Electronic Health Records (EHRs) were supposed to be our ticket to a new era of medicine. The dream was simple: perfect, portable patient records at our fingertips. But anyone who's actually worked on the front lines knows the reality has been… well, a little more complicated.
The disadvantages of electronic health records are not just minor inconveniences. We're talking about staggering costs that can cripple a clinic, workflow nightmares that fuel clinician burnout, and data integrity problems that can put patient safety on the line. These systems, designed to help, often feel like a source of constant friction.
The Hidden Flaws in Digital Healthcare
The shift from paper to digital was meant to be a great leap forward. The goal was admirable—to build a single, reliable source of truth for every patient's journey. Yet, the systems we got often feel more like a step sideways. Instead of making life easier, many EHRs have added layers of frustrating complexity, burying clinicians in administrative tasks.
This guide is about facing those challenges head-on. We're going to peel back the curtain and look at the real-world consequences of this digital transition.
The issues aren't just theoretical; they have a daily impact on finance, workflow, and safety. Here’s a quick overview of what we'll be diving into.
Core EHR Challenges at a Glance
| Challenge Category | Impact on Healthcare | Real-World Consequence |
|---|---|---|
| Financial Burden | High initial and ongoing costs create barriers to adoption and strain budgets. | A small practice delays upgrading essential medical equipment to afford its yearly EHR license fees. |
| Workflow Disruption | Clunky interfaces and excessive data entry lead to lost time and frustration. | A physician spends an extra two hours after their shift on documentation, a phenomenon known as 'pajama time.' |
| Patient Safety Risks | Data silos, copy-paste errors, and alert fatigue can lead to dangerous mistakes. | An allergy noted in one hospital's EHR is missed when a patient is transferred to another system, risking an adverse reaction. |
| Interoperability Failure | Systems can't "talk" to each other, creating fragmented patient histories. | A radiologist can't easily access prior scans from a different imaging center, forcing a duplicate MRI. |
| Security & Privacy | Centralized digital records become high-value targets for cyberattacks. | A data breach exposes the sensitive health information of thousands of patients, leading to identity theft. |
These challenges aren't isolated—they feed into one another, creating a web of inefficiency and risk.
This guide will unpack each of these disadvantages, but we'll also look at how to solve them. It's about turning these complex systems into the intuitive, life-saving tools they were always meant to be.
The diagram below maps out how these core flaws spiral into tangible problems across the healthcare system.
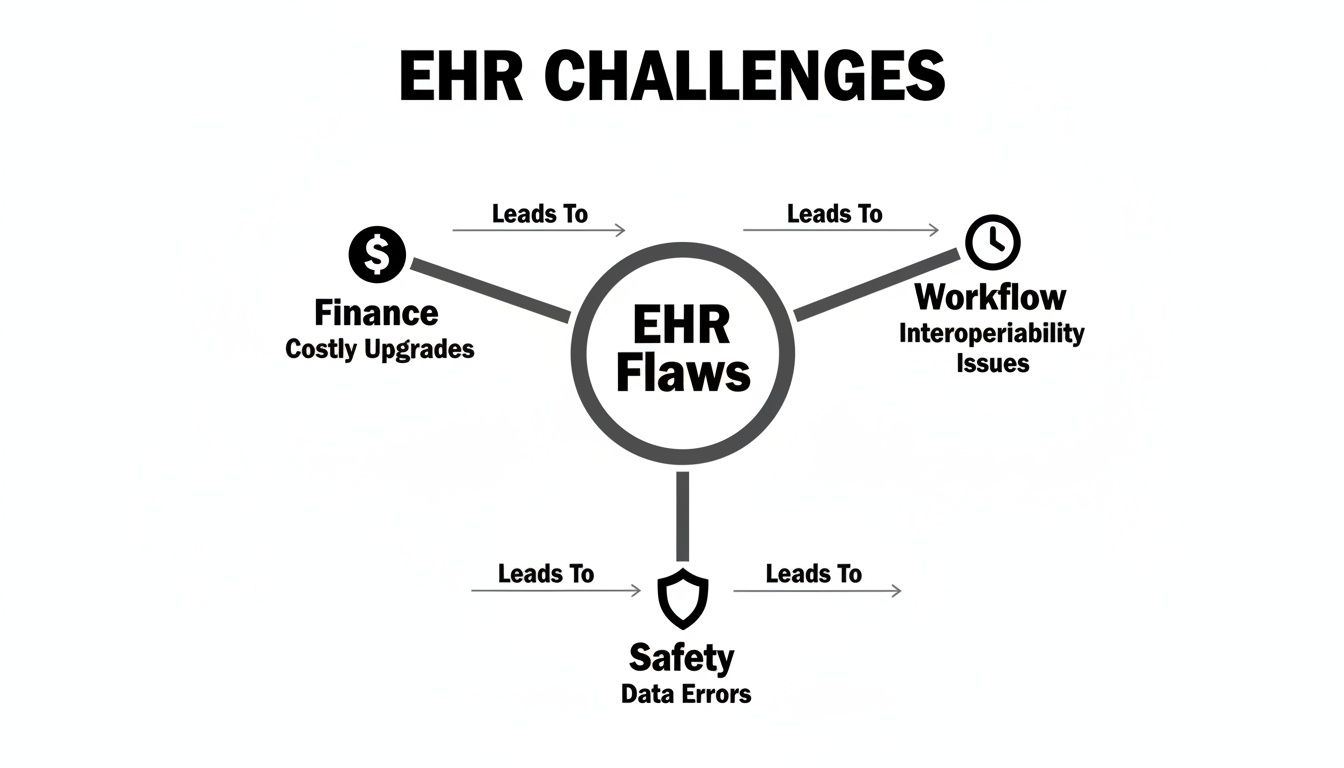
As you can see, the issues are deeply connected. A clunky workflow doesn't just waste time; it can lead to errors that impact patient safety. Understanding this is the first step toward building something better.
At PYCAD, we live in this world every day, focusing on the particularly tricky challenges in medical imaging. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, making data accessible and actionable. You can see how we turn frustrating systems into elegant solutions on our portfolio page.
Now, let's start by digging into one of the biggest roadblocks of all: the great disconnect of interoperability.
The Great Disconnect: Interoperability
Imagine a world-class library filled with brilliant books, but every single one is written in a unique, untranslatable language. A doctor could hold a patient's entire medical history in their hands, yet understand none of it. This isn’t some far-off sci-fi plot; it's the daily reality of healthcare's interoperability problem, easily one of the most significant disadvantages of electronic health records.
The core promise of EHRs was a single, seamless patient story. What we got instead was a digital Tower of Babel. Each hospital, clinic, and lab often ends up with its own proprietary system that simply refuses to talk to the others. This creates isolated islands of data, leaving physicians to make critical decisions with a dangerously incomplete picture.
This disconnect is far more than a technical headache. It has profound, real-world consequences that ripple through every level of patient care, forcing clinicians into a frustrating cycle of chasing down faxes, making endless phone calls, and re-entering data by hand—all while the patient waits.
The Real Cost of Digital Silos
When patient data is trapped in separate systems, the financial and clinical costs skyrocket. A patient might show up at an emergency room and get a costly, radiation-heavy CT scan, even though an identical one was done at another hospital just last week. The ER team simply can't get their hands on it. This isn't just wasteful; it's a systemic failure.
This breakdown in communication leads directly to:
- Redundant and Expensive Testing: Patients are subjected to repeated labs, imaging scans, and other procedures simply because their previous results are locked away somewhere else.
- Dangerous Delays in Treatment: Critical time is lost as specialists wait for referring physicians to send over vital history, delaying diagnoses and life-saving interventions.
- Massive Administrative Waste: Staff spend countless hours manually piecing together information from different sources, a chore that modern technology was supposed to eliminate.
The scale of this problem is staggering. As of 2021, a mere 46% of U.S. hospitals had achieved even basic EHR interoperability. This gap fuels an estimated $30 billion in annual waste for the U.S. healthcare system alone. It’s a direct consequence of these digital walls.
A Radiologist's Blind Spot
Nowhere is this disconnect more glaring than in medical imaging. Picture a radiologist trying to interpret a complex MRI. Without the ability to see the referring physician’s notes, the patient’s prior imaging studies, or their complete clinical history, the radiologist is essentially flying blind. They can see the pixels on the screen, but they lack the full story needed for a truly accurate diagnosis.
This is the exact challenge we live and breathe at PYCAD. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, creating a fluid bridge over these data chasms. Our mission is to make sure a radiologist can pull up a patient's entire imaging history and relevant clinical data with a single click, right inside the platform they already use. You can see how we tackle these complex integration problems by checking out our portfolio page.
Interoperability is not a feature; it's the fundamental bedrock upon which patient safety is built. When systems fail to communicate, the first casualty is the cohesive, continuous care every patient deserves.
This fundamental barrier undermines the very purpose of a unified health record. To truly move forward, the industry has to address this digital divide head-on. For a deeper dive into this critical issue, take a look at our guide on the interoperability of electronic health records. This failure to connect systems is more than a flaw; it’s a systemic risk that introduces the next major disadvantage: the creation of dangerous medical errors.
When Digital Records Create Medical Errors

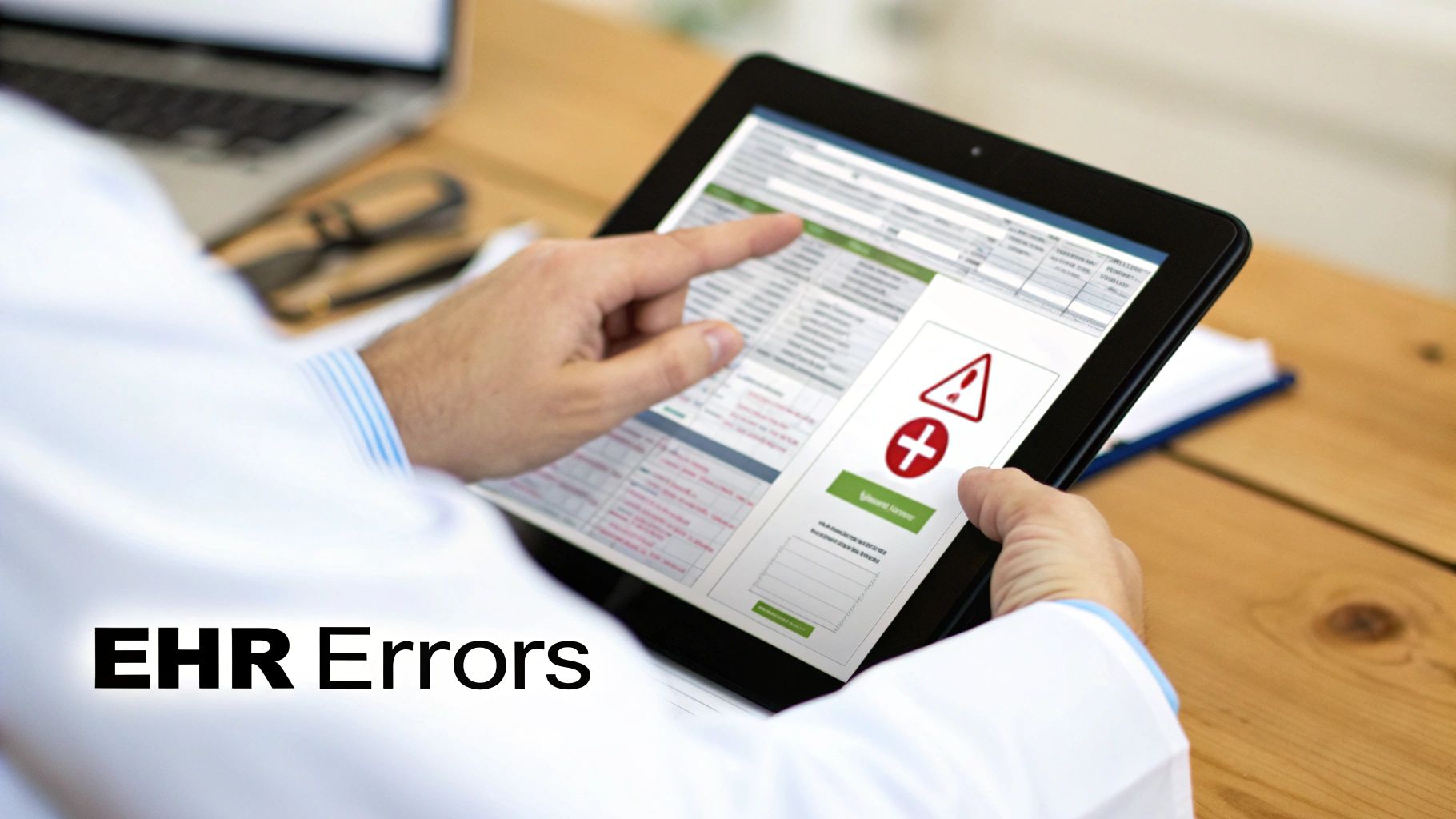
Electronic Health Records were supposed to be our fortress against human error. The dream was simple: a future where digital precision would make misplaced charts and messy handwriting things of the past. But what we've found is a painful irony. These very systems have given rise to a new, more subtle kind of mistake—what many now call "EHRrors."
This is one of the most sobering disadvantages of electronic health records: the very tool designed for accuracy can, in fact, become a source of systemic error. Instead of just stopping mistakes, a poorly designed system can introduce, hide, and even multiply them across a patient's entire medical journey. It's like a digital rumor—one wrong entry gets copied, and before you know it, that falsehood is treated as fact everywhere.
Think about it. A small data entry slip-up, like a wrong allergy or a misplaced decimal in a dosage, no longer stays put in a single paper file. In the interconnected world of EHRs, it can be copied and pasted across dozens of reports, quietly shaping the decisions of countless clinicians for years.
The Anatomy of a Digital Mistake
These errors aren't just random glitches. They often grow from specific design flaws and user habits that EHRs can unintentionally encourage. Three culprits, in particular, are notorious for weaving a web of bad information.
- The Copy-Paste Cascade: Under immense time pressure, it’s all too easy for clinicians to use "copy forward" functions to pull old notes into a new visit. It’s efficient, but it can also clone outdated information—like a resolved condition or a discontinued medication—making it look current and creating a distorted picture of the patient's health.
- Pervasive Alert Fatigue: EHRs are famous for their constant barrage of pop-ups and warnings. When you're bombarded with digital noise all day, you naturally become desensitized. Clinicians start to ignore or dismiss alerts, which means they could easily miss a truly critical one about a dangerous drug interaction or a life-threatening allergy.
- Clunky and Mismatched Interfaces: So many systems rely on rigid data fields that just don't match the fluid, complex reality of patient care. A doctor might be forced to pick from a dropdown menu that doesn't quite capture a patient's symptom, leading to a record that's technically complete but clinically misleading.
These seemingly small issues build on each other over time, slowly eroding the integrity of the patient record. And this isn't just a theoretical worry. The data shows that as many as every other patient—around 50%—has found a serious EHRror in their own records. Even more concerning, over half of healthcare professionals expect most patients will run into these kinds of mistakes, from wrong medications to outdated vital signs.
The Patient's Perilous Perspective
For a patient, finding a life-threatening mistake in your own chart is a deeply unsettling experience. Imagine seeing a medication you're dangerously allergic to listed as "active," or discovering that someone else's lab results have been mixed into your file. It shatters the very trust that is so essential for healing.
The greatest danger of EHRrors is their legitimacy. An error printed in a clear, digital format carries an unearned authority that a scribbled note on a paper chart never could. It looks official, it feels correct, and it is dangerously easy to believe.
This challenge really brings home just how critical it is to maintain the highest standards for medical information. To go deeper on this, you can read our guide on data quality in healthcare. Protecting the integrity of a patient's story is non-negotiable, especially when you're dealing with complex data like medical images.
At PYCAD, we know that preventing these errors means building tools designed for the reality of clinical work. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms. Our approach is built around ensuring that vital imaging data is presented with absolute accuracy and clarity, cutting down the risk of misinterpretation. By creating intuitive, seamless workflows, we empower clinicians with the right information at the right time. You can see our solutions on our portfolio page.
The Human Cost of Inefficient EHR Design
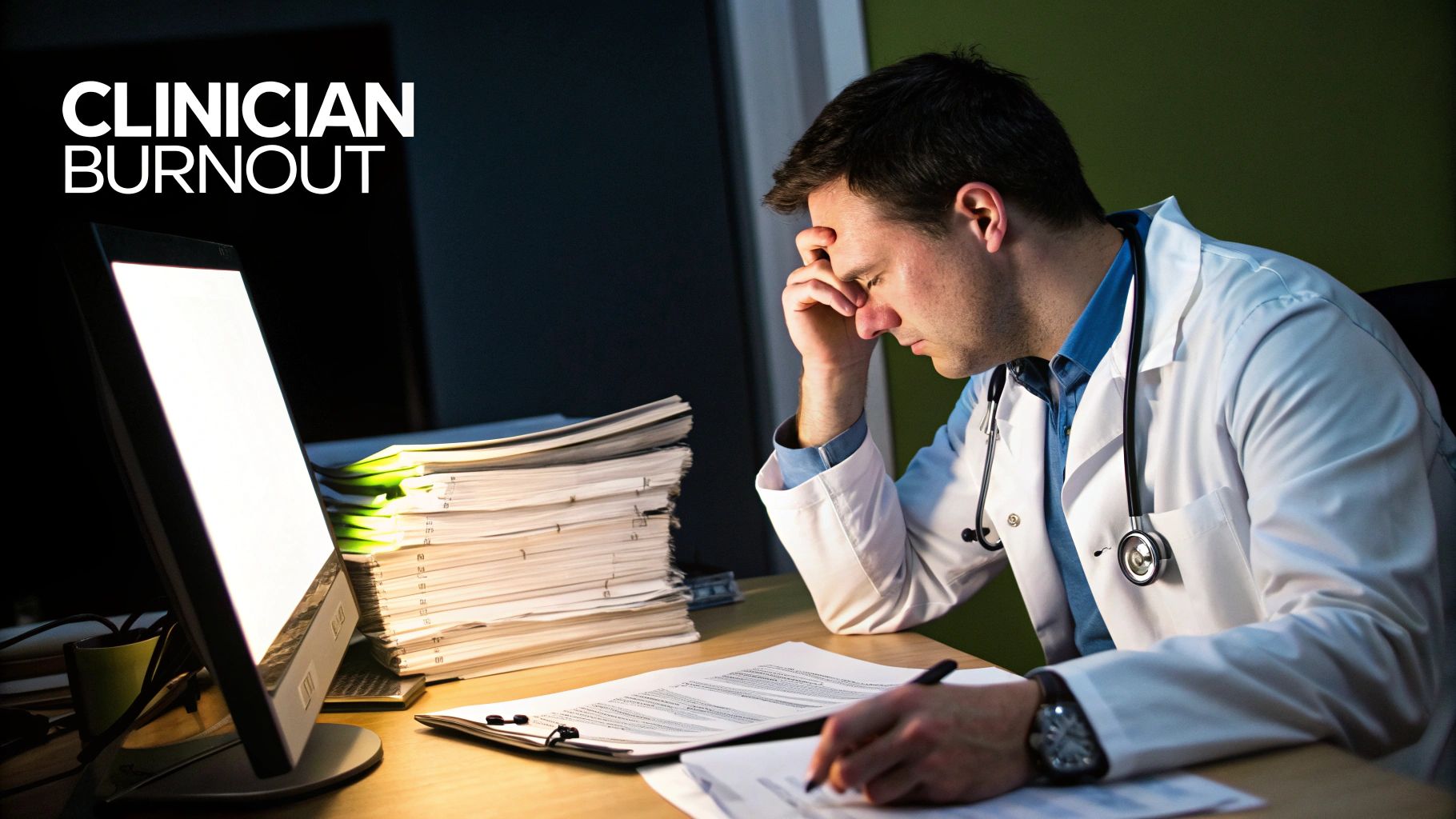
Forget the technical glitches for a moment. Beyond the data errors and system crashes, the most profound failure of many electronic health records is the deep, human toll they take on clinicians. These systems were supposed to liberate doctors and nurses, but for many, they've become digital taskmasters, fueling a quiet crisis of burnout that’s eating away at the very heart of medicine.
The problem isn't the technology itself. It’s the design—a design that too often prioritizes billing codes and administrative metrics over the fluid, deeply human nature of patient care.
When a physician has to spend more time clicking boxes and navigating convoluted menus than making eye contact with a sick patient, something vital is lost. This isn't just a minor annoyance; it’s an erosion of the sacred doctor-patient relationship, replaced by a relationship with a screen.
The Rise of Pajama Time
This constant administrative weight has given rise to a phenomenon known grimly among clinicians as "pajama time." It's the unpaid, unseen work that physicians and nurses are forced to do from home, long after their shifts should have ended, just to catch up on documentation.
These are the hours spent finishing charts, signing off on orders, and clearing inboxes—the very tasks the cumbersome EHR made impossible to complete during a packed day. "Pajama time" is more than just working late; it’s a symptom of a broken system. It steals personal time, disrupts family life, and slowly turns a calling into a chore.
This relentless demand fuels a dangerous trifecta of professional distress:
- Exhaustion: The cognitive load of wrestling with a non-intuitive system all day, followed by hours of administrative catch-up, is utterly draining.
- Cynicism: When the tools you’re given seem to work against the goal of healing, it's easy to become disillusioned and detached.
- Moral Injury: This happens when you’re forced to act against your better judgment. A system that makes you prioritize data entry over being present with your patient feels like a betrayal of your core mission.
These aren't just feelings; they are measurable outcomes of poor EHR usability. In fact, a study of 128 healthcare providers revealed that 74 (58%) agreed or strongly agreed that EHRs add to their daily frustration. That's a staggering number, and it shines a bright light on the technology's negative impact. You can discover more insights about the direct link between EHR design and clinician stress in the full research.
When Clicks Replace Care
The root of the problem is a matter of focus. Many EHR systems were built to be powerful data collection and billing engines, not intuitive clinical partners. The result is a workflow that feels unnatural and disruptive.
A physician’s thought process is rarely linear; it's a dynamic interplay of observation, inquiry, and intuition. Yet, EHRs often force them into rigid, step-by-step documentation that shatters the natural flow of a patient encounter.
Technology should be a quiet, competent assistant in the exam room, not the loudest, most demanding presence. When the EHR commands more attention than the patient, it has failed its primary purpose.
This constant battle with the interface is one of the most disheartening disadvantages of electronic health records. It’s what pushes talented, empathetic professionals away from the bedside and straight toward burnout.
The solution isn’t to abandon digital records but to demand better, more human-centered design. At PYCAD, we see this challenge clearly, especially in the complex world of medical imaging. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, focusing relentlessly on creating a seamless and intuitive experience.
By removing friction and placing critical information exactly where clinicians need it, our tools are designed to give time back to the provider. See the difference that user-centric design makes on our portfolio page. Ultimately, great healthcare technology should reduce burdens, not create new ones.
Bridging The Gaps With Custom Solutions
Acknowledging the deep-seated disadvantages of electronic health records is the first honest step we can take. The goal isn’t to ditch these systems entirely, but to enhance them with intelligent, targeted tools built for the people on the front lines—the clinicians. It’s about shifting our focus from the problem to the solution, especially in specialized areas like medical imaging where generic EHRs just don't cut it.
Systemic problems require specific, well-designed solutions. A one-size-fits-all EHR will never serve a radiologist, an oncologist, and a family doctor with the same level of precision. The real path forward is in building bridges—custom integrations that shore up the weaknesses of existing platforms and bring efficiency back to the clinical workflow.
This is exactly what we live and breathe at PYCAD. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, creating a seamless connection that closes the interoperability gap. Our solutions are designed to give clinicians the fast, intuitive access to critical imaging data they need, right inside the EHR environment they already use. Visit our portfolio page to see our work.
Restoring Clinical Focus Through Smart Design
The best technology should feel invisible, acting as a silent partner instead of a loud, demanding obstacle. This means getting away from clunky interfaces and information overload and designing systems that actually anticipate what a clinician needs next. For instance, why force a radiologist to log into three separate applications when a custom viewer can instantly pull all relevant prior studies and reports into a single, cohesive timeline?
This kind of thoughtful design is a direct antidote to the burnout and frustration so common in healthcare today. By putting the user experience first, we can turn digital friction into clinical momentum.
The most powerful technology is not the one with the most features, but the one that feels the most invisible. True innovation in healthcare IT is about removing barriers, not adding more clicks.
This principle is at the core of our development philosophy. We immerse ourselves in the complex workflows of medical imaging to build solutions that feel like a natural extension of a clinician's own mind. You can see how we've transformed workflows for our clients by exploring the case studies on our portfolio page.
Practical Steps Toward A Better EHR Ecosystem
Fixing the current state of EHRs is a team sport. It’s not just about writing better code; it’s about establishing better processes and being open to new technologies that fill the voids left by older, monolithic systems.
Here are a few key areas where we can make a real difference:
- Task Automation: Automating repetitive administrative work, like manual data entry, is low-hanging fruit that gives clinicians back precious time.
- Voice Recognition: Bringing in modern voice-to-text tools can slash the time spent typing notes. The benefits of medical voice charting are clear—they directly address some of the biggest EHR pain points.
- Data Migration and Integrity: When transitioning systems, ensuring data is clean and accurate is non-negotiable. Following robust data migration best practices is essential to prevent errors from spreading.
- API-Driven Integration: Using modern APIs is the key to a flexible future. It allows specialized tools to plug securely into core EHRs, creating a powerful, interconnected ecosystem.
By concentrating on these practical, real-world solutions, healthcare organizations can start to reverse the damage done by clunky technology and build a digital foundation that genuinely supports patient care.
Turning Digital Frustration Into Real Innovation
The whole EHR saga has taught us a powerful lesson: technology alone is never the magic bullet. When we look at the rampant data errors, the heartbreaking clinician burnout, and the constant interoperability failures, it's clear these aren't just tech glitches. They're a massive signpost pointing us toward a whole new way of thinking about digital health.
These persistent disadvantages of electronic health records have shone a bright light on the need to break free from rigid, one-size-fits-all systems.
The path forward has to be more human. It requires tools that are flexible, intuitive, and genuinely connected—solutions that actually support clinicians instead of burying them under a mountain of administrative busywork. This is where real progress starts: by designing technology that works for people, not the other way around.
From Problem to Possibility
To finally deliver on the original promise of EHRs, we need a fresh commitment from everyone in the game. Developers, healthcare leaders, and specialized partners have to come together to build an ecosystem that truly empowers providers and keeps patients safe. It's not about just adding more features. It's about smarter, more thoughtful design that anticipates needs and smooths out the friction in a clinician's day.
This is the philosophy that drives us at PYCAD. We see the gaps left by generic systems as opportunities to create focused, powerful solutions. For example, in medical imaging, standard EHRs often create frustrating bottlenecks and delays. That's precisely why we at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms.
True innovation doesn't come from a single massive system that tries to do everything. It comes from creating specialized, elegant tools that do one thing exceptionally well and connect seamlessly with the larger ecosystem.
Moving beyond these frustrations often takes a dedicated effort, sometimes through strategic initiatives spearheaded by a Centre for Digital Transformation of Health.
Our goal is simple: to create technology that feels almost invisible, freeing clinicians to focus completely on their patients. By building bridges over those interoperability chasms and designing for the real-world demands of specialties like radiology, we help turn digital frustration into clinical efficiency. We believe the best technology is the kind that gives time back to the people who need it most.
That original vision of a connected, efficient healthcare system is still worth fighting for. With the right partners and a renewed focus on the people using the tools, it's absolutely within our reach.
To see how we put these principles into practice to solve complex integration challenges, feel free to explore our portfolio page.
Frequently Asked Questions About EHR Challenges
Diving into the world of digital health always brings up tough questions. When you really get into the weeds, you start to see the disadvantages of electronic health records, and understanding them is the first step toward finding better solutions for everyone involved. Let's tackle some of the most common ones head-on.
What Is The Biggest Disadvantage Of EHR Systems?
If you ask ten different clinicians, you might get ten different answers, but they all point back to one colossal problem: the lack of interoperability.
Think of it like this: every hospital's EHR is a book written in its own unique, secret language. When a patient moves between hospitals, it's like trying to read a story where every other chapter is in a language you don't understand. This failure to communicate creates dangerous gaps in a patient's medical journey. It leads to redundant tests, delays in life-saving treatments, and prevents doctors from seeing the full picture they need to provide safe care. It's the central flaw that makes so many other problems, like medical errors and workflow nightmares, so much worse.
How Do EHRs Cause Physician Burnout?
EHRs are a massive contributor to physician burnout because of the sheer administrative weight they place on clinicians' shoulders. Instead of being a helpful assistant, a clunky, poorly designed EHR becomes a barrier, forcing doctors to spend more time clicking through menus than actually connecting with their patients.
This is where the infamous "pajama time" comes from—those extra hours doctors and nurses spend at home, long after their shift is over, just to finish charting. When you're constantly fighting with your tools, it drains your energy, kills your job satisfaction, and slowly erodes the very human connection that drew you to medicine in the first place.
The real problem is a design philosophy that has often prioritized billing codes and data collection over the art and flow of clinical care. When technology gets in the way of medicine, burnout is what you get.
Are Electronic Records More Secure Than Paper Records?
Not necessarily—they just face a completely different, and potentially much larger, set of risks. A paper chart might get misplaced, but a single cyberattack on an EHR can expose the private data of millions of people all at once.
Think about it: one successful ransomware attack can bring an entire hospital system to its knees, canceling surgeries and grinding patient care to a halt. This digital vulnerability means that protecting patient data isn't a one-time fix; it requires constant, expensive vigilance and sophisticated cybersecurity to stay ahead of ever-evolving threats.
Can The Problems With EHRs Be Solved?
Yes, absolutely. We can overcome many of the disadvantages of electronic health records, but it requires a fundamental shift in thinking. We need to focus on user-centered design, demand strong interoperability standards, and embrace specialized tools that fill the gaps that one-size-fits-all systems leave behind.
This is exactly what we live and breathe at PYCAD, especially in the world of medical imaging. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, creating a fluid, intuitive experience that works with existing EHRs, not against them. The solution is to build technology that serves clinicians, not the other way around. By turning digital frustration into clinical efficiency, we can finally fulfill the original promise of a truly connected and supportive healthcare ecosystem. To see our work, please visit our portfolio page.
At PYCAD, we specialize in transforming complex medical imaging workflows into simple, elegant solutions. To see how we've helped healthcare organizations overcome their biggest technology hurdles, please visit our portfolio page.