical technology is the kind that feels intuitive and supportive to the clinicians who rely on it every day. By creating custom platforms that bring AI insights directly into their workflow, we help medical professionals deliver the best care possible. To see how we approach building these fluid, user-focused solutions, we invite you to explore our portfolio.