Picture a pathologist working alongside a powerful assistant—one that has scrutinized millions of slides and can spot subtle patterns the human eye might miss. That's the reality taking shape with artificial intelligence in pathology. This isn't about replacing highly trained experts; it's about giving them incredibly powerful, data-driven tools to enhance their own skills.
The New Era of AI-Powered Diagnostic Medicine
Pathology is at a crossroads. Labs are dealing with a flood of increasingly complex cases, especially in cancer diagnostics, all while facing a persistent shortage of specialists. To keep up without compromising quality, they need new approaches, and AI has stepped up as a major part of the solution.
Think of an AI model as a tireless, highly specialized apprentice. It learns by studying massive digital slide libraries, training itself to identify, count, and classify cells with a speed and consistency that's simply beyond human capability. This directly tackles some of the biggest headaches in today's diagnostic labs.
Addressing Critical Laboratory Needs
The introduction of AI isn't just about cool new tech; it's a practical response to real-world pressures. Pathologists can hand off repetitive, time-intensive tasks to these systems. This frees them up to focus their deep expertise on what truly matters: interpreting complex cases and solving diagnostic puzzles. It’s a partnership that elevates the entire process.
Here are a few areas where AI is making an immediate difference:
- Taming the Caseload: AI tools can pre-screen slides, flagging cases that show potential signs of cancer or need a pathologist's immediate attention. This helps labs triage their workflow, getting critical results back to doctors and patients faster.
- Improving Diagnostic Consistency: Let's face it, human interpretation can vary from one person to another. AI offers an objective, quantitative analysis for tasks like tumor grading, helping to standardize results across an entire department.
- Boosting Precision: Algorithms are brilliant at detecting subtle morphological clues that might otherwise go unnoticed. This acts as an invaluable "second opinion," increasing a pathologist's confidence, especially when dealing with borderline or ambiguous findings.
By taking on the meticulous, data-heavy lifting, AI gives pathologists the freedom to concentrate on the nuanced art of diagnosis. The goal is a human-AI synergy that raises the bar for both the quality and speed of patient care.
This collaboration between human experts and smart algorithms is already changing the game. For instance, in one study reviewing stomach lining biopsies, AI was able to find precancerous changes in about 5% of cases that pathologists had initially cleared. While AI isn't perfect, its ability to flag these subtle findings for expert confirmation shows its incredible value as a safety net. This synergy ultimately leads to earlier detection and better outcomes, pushing pathology into a more powerful, proactive future.
How AI Changes the Day-to-Day Pathology Workflow

To really get what artificial intelligence in pathology means, you have to look past the buzzwords and see how it actually fits into the daily grind of a lab. AI isn't some magic button; it's a series of tools that slot into different points of the diagnostic journey, from when a tissue sample first comes through the door to the final report landing on a clinician's desk. The whole point is to make the entire process smarter and more efficient.
Imagine the traditional pathology workflow as a manual assembly line. Every single step, from sorting to analysis, depends entirely on a pathologist's eyes and hands. It works, but it can create serious bottlenecks. AI introduces smart automation and quality checks along that line, helping everything move more smoothly.
Step 1: Getting Cases in the Right Order
A busy lab can get hit with hundreds of cases a day. Figuring out which ones need attention right now is a constant headache. Usually, cases are just handled in the order they show up, meaning a potentially urgent cancer case could be sitting behind a pile of routine screenings. This is the first place AI can make a huge difference.
AI algorithms can give every incoming digital slide a quick, initial scan. By analyzing the entire image for red flags, the system can instantly identify and bump suspicious cases to the top of the queue.
- Flagging Urgent Cases: The AI tags slides showing a high probability of cancer or other critical findings.
- Smarter Worklists: Pathologists get a prioritized list, so they can apply their skills to the most critical cases first.
- Faster Turnaround: This automated triage means urgent diagnoses get to doctors—and patients—days sooner.
It’s important to remember that the AI isn't making a diagnosis here. It's acting like an incredibly efficient air traffic controller for the lab, making sure the most critical flights land first.
Step 2: Taking Over the Tedious Work
Once a pathologist opens a case, some of the most critical work is also the most mind-numbing: counting cells, measuring features, and quantifying biomarkers. Tasks like counting mitotic figures to grade a tumor or calculating the percentage of cancerous cells are essential, but they're repetitive and notoriously prone to slight variations between pathologists.
This is exactly the kind of thing AI is built for. Trained on millions of examples, these tools can perform these precise, quantitative tasks with incredible speed and consistency.
Take prostate biopsies, for instance. An AI model can screen the entire slide in seconds, highlighting every area that looks suspicious for cancer. This frees the pathologist from the painstaking chore of manually scanning every single millimeter of tissue. They can jump straight to the AI-flagged regions, using their expert judgment to confirm or dismiss the findings.
AI turns tedious manual counting into an automated, data-driven task. This doesn’t just save a massive amount of time; it makes the diagnosis more objective and reproducible, cutting down on the variability between different pathologists.
Step 3: A Second Set of Eyes for Diagnosis
After the initial sort and number-crunching, the pathologist’s deep expertise takes center stage for the final interpretation. In this phase, AI acts less like an automator and more like a deeply knowledgeable assistant, offering data-driven insights that help build a more confident diagnosis.
Think about the challenge of grading tumors, where tiny, subtle differences in cell structure can completely change a patient's treatment path. An AI tool can provide objective measurements and instantly compare the case against a massive database of similar examples, essentially offering a data-backed second opinion on demand.
This partnership between human and machine works like this:
- AI Analysis: The algorithm scans the slide, maps out tumor regions, and measures key biomarkers.
- Pathologist Review: The pathologist looks at the AI's output, which is usually shown as a visual "heat map" or overlay on the digital slide.
- Informed Decision: The pathologist then combines the AI's hard data with their own clinical knowledge and the patient's context to make the final call.
This human-AI collaboration is where the magic really happens. The AI provides the objective numbers, but the pathologist provides the crucial context, ensuring the diagnosis isn't just technically accurate but clinically meaningful. It’s this teamwork that pushes the standard of care forward, leading to more precise and personalized treatments for patients.
Improving Diagnostic Accuracy with AI Insights
In pathology, getting the diagnosis right is everything. It's the foundation of every treatment plan, and a small misinterpretation can change a patient's entire journey. This is where artificial intelligence in pathology shows its true strength, moving beyond simple efficiency to become a vital partner in precision, especially in the nuanced world of oncology.
One of the field's oldest challenges is inter-observer variability. It's the simple fact that two highly skilled pathologists can look at the same complex slide and come away with slightly different interpretations. It's not about skill, but human nature. AI helps solve this by introducing an objective, data-rich perspective that acts as a consistent reference point for everyone.
Reducing Variability and Boosting Confidence
AI algorithms don't just "look" at tissue samples; they analyze them with mathematical rigor. They count cells, measure tumor margins, and quantify biomarker expression with a level of precision that's simply not possible for the human eye. This data-first approach takes the guesswork out of critical diagnostic steps.
Take tumor grading, for example. What often involves a visual estimate of cell percentages becomes a hard number with AI. The algorithm can provide an exact count across the entire slide, giving the pathologist a solid, repeatable figure to anchor their assessment. This means a diagnosis is just as consistent on a Friday afternoon as it is on a Monday morning.
Think of AI as an impartial second opinion that has studied millions of reference images. It doesn't replace the pathologist's expertise—it fortifies it with objective evidence, building diagnostic confidence and creating a new standard of consistency.
The end game here is to make every diagnostic decision a data-driven one. If you're interested in the broader impact of this shift across industries, you can explore the benefits of data-driven decision-making. For pathology, it means every diagnosis is supported by robust, quantifiable proof.
A Deeper Look at Cancer Subtype Classification
AI’s impact becomes crystal clear when you get into the weeds of classifying cancer subtypes. Many cancers, like breast cancer, have specific variations that demand different treatments. Nailing the subtype is the key to personalized medicine, but the visual clues on a slide can be incredibly subtle.
This is where trained AI models shine. Fed with massive datasets of annotated images, they learn to spot these faint patterns with incredible accuracy, which directly boosts agreement among pathologists.
A recent study involving six top academic centers really drives this point home. When pathologists used AI to help score challenging HER2 breast cancer cases, the results were striking.
Impact of AI on Diagnostic Agreement in HER2 Scoring
This table showcases the percentage point improvement in diagnostic agreement among pathologists when using AI assistance for challenging HER2 breast cancer classifications, based on recent studies.
| HER2 Status | Agreement Without AI | Agreement With AI | Improvement |
|---|---|---|---|
| HER2-low | 73.5% | 86.4% | +12.9 points |
| HER2-ultralow | 65.6% | 80.6% | +15.0 points |
These numbers are more than just statistics; they represent a significant leap in consistency for some of the toughest cases. Critically, this AI-assisted workflow also slashed the misclassification of HER2-null cases by about 65%. This means more patients are correctly identified for the targeted therapies that could save their lives.
This infographic paints a clear picture of AI's benefits on key lab performance metrics.
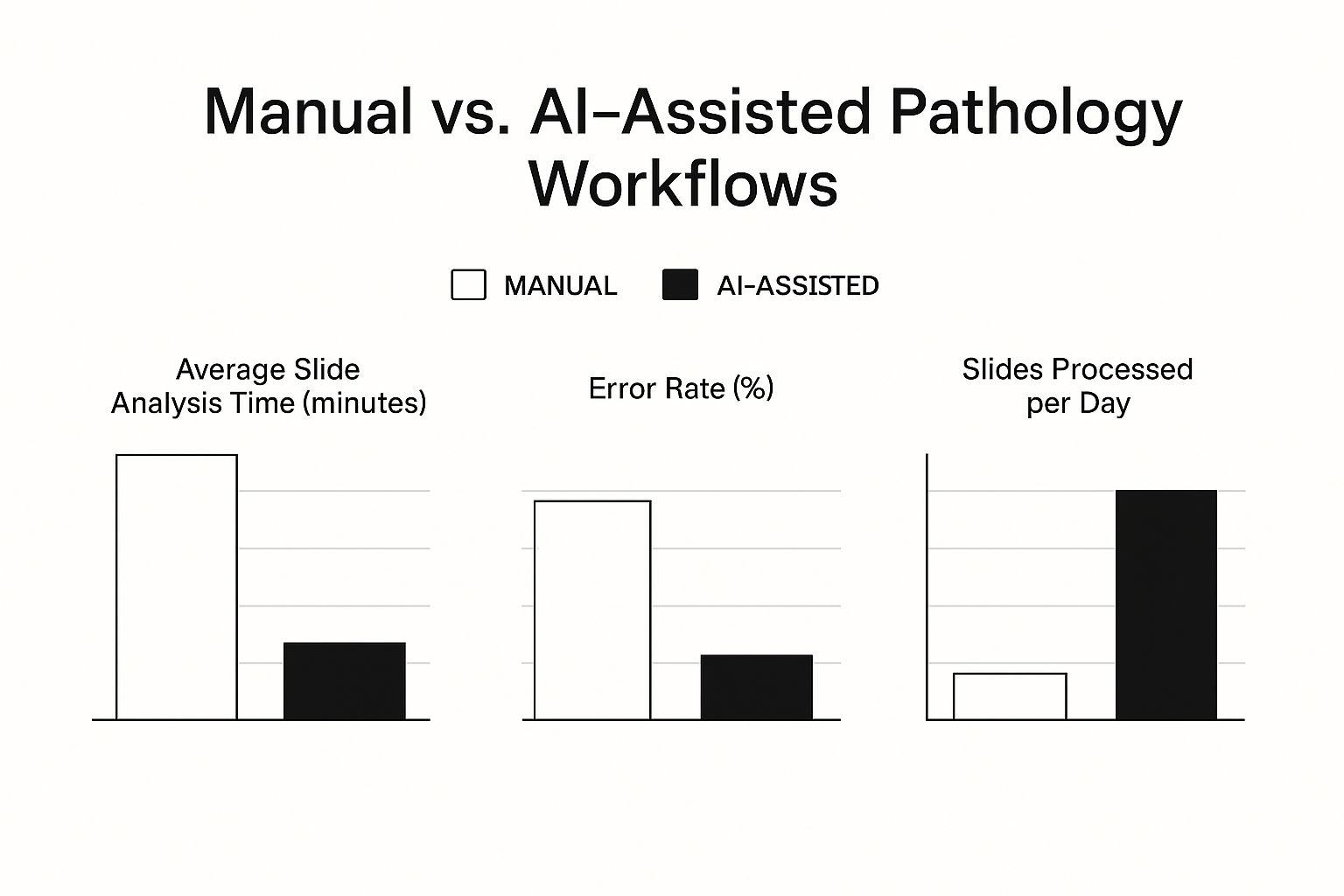
The data speaks for itself. Integrating AI doesn't just lower error rates; it also boosts daily throughput and cuts down on the time spent analyzing each slide. By adding this layer of precision, AI acts as a powerful safeguard, helping pathologists deliver the most accurate diagnosis possible. It’s this blend of human expertise and machine precision that is raising the standard of care for every single patient.
Solving Modern Laboratory Challenges with AI
Pathology labs today are in a tough spot. They're being squeezed from all sides. On one hand, diagnostic demand is skyrocketing, thanks to an aging population and the growing complexity of cancer testing. On the other, they’re grappling with a chronic shortage of pathologists and budgets that seem to get tighter every year. It’s a classic case of being asked to do more with less.
This is where artificial intelligence in pathology stops being a futuristic concept and becomes a practical, strategic tool for survival. AI-powered automation directly tackles these pressures by making labs more efficient, speeding up diagnosis times, and helping a stretched workforce manage their caseloads more effectively.

Alleviating Workforce Strain and Preventing Burnout
It's no secret that there’s a global shortage of pathologists. This isn't just a statistic; it translates into real-world strain and burnout as skilled experts work tirelessly to keep up. AI steps in to help carry the load by taking over the most repetitive, mind-numbing parts of the job.
Think about it. A pathologist might spend hours manually counting thousands of cells to grade a tumor or meticulously scanning an entire slide just to find a handful of abnormal cells. These are perfect jobs for an algorithm that can perform them almost instantly and without getting tired.
- Automated Pre-Screening: AI can do a first pass on slides, quickly identifying normal cases that need minimal review and flagging the potentially problematic ones for immediate attention.
- Quantitative Analysis: It can instantly provide precise data for tasks like biomarker quantification, replacing subjective guesswork with hard, objective numbers.
- Reduced Manual Effort: All this automation frees up a massive chunk of a pathologist's day, giving them more time to focus on tricky diagnoses, consult with colleagues, and collaborate with oncologists.
By taking on this grunt work, AI gets right to the heart of what causes burnout. It lets highly trained professionals use their expertise on the complex cases where human judgment is irreplaceable.
Enhancing Operational Efficiency and Scalability
Beyond lightening the load for individual pathologists, AI can reshape how a lab operates. It allows labs to handle a growing number of cases without necessarily needing to hire more people—a massive advantage when budgets are a constant concern.
AI acts as a "force multiplier," allowing a single pathologist to manage a larger caseload with greater confidence and less stress. This investment in technology is an investment in the long-term viability of the lab itself.
This isn’t just a nice-to-have; it's becoming a necessity. In a recent global survey of 360 senior lab leaders, 38% said workforce shortages were their single biggest challenge. Meanwhile, 31% pointed to declining reimbursement rates as their top financial pressure. You can read more about the forces driving AI adoption in the full survey results.
Ultimately, bringing AI into the lab is a forward-thinking move. It's about preparing for the future—a future with even more tests and greater diagnostic complexity. By building smarter, more efficient workflows, AI helps ensure labs can continue providing the accurate, timely diagnoses that are so critical for patient care, no matter what pressures come their way.
Navigating the Hurdles of AI Implementation
Bringing artificial intelligence into a pathology lab is a major project. It’s less like flipping a switch and more like planning a complex expedition. While the potential payoff is huge, getting there means tackling a few significant challenges head-on. Labs have to navigate technical upgrades, find the budget, and—most importantly—manage the human side of the equation to make sure these powerful new tools actually work as promised.

This screenshot from the FDA's website shows just how many AI-enabled medical devices are now on the market, which also highlights the growing regulatory landscape. A key part of a successful rollout is choosing tools that have already passed these tough validation and approval processes, ensuring they are safe and effective for clinical use.
Overcoming Technical and Financial Barriers
Right out of the gate, the biggest hurdles are usually technical and financial. AI algorithms need pristine digital slides to do their job, which means the first step for many labs is the complete switch to digital pathology. That’s a serious upfront investment.
Labs need to budget for several big-ticket items:
- High-Throughput Scanners: These are essential for turning physical glass slides into high-resolution whole-slide images.
- IT Infrastructure: We're talking about massive data storage systems and serious processing power. The file sizes for digital images are enormous, and the infrastructure has to be able to handle them.
- Software Integration: The AI platform can't be an island. It has to talk to the existing Laboratory Information System (LIS) smoothly to prevent clumsy workflows or data getting stuck in silos.
These initial costs can be a tough pill to swallow. It takes a solid business case and careful planning to get the funding approved, weighing the long-term gains in efficiency and accuracy against the initial cash outlay.
Managing the Human Side of Change
But the technology is only half the battle. The human element—getting your team trained, adjusting workflows, and building trust in the new system—is just as critical. Pathologists and lab staff have spent years perfecting their methods, so it's natural for them to be a little skeptical of a brand-new technology.
A smooth transition is about much more than showing people how to use new software. It's about a cultural shift, helping the team see AI as a partner, not a replacement.
The real magic happens when AI and pathologists work together. It’s about creating a true human-AI synergy where the tech crunches the numbers and handles the repetitive tasks, freeing up the experts to focus on nuanced interpretation and the bigger clinical picture.
Good training needs to cover a few key areas:
- Understanding the "Why": People need to see how AI will make their jobs easier and improve patient care.
- Building Trust: Pathologists have to understand what the algorithms do well and where their limits are. They need to feel confident in the results.
- Workflow Adaptation: AI changes the game, from how cases are prioritized to how they're reviewed. This means old routines will need to be adjusted.
Choosing the Right Tools and Avoiding Fatigue
Finally, you have to be smart about the tools you choose. Not all AI is created equal. It's crucial to pick algorithms that are clinically validated and have regulatory approval. Using an unproven tool is risky; it could introduce errors and undermine the very diagnostic confidence you’re trying to build.
There’s another subtle but major challenge here: clinician alert fatigue. If an AI system bombards pathologists with too many false positives or unimportant flags, they'll eventually start tuning it out. The whole point is lost. The goal is to find a tool that offers genuinely helpful insights without adding to the noise.
Even though AI has been around for over five years, its day-to-day use is still a work in progress. One healthcare survey found that only about 19% of medical organizations felt they had high success with AI-assisted diagnosis. This shows there's a real gap between what an algorithm can do and its practical impact. To get the full value from AI, we have to get serious about fixing these integration and alert fatigue issues, a topic explored further in the Journal of Clinical and Translational Pathology.
The Future Landscape of Pathology with AI
Bringing artificial intelligence into pathology is about so much more than just upgrading lab equipment. It’s a fundamental shift in how diagnostic medicine will work. The lab of tomorrow won't just have new tools; it will have AI as an indispensable member of the diagnostic team, creating a seamless partnership between human experts and machine intelligence. This shift takes us beyond just detecting disease—it opens the door to predicting it, kicking off a new era of proactive and personalized patient care.
The vision is for a powerful human-AI collaboration. Imagine AI handling the tireless, quantitative work—counting mitotic figures, measuring biomarkers, and spotting faint patterns across thousands of slides. This frees up pathologists to do what they do best: operate at the peak of their clinical and intellectual abilities. They can spend their time piecing together complex diagnostic puzzles, consulting with oncologists, and pushing the boundaries of medical innovation.
The Rise of Predictive Biomarkers
One of the most exciting frontiers is the development of predictive biomarkers. AI is learning to see subtle patterns in tissue morphology that are completely invisible to the human eye but contain crucial clues about a disease's trajectory. By analyzing a tumor's intricate architecture, these algorithms can help answer vital questions before a single treatment decision is made.
- Forecasting Disease Progression: An algorithm could predict how aggressively a tumor might behave, helping clinicians decide how aggressive the treatment needs to be.
- Predicting Therapy Response: AI can identify patients who are most likely to respond to specific drugs, like immunotherapy, based on unique tissue features.
- Identifying Resistance Patterns: Early signs of treatment resistance could be flagged by an AI, giving doctors a critical heads-up to change a patient's care plan.
This is a massive leap from reactive diagnosis to proactive forecasting. To really get a feel for how these future tools will work, it helps to understand the underlying tech. For a deeper look, you can explore how various networks power the next generation of AI agents and see how these complex systems come to life.
A New Standard of Personalized Medicine
When you boil it all down, the future of AI in the pathology lab is about delivering on the promise of truly personalized medicine. By combining AI-driven tissue analysis with genomic data and a patient’s clinical history, we can build a far richer, more detailed picture of an individual's disease. This holistic view enables smarter, more targeted treatment decisions right from the start.
The future is not a pathologist versus a machine. It's a pathologist empowered by a machine, working together to deliver a standard of care that is more precise, proactive, and effective than ever before.
This powerful partnership points to a future where diagnoses aren't just faster and more accurate, but far more insightful. By looking deeper into the biology of a disease, this human-AI synergy will pave the way for treatments uniquely tailored to the individual, improving outcomes and offering new hope. The journey is really just beginning.
Answering Your Questions About AI in Pathology
As AI becomes more common in pathology, it’s only natural that questions and concerns pop up. Pathologists, lab managers, and other healthcare pros are all wondering what this technology really means for them. Here, we'll tackle some of the most common questions head-on, giving you straight answers about AI's role, its challenges, and how we can trust its results.
Will AI Replace Pathologists?
Let's clear this one up right away: the consensus among experts is a firm no. AI is not here to replace pathologists, but to work alongside them.
Think of it this way: AI is like an incredibly powerful and tireless assistant. It can do the tedious, repetitive work—like counting thousands of mitotic figures or flagging every single suspicious cell on a gigapixel slide—with a speed and consistency that's simply beyond human capability.
But what AI can't do is think critically. It doesn't understand the nuances of a patient's clinical history or have the seasoned judgment that comes from years of experience. The real magic happens when you combine the two.
The future of pathology is a partnership. AI handles the heavy lifting of quantitative analysis, freeing up pathologists to focus on what they do best: interpreting complex cases, collaborating with oncologists, and advancing research.
What Are the Biggest Barriers to Adopting AI in a Pathology Lab?
Bringing AI into a lab isn't as simple as installing new software. It’s a major shift that comes with a few significant hurdles that need to be planned for carefully. The main roadblocks are usually a combination of money, logistics, and people.
- The Financials: Let's be honest, the upfront cost can be steep. You're looking at digital slide scanners, massive IT storage solutions, and the AI software licenses themselves. Building a solid business case is essential.
- The Technical Integration: Getting a new AI platform to talk to your existing Laboratory Information System (LIS) and other digital pathology tools can be a real headache. It’s a complex technical puzzle that requires specialized IT skills to get right.
- The Human Factor: This is often the most underestimated challenge. It’s not just about training people how to use a new tool. It’s about building trust in the AI's outputs and fundamentally changing workflows that may have been in place for decades. That requires great leadership and a real commitment to managing the change.
Successfully navigating these barriers requires a well-thought-out, step-by-step plan that has buy-in from everyone, from the lab techs on the ground to the C-suite.
How Is the Accuracy of AI Pathology Tools Validated?
Before any AI tool can be used to help diagnose a patient, it has to go through an incredibly strict validation process to prove it's safe, accurate, and reliable. This is far more than a simple software test; it’s a multi-stage gauntlet, often overseen by regulatory bodies.
It starts with training. The AI model learns from a huge, diverse dataset of digital slides that have been carefully annotated by expert pathologists. These slides often come from many different hospitals to make sure the AI can handle variations in staining, tissue preparation, and patient populations.
Next, it’s test time. The model's performance is measured against a completely new set of cases it has never seen before—the "validation" dataset. Its findings are compared to a "ground truth," which is usually the consensus diagnosis from a panel of experienced pathologists.
Finally, for an AI tool to be used in a clinical setting in the U.S. or Europe, it needs the green light from regulators. This means submitting mountains of performance data to organizations like the FDA or earning a CE-IVD mark. This final step is non-negotiable and ensures that any artificial intelligence in pathology touching patient care meets the absolute highest standards.
At PYCAD, we specialize in bringing the power of AI to medical imaging. Our team provides end-to-end services, from data annotation to deploying robust AI models, helping medical device companies and healthcare innovators enhance diagnostic accuracy and efficiency. Discover how our expertise can accelerate your project by visiting https://pycad.co.