Imagine a CT scanner is taking pictures of a loaf of bread without actually cutting it. CT slice thickness is simply the width of each of those individual pictures. It's a fundamental setting that technologists choose for every scan, and it directly shapes how much detail we can see in the final images.
Why CT Slice Thickness Matters in Diagnostics
That single parameter—slice thickness—is one of the most critical decisions in computed tomography. It forces a delicate balancing act that radiologists and technologists navigate for every single patient.
Choosing the right slice thickness is all about weighing two competing factors:
- Image Detail (Spatial Resolution): Thinner slices give us a much more detailed, high-resolution view of the body. This is absolutely essential when we're hunting for tiny problems, like small lung nodules or hairline fractures that would be invisible on a thicker slice.
- Image Noise and Radiation Dose: On the other hand, thicker slices capture more X-ray photons per slice. This results in a "cleaner" image with less random graininess, which we call noise. Thinner slices naturally capture fewer photons, which can make the image look noisy. To get a clear picture with thin slices, we sometimes have to increase the radiation dose.
To get a quick sense of these trade-offs, here’s a simple breakdown.
Quick Overview of CT Slice Thickness Trade-Offs
| Parameter | Thinner Slices (e.g., <1 mm) | Thicker Slices (e.g., >3 mm) |
|---|---|---|
| Spatial Resolution | Excellent (can see small structures) | Lower (may miss fine details) |
| Image Noise | Higher (appears grainier) | Lower (appears smoother) |
| Partial Volume Averaging | Minimized (less blurring of small objects) | Increased (small objects may be obscured) |
| 3D/MPR Quality | High-quality, detailed reconstructions | Lower quality, "blocky" reconstructions |
| Radiation Dose | Often requires a higher dose to reduce noise | Allows for a lower dose for similar noise levels |
| Scan Time | Can be longer due to more data | Faster acquisition |
As you can see, the choice isn't just about getting the prettiest picture; it’s about answering a specific clinical question effectively and safely.
The Evolution to Thinner Slices
This constant balancing act has driven much of the innovation in CT technology. The earliest scanners back in the 1970s were stuck with slice thicknesses greater than 10 mm, which seems incredibly clunky by today's standards and really limited what doctors could diagnose.
The game changed completely with the arrival of multi-slice CT (MSCT) in the late 1990s. This was a huge leap forward, giving us the power to acquire slices of 1 mm or even less. This innovation finally made it possible to create isotropic voxels—essentially, perfect 3D pixels shaped like cubes. These are the building blocks for the incredibly precise 3D reconstructions we rely on today. You can get a deeper look into the history of these CT advancements to see just how far the technology has come.
At its heart, the challenge in CT imaging is always to pick a slice thickness that delivers enough detail for a confident diagnosis while staying true to the ALARA (As Low As Reasonably Achievable) principle for radiation safety.
The image below gives a great visual of how slice thickness is tailored to the specific part of the body being examined.
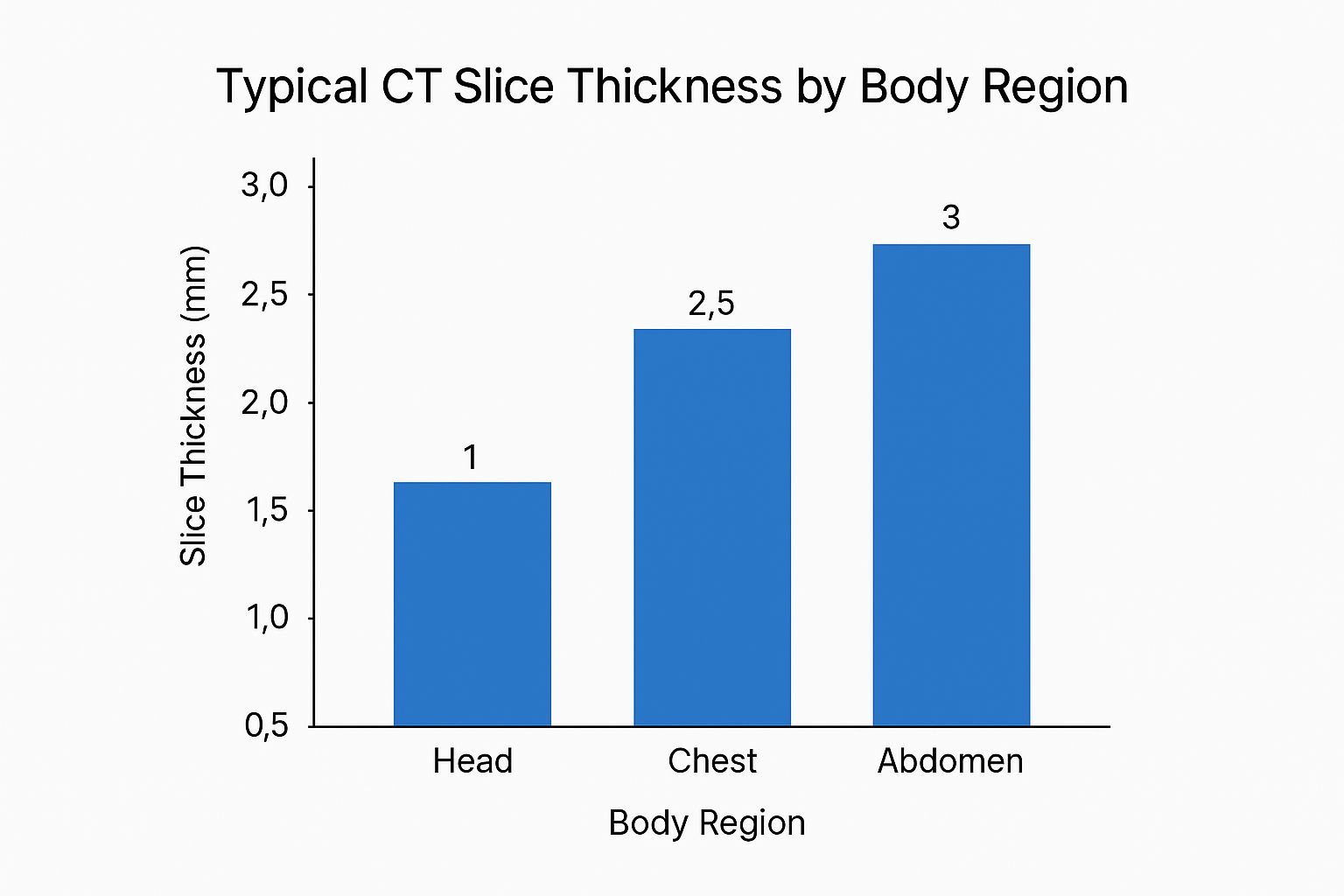
As the chart shows, a scan looking for fine detail in the head will use much thinner slices than a routine scan of the abdomen. This kind of customization is what allows us to optimize every single exam, making sure we get the best possible diagnostic answers for each patient's unique situation.
How a CT Scanner Actually Creates a Slice

To really get a feel for how CT slice thickness affects your images, it helps to peek under the hood and see how the scanner physically carves out these digital slices. It’s a clever dance between mechanical parts and advanced electronics, all designed to precisely shape and capture the X-ray beam.
The key players here are the collimators. The best analogy is the aperture on a camera lens—you can open it wide to let in lots of light or shrink it to a pinpoint for sharp focus. A CT scanner’s collimators do the exact same thing, but for X-rays.
These are essentially a set of lead shutters sitting next to the X-ray tube. By mechanically adjusting how far apart they are, the technologist shapes the X-ray fan beam into a razor-thin ribbon before it passes through the patient. This is the first and most fundamental step in deciding how thick a slice will be.
Collimators and Detectors: A Team Effort
The width of that X-ray ribbon, set by the pre-patient collimators, dictates what we call the nominal slice thickness. A tighter, narrower beam creates a thinner slice. This captures less anatomy in that slice but gives you much finer detail along the length of the patient (the Z-axis).
After the beam passes through the patient, it hits the detector array on the other side of the gantry. In any modern scanner, this isn't just one big sensor. It's a grid made up of thousands of tiny, individual detector elements arranged in neat rows. The final slice thickness you get is a result of both the collimated beam width and how the scanner groups these detector rows together.
Getting slice thickness right has been a long journey. Before the late 1990s, single-detector scanners gave us very few options. Early attempts at CT angiography (CTA), for instance, were stuck with thick slice settings, often over 3 mm, which really smeared out the detail along the Z-axis. Helical scanning in the early 90s was a great step forward, but still held back by those single-row detectors. If you're curious about the early days, there are some great reads on the historical development of CT technology.
From One Slice at a Time to Multi-Detector CT
The game truly changed with the arrival of Multi-Detector CT (MDCT). This innovation swapped out the single row of detectors for multiple, parallel rows, completely changing how we manage slice thickness.
With an MDCT scanner, a single rotation of the gantry could now grab the data for many slices at once. This opened up a world of possibilities:
- Ultra-Thin Acquisitions: Suddenly, we could acquire slices as thin as 0.5 mm or 0.625 mm, capturing incredible detail.
- Warp-Speed Scans: We could now scan entire organs in just a few seconds, dramatically reducing motion blur from a patient's breathing or heartbeat.
- Unbelievable Flexibility: Technologists could scan with super-thin slices and then, back at the workstation, electronically "stack" them to create thicker slices for review. We’ll dig into that a bit later.
This leap to MDCT wasn't just a minor upgrade. It was a fundamental redesign that unlocked the high-resolution, three-dimensional imaging we depend on today.
The Magic of Isotropic Voxels
The ability of MDCT scanners to acquire these paper-thin slices led us to one of the most powerful concepts in modern imaging: isotropic voxels. Think of a "voxel" as a 3D pixel—it's the tiny cube of data that is the basic building block of a CT image.
Imagine you're building a model with LEGOs. If you only use the standard rectangular bricks, your model will look stretched and blocky from the side. But if you have perfectly cube-shaped bricks, you can build smooth, detailed structures that look right from any angle.
Isotropic voxels are those perfect cubes. This happens when the slice thickness is equal to the size of the pixels in the image (the X and Y dimensions). Why does this matter so much? Because it means the data can be reformatted without any distortion. Radiologists can create beautiful multiplanar reconstructions (MPRs), slicing through the anatomy coronally, sagittally, or at any oblique angle with the same crisp clarity as the original axial images. This is absolutely essential for things like surgical planning, mapping out blood vessels, and diagnosing complex conditions.
Balancing Image Quality With Radiation Dose
In the world of CT imaging, every technical choice has a consequence. Perhaps the most critical decision of all is the constant negotiation between getting a crystal-clear picture and keeping the patient safe. The CT slice thickness you select is right at the heart of this trade-off. It’s a balancing act governed by one of the most fundamental principles in medical imaging: ALARA, or "As Low As Reasonably Achievable."
The ALARA principle is our guiding star. It insists that we use the absolute minimum radiation dose necessary to produce an image that is diagnostically useful. Go too low, and the image becomes a blurry mess, potentially forcing a repeat scan and doubling the dose. Go too high, and you expose the patient to unnecessary risk. Slice thickness is one of the main dials we turn to find that perfect balance.
Thinner Slices and the Quest for Detail
So, why would you opt for a thinner slice? The simple answer is to crank up the spatial resolution. This is our ability to see two tiny, separate objects as distinct instead of one blurry blob. When your slices are thin, even minuscule anatomical structures can be precisely defined and measured.
One of the biggest wins here is minimizing an artifact we call the partial volume effect. Picture a tiny pea sitting on a countertop. If you try to capture its shape by pressing a thick slice of bread down on it, the pea just gets mashed into the bread. It becomes part of the bread's overall texture, nearly impossible to spot.
That's precisely what happens in a CT scan. A small lung nodule or a tiny kidney stone can get averaged into the surrounding tissue if it's caught within a thick slice, effectively rendering it invisible.
The partial volume effect is a major diagnostic hurdle. By using a thinner CT slice thickness, we ensure small but critical pathologies aren't blurred into obscurity, giving them a much higher chance of being detected.
By "slicing" the anatomy more finely, we isolate these small structures. This gives them sharp, well-defined edges that make them pop. It’s why exams demanding exquisite detail, like high-resolution chest CTs or complex vascular studies, rely on sub-millimeter slices.
The Inescapable Problem of Image Noise
Of course, this hunt for detail isn't free. Thinner slices mean smaller volumes, and smaller volumes mean fewer X-ray photons are captured by the detector for that slice. This photon starvation is what introduces image noise—that grainy, mottled look you can see on an image.
It’s a lot like taking a picture in a dark room. If you use a super-fast shutter speed (analogous to a thin slice with a low dose), your photo will be grainy because the camera's sensor didn't collect enough light. To get a clean shot, you’d need to leave the shutter open longer or use a bright flash, both of which are like increasing the radiation dose in a CT scan.
To fight the noise that comes with a thin slice and still get a usable image, technologists often have to increase the radiation output. They typically do this by bumping up the tube current-time product (mAs). This pushes more photons through the patient, improving the signal-to-noise ratio (SNR) but, as a direct result, increasing the patient's radiation dose.
Finding the Diagnostic Sweet Spot
This is where the real art and science of CT scanning come together. The goal isn't just to create the "prettiest" picture possible. The goal is to get an image that answers the clinical question with confidence while staying true to the ALARA principle. It all comes down to a careful, case-by-case evaluation.
- High-Detail Scans: For a patient with suspected interstitial lung disease, the need to see microscopic changes in the lung tissue absolutely justifies using thin slices (around 1 mm) and, consequently, a potentially higher dose.
- Routine Follow-Ups: On the other hand, a routine follow-up scan for a known, large abdominal mass probably doesn't need that level of detail. In this case, using thicker slices (in the 3-5 mm range) would give the radiologist all the information they need while dramatically lowering the patient’s radiation exposure.
Ultimately, choosing a CT slice thickness is a clinical judgment call. It requires weighing the diagnostic value of high resolution against the inherent risk of radiation, ensuring every single scan is optimized for both diagnostic accuracy and patient safety.
Choosing the Right Slice Thickness for Clinical Cases
Theory gives us the foundation, but clinical practice is where the real art and science of CT imaging come alive. Picking the right CT slice thickness isn't a one-size-fits-all decision; it’s a specific choice driven by the diagnostic question we need to answer. Every part of the body and every potential disease has its own requirements for detail, demanding a unique approach.
Think of it like choosing the right tool for a job. You wouldn't use a sledgehammer for delicate woodwork, and you wouldn't use a tiny engraving tool to break up concrete. In the same way, the slice thickness has to match the scale of the anatomy you're looking at to get a confident diagnosis.
High Resolution for Fine Details
Some clinical situations absolutely demand the highest spatial resolution possible, making sub-millimeter slices a must. These are the cases where the targets are incredibly small, and any blurring from a thicker slice could completely hide what you're looking for.
-
Cardiac CT Angiography (CTA): To see the tiny coronary arteries—often just a few millimeters wide—you need exceptionally thin slices, typically around 0.625 mm. This level of detail is critical for spotting stenosis (narrowing) or plaque that could lead to a heart attack.
-
Interstitial Lung Disease (ILD): When we’re looking for conditions like pulmonary fibrosis, we have to see the delicate, web-like structures inside the lung tissue. Thin slices, often 1.0 mm to 1.25 mm, are essential to pick up subtle patterns of scarring and inflammation that would be completely invisible on routine chest scans.
-
Fine Musculoskeletal Fractures: Finding subtle hairline fractures, especially in complex joints like the wrist or ankle, depends on thin-slice imaging. Slices of 0.625 mm to 1.5 mm allow us to create high-quality multiplanar reformats, which let surgeons see the fracture lines from any angle.
In these situations, the need for maximum detail is more important than the potential for more image noise or a higher radiation dose. The diagnostic information we get from seeing these tiny structures clearly is simply too important for patient care to compromise on.
Broader Views for General Assessments
On the other hand, not every scan needs microscopic detail. For routine scans of larger body areas, using thicker slices is often a smarter, safer, and more efficient way to go. It follows the ALARA (As Low As Reasonably Achievable) principle by lowering the patient's dose while still giving us all the information needed for a diagnosis.
For many routine abdominal and pelvic scans, a CT slice thickness of 3 mm to 5 mm provides an excellent balance. It effectively minimizes radiation dose and reduces the sheer volume of data for radiologists to review, all while being perfectly capable of detecting larger pathologies like tumors, abscesses, or organ damage.
This approach also has roots in how CT technology has developed over the years. The very first clinical scanner in 1971 took about five minutes to acquire a single 10 mm slice. Fast forward to today, and a modern 64-slice scanner can image an entire abdomen in under 10 seconds using slices as thin as 0.5 mm—a huge leap in engineering. This push for thinner, faster scans has also spurred on new dose-reduction techniques, helping to balance the massive increase in data with patient safety. You can learn more about the evolution of CT scan speeds and safety in this detailed overview.
A Quick Guide to Common Protocols
To make this more concrete, here's a look at the typical slice thicknesses used for some of the most common scans we perform. These aren't rigid rules but reflect the standard practice that balances image quality with patient safety for specific clinical questions.
| Clinical Application | Typical Slice Thickness | Primary Rationale |
|---|---|---|
| Cardiac CTA (Coronary Arteries) | 0.5 – 0.75 mm | Maximizes spatial resolution to visualize small vessels and stenosis. |
| High-Resolution Chest CT (ILD) | 1.0 – 1.25 mm | Crucial for identifying fine interstitial patterns and early fibrosis. |
| Abdomen/Pelvis (Routine) | 3.0 – 5.0 mm | Balances diagnostic quality for large organs with dose and data reduction. |
| CT Urography (Kidney Stones) | 2.0 – 3.0 mm | Sufficient to detect small calcifications while minimizing radiation dose. |
| Non-Contrast Head CT (Stroke) | 2.5 – 5.0 mm | Allows for rapid detection of acute hemorrhage or large territorial infarcts. |
| Complex Fractures (e.g., Wrist) | 0.625 – 1.5 mm | Enables high-quality 3D and multiplanar reformats for surgical planning. |
This table shows how the choice is always a trade-off. For something tiny like a coronary artery, we need the thinnest slice possible. For a general survey of the abdomen, thicker slices do the job perfectly well and are safer for the patient.
Specialized Protocols for Specific Needs
Beyond these general categories, many protocols are fine-tuned to answer a single, urgent clinical question.
- Stroke Protocols: In a potential stroke, the first step is often a non-contrast head CT to rule out a bleed. We typically use slices around 2.5 mm to 5 mm. This is thick enough to quickly spot significant hemorrhage without the fine detail—and longer reconstruction time—of thinner slices.
- Kidney Stone Scans: A low-dose study for renal colic usually uses slices between 2 mm and 3 mm. This is more than enough to spot even small calcified stones in the urinary tract while keeping radiation exposure to a minimum, which is key for patients who might need repeat scans.
Ultimately, choosing the CT slice thickness is a deliberate act, guided by the anatomy we’re examining, the pathology we suspect, and the unwavering principle of keeping our patients safe.
Fine-Tuning Scans with Modern Tech

The age-old balancing act of picking just one CT slice thickness is quickly becoming a thing of the past. Modern scanners and software have given us sophisticated ways to get the best of both worlds—fine detail and smooth, low-noise images—all from a single scan.
One of the most powerful tools in our arsenal is reconstructed slice thickness. This technique cleverly separates the slice thickness the scanner acquires from the slice thickness the radiologist actually views. The concept is simple but brilliant: scan the patient using the thinnest slices the machine can manage, often well under a millimeter.
This initial dataset is packed with high-resolution information, making it perfect for generating detailed 3D models or multiplanar reformats (MPRs). The only catch is that these ultra-thin slices can look pretty noisy on their own. That's where the software steps in to computationally "stack" the data, creating a second, thicker set of slices—say, 3 mm or 5 mm—that are much smoother and easier on the eyes for routine review.
The Game-Changer: Iterative Reconstruction
Another huge leap forward, which goes hand-in-hand with slice optimization, is iterative reconstruction (IR). For years, our standard reconstruction methods were fast, but they had a nasty habit of amplifying noise, especially when we tried to lower the radiation dose. IR algorithms are a whole lot smarter.
Think of it like restoring an old, grainy photograph. Instead of just accepting the noise, IR repeatedly refines the image. It starts by creating a rough draft, compares it against a sophisticated statistical model of what a "perfect" CT image should look like, figures out what's noise, and subtracts it. This process iterates over and over until you're left with a clean, high-quality image.
The real magic of iterative reconstruction is that it lets us use much thinner slices at a significantly lower radiation dose. It effectively breaks the old rule that thin slices always demanded more radiation to be useful for diagnosis.
This technology is precisely why low-dose CT screening programs, like those for lung cancer, have become so successful. It gives us the confidence to capture the detail we need without compromising patient safety.
AI Is Now Driving Protocol Decisions
The latest frontier in optimizing our scans is the arrival of Artificial Intelligence (AI) and deep learning. AI isn't just for image analysis anymore; it's now helping us tailor the entire scanning process, including how we choose slice thickness.
AI-driven systems can analyze patient data—things like age, weight, and the reason for the scan—to recommend the ideal protocol before the technologist even hits the button. This brings a new level of consistency and helps ensure we’re always following the ALARA principle for every single patient.
Even more impressive are the deep learning reconstruction (DLR) algorithms, which are taking noise reduction to a completely new level. These advanced AI models are trained on mountains of high-quality scan data, allowing them to produce incredibly clear images from extremely low-dose scans that would have been unreadable just a few years ago.
Companies like PYCAD are leading the charge, building AI tools that plug right into our workflows to boost both efficiency and diagnostic accuracy. This intelligent approach helps ensure every scan is perfectly tuned for the best possible result with the lowest possible risk.
Putting It All Together in Your Daily Practice
When you get right down to it, mastering CT imaging is all about one thing: the slice thickness you choose. This single parameter is the fulcrum on which image detail, clarity, and patient safety all balance. It’s not about memorizing physics; it's about confidently applying this knowledge to every single scan to give each patient the best possible outcome.
The core challenge never really changes: how do we get a diagnostically sharp image without exposing the patient to more radiation than necessary?
Thinking in terms of this fundamental trade-off is the key. Thinner slices are fantastic for seeing tiny anatomical details, giving you incredible spatial resolution. But the trade-off is more image noise. On the flip side, thicker slices give you a smoother, less grainy image and let you dial down the radiation dose. The catch? You risk blurring or missing small findings because of partial volume averaging. The "right" choice is always, and only, the one that fits the clinical question at hand.
Key Takeaways for Clinical Confidence
So, how do you translate this into your day-to-day work? Keep these principles in mind:
-
Start with "Why": The clinical question is everything. Are you hunting for minuscule coronary plaques, or are you doing a general survey of the abdomen? Your answer should immediately guide your slice thickness selection.
-
Use Your Tools Wisely: Get comfortable with reconstructed slice thickness. The modern standard is to acquire data with thin slices and then rebuild thicker ones for review. This gives you the best of both worlds: high-resolution source data for multi-planar reformats and smoother, low-noise images for primary interpretation.
-
Embrace New Technology: Iterative reconstruction and AI-powered deep learning aren't just buzzwords anymore; they are powerful clinical tools. They genuinely break the old rules of the dose-noise-resolution trade-off, making it possible to achieve thin-slice, low-dose scans that were unthinkable just a few years ago.
Ultimately, the goal is to make slice thickness a conscious, strategic choice for every scan, not just a default setting on the protocol. By weaving together the concepts of resolution, noise, and dose with the capabilities of modern CT scanners, we can truly optimize every single study.
This mindset shifts slice thickness from being just another technical setting to a powerful lever for improving diagnostic accuracy. It helps you make smarter, safer, and more effective decisions that have a direct, positive impact on patient outcomes. When you master the nuances of slice thickness, you ensure every image you acquire tells the clearest possible story.
Got Questions About CT Slice Thickness? Let's Break It Down.
When you're in the trenches of daily scanning, the technical details can get a little fuzzy. Let's tackle some of the most common questions about CT slice thickness and connect the physics to what you actually do in the control room.
Getting these concepts straight is fundamental to tweaking your protocols for the best possible diagnostic images.
Acquired vs. Reconstructed Slices: What's the Real Difference?
This is probably one of the most common points of confusion, but the distinction is crucial. Even though they sound alike, they refer to two completely different parts of the imaging chain.
Acquired slice thickness is all about the hardware. It's the physical thickness of the data slice your scanner is capturing during the actual scan, defined by the X-ray beam collimators and how the detector rows are set up. The modern approach is to acquire data as thinly as possible, often well below a millimeter.
Reconstructed slice thickness, on the other hand, happens in the software after the scan is done. A technologist takes that raw, super-thin acquired data and tells the computer to digitally "stack" it into thicker slices for the radiologist to review. This gives you the best of both worlds: smooth, low-noise images for general review, with the original thin-slice data ready and waiting for any detailed 3D work or multiplanar reformats.
Is Thinner Always Better? (Spoiler: No)
It's easy to fall into the trap of thinking thinner slices automatically equal a better scan. The reality is far more practical: the "best" slice thickness is whatever answers the clinical question at hand.
The optimal CT slice thickness isn't the thinnest one possible. It's the one that gives a clear diagnostic answer while keeping the radiation dose as low as reasonably achievable (ALARA).
Sure, razor-thin slices are fantastic for their high spatial resolution, letting you see tiny structures like the coronary arteries or faint lung nodules. But that detail comes at a cost. Thinner slices can look grainy due to increased image noise and might even require a higher radiation dose to get a clean-looking image.
For a lot of everyday work, like a general abdomen scan looking for larger masses, thicker slices are actually the better choice. They deliver great contrast, have less noise, and lower the patient's radiation dose. In those cases, thicker isn't just adequate—it's superior.
How Does Patient Size Change the Game?
A patient's size and body habitus have a huge impact on how you should be thinking about slice thickness, especially when it comes to reconstruction. It's simple physics: larger patients absorb more of the X-ray beam, which can dramatically increase the noise in the final image.
To combat this, a common and effective trick is to reconstruct thicker slices for larger patients. This technique essentially averages the signal from several of the thin acquired slices into a single, thicker slice.
Doing this boosts the signal-to-noise ratio, smoothing out that grainy appearance and producing a much clearer, diagnostically useful image. It's a key adjustment for tailoring protocols to fit each person, ensuring you get quality scans no matter the patient's anatomy, and it's often paired with other parameter tweaks for a fully optimized study.
At PYCAD, we build AI-powered tools that help imaging departments refine their workflows and optimize critical parameters like slice thickness. To see how our solutions can bring more accuracy and efficiency to your practice, check us out at https://pycad.co.






