In a busy hospital, the radiology department is the air traffic control tower. Every single scan—from an X-ray to a complex MRI—is a flight that needs to be guided with absolute precision. It starts with scheduling, moves through the imaging process, and lands safely as a diagnostic report in a physician's hands. The two systems orchestrating this entire, intricate ballet are PACS and RIS, the true digital heartbeat of modern medical imaging.
The Digital Heartbeat of Modern Radiology
Can you imagine trying to run a major airport with paper tickets and walkie-talkies? It would be pure chaos. That's exactly what radiology would be without a robust digital backbone. The sheer volume of data generated by modern imaging is staggering, and it demands a sophisticated framework to keep everything moving. This is where Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS) come in. These platforms work together, ensuring every patient's journey is smooth, safe, and efficient.

This guide is designed to pull back the curtain on these systems. We'll skip the dense, technical jargon and get straight to their core purpose and the incredible synergy they create. Understanding how they operate is the first step in seeing just how much they impact patient care and the speed of diagnosis.
Distinguishing the Core Roles
When you look at them from a high level, the division of labor between PACS and RIS is beautifully simple, yet incredibly powerful. Each system has its own clear mission, and when they come together, they create a complete, seamless operational picture.
- RIS as the Command Center: Think of the Radiology Information System as the operational brain. It manages all the logistical and text-based information. This includes everything from scheduling a patient's appointment and tracking their records to handling billing and distributing the final report.
- PACS as the Visual Archive: The Picture Archiving and Communication System is the massive, secure digital library for the images themselves. It’s where every X-ray, CT scan, and MRI is stored, retrieved, and displayed, making them instantly accessible to clinicians wherever they are.
Here’s a simple way to remember it: The RIS knows who the patient is, what procedure they need, and when it’s happening. The PACS holds the visual evidence from that procedure—the actual images that make a diagnosis possible.
A well-integrated PACS and RIS environment does more than just manage data. It creates an intelligent, fluid workflow that slashes errors, speeds up diagnoses, and gets critical information into the right hands, faster.
At PYCAD, we live and breathe this ecosystem. We specialize in building custom web DICOM viewers and integrating them directly into medical imaging platforms, giving clinicians the best possible tools to view and interpret the rich visual data stored in a PACS. Exploring how these systems work together is fundamental for anyone in healthcare technology, a conversation we continue in our look at next-generation radiology. This guide will give you the foundation you need for that deeper dive.
Understanding PACS: The Digital Vault for Medical Images
Think of a Picture Archiving and Communication System (PACS) as the ultimate visual library for a patient's health story. But instead of dusty books, this library holds every X-ray, MRI, CT scan, and ultrasound ever taken, all organized and instantly accessible. It’s a powerful digital ecosystem that moves radiology beyond the clumsy world of physical film into a seamless, data-driven reality.

The days of frantically searching for a misplaced X-ray or waiting hours for a courier to deliver a prior scan from an off-site warehouse are thankfully behind us. With a PACS, a doctor can pull up a patient's entire imaging history—from a bone scan a decade ago to a CT scan from yesterday—with just a few clicks. This immediate access is a game-changer for tracking disease progression and making faster, more confident diagnoses.
The Four Pillars of PACS
To really get what makes a PACS tick, you need to know its four essential components. Each one plays a critical role in the life of a medical image.
- Imaging Modalities: These are the image creators—the CT scanners, MRI machines, and X-ray units that generate the raw visual data.
- A Secure Network: This is the high-speed highway that securely zips massive image files from the imaging machines to the central archive and then out to the doctors who need to see them.
- Viewing Workstations: These are the specialized "reading rooms" where radiologists and specialists do their work. Outfitted with high-resolution monitors and advanced software, these stations are mission-control for diagnosis.
- The Archive Server: This is the heart of the whole operation. It’s a robust, secure server that acts as the digital vault, storing and managing enormous volumes of image data while ensuring it’s always safe and available.
A PACS doesn't just store images; it creates a world of universal, immediate access to visual diagnostic data. It empowers clinicians to collaborate and diagnose from anywhere, at any time.
This digital vault truly comes alive through its viewing software. A basic viewer might just display an image, but a sophisticated one gives clinicians the tools they need for deep, efficient analysis. This is where tailored solutions make all the difference. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, delivering the advanced tools and seamless workflows that modern healthcare demands. You can see examples of our specialized work on our portfolio page.
The incredible potential of this visual vault is being amplified even further by new developments in AI for medical imaging and diagnostics, which are changing the very nature of image analysis.
By centralizing every scan, pacs and ris systems work hand-in-hand to build a complete patient record. The visual data from the PACS is perfectly framed by the administrative context from the RIS. This powerful synergy breaks down data silos, cuts down on diagnostic errors, and ultimately raises the standard of care by making sure every decision is informed by the full clinical picture.
Decoding RIS: The Workflow Command Center
If a PACS is the high-tech, secure vault for medical images, then the Radiology Information System (RIS) is the bustling control room that runs the entire operation. It’s the logistical mastermind, the air traffic controller for the radiology department. The RIS doesn't care about the pixels in an MRI; it cares about the who, what, when, where, and why behind every single scan.
Think of it as the central nervous system of the patient's imaging journey. From the moment an exam is requested, the RIS springs to life, orchestrating every step with incredible precision.
Orchestrating the Patient Journey
Let's walk through a typical patient visit to see the RIS in its element. This is where you can truly appreciate how pacs and ris systems combine to create a seamless experience, moving from abstract concepts to real-world impact.
It starts with a simple digital request from a doctor. That order lands in the RIS, triggering a cascade of perfectly coordinated events.
-
Scheduling and Registration: First, the RIS consults the intricate schedule of every scanner and radiologist. It finds an open slot, books the appointment, and prevents any conflicts. When the patient arrives, the RIS handles the registration, capturing demographics and insurance details, building a complete digital record that follows them.
-
Real-Time Patient Tracking: The moment a patient checks in, they're on the RIS's radar. The system tracks their journey in real-time—from the waiting room, to the changing area, into the CT scanner, and out to recovery. This level of visibility is a game-changer for managing patient flow and keeping wait times down.
Mastering these logistics is where a radiology department can unlock huge efficiencies. If you're looking to dive deeper, we've covered many more strategies in our guide to radiology workflow optimization.
From Scan to Final Invoice
After the technologist captures the images and sends them to the PACS, the RIS's job is far from over. It now shifts to managing the crucial diagnostic and administrative tasks that follow.
The RIS is the single source of truth for the entire administrative and diagnostic workflow. It ensures that every action, from scheduling to billing, is connected, tracked, and flawlessly executed.
The radiologist now sees the new study appear on their worklist, which has been intelligently prepared and prioritized by the RIS. They analyze the images and create their diagnostic report, a process the RIS makes remarkably efficient.
Here’s how the RIS brings it all home:
- Report Generation and Distribution: The system often integrates with voice recognition software, letting radiologists dictate their findings directly. Once the report is finalized and signed, the RIS takes over, automatically sending it to the referring physician through secure, compliant channels.
- Billing and Financials: With the exam and report finalized, the RIS has all the information it needs. It captures the correct billing codes and generates the data for an accurate invoice, dramatically cutting down on manual errors and accelerating the payment cycle.
This end-to-end management ensures no detail is missed. The RIS is the backbone that enables the clinical excellence of the PACS to truly shine. At PYCAD, this synergy is at the heart of what we do. We design and build custom web DICOM viewers and embed them into medical imaging platforms, making sure the powerful images from a PACS are supported by the workflow intelligence of a world-class RIS. You can see our work in action on our portfolio page.
How PACS and RIS Systems Bring Radiology to Life
The real magic in modern radiology happens when PACS and RIS stop being two separate systems and start talking to each other. When they work in concert, they create a single, seamless ecosystem that guides the entire patient experience, from scheduling to diagnosis.
Think of it like a world-class orchestra preparing for a performance.
The RIS is the conductor. It holds the master plan—the sheet music—and coordinates every musician. It schedules rehearsals and ensures the entire performance flows from one movement to the next without a single missed note. It’s all about the logistics, the schedule, and the story of the patient's visit.
The PACS, in this analogy, is the orchestra itself. It produces the rich, detailed, and powerful music—the medical images that form the very heart of the diagnostic process. Without the orchestra, the conductor has nothing to lead. But without the conductor, the orchestra's brilliant music would just be noise.
Their synergy is what creates a masterpiece.
Mapping the Integrated Patient Journey
This beautiful harmony between pacs and ris systems isn’t just an abstract idea; it plays out every day in a highly efficient, logical sequence. Let’s walk through a patient's journey to see how this digital symphony performs in a real-world clinic.
It all starts the moment a physician orders a scan. That single click, whether in an Electronic Health Record (EHR) or directly in the RIS, kicks off a perfectly synchronized chain of events.
-
The Order and the Schedule (RIS Takes the Lead): The RIS receives the order, complete with the patient’s information and the specific exam needed. It then gets to work, intelligently scheduling the appointment to avoid conflicts and making sure the right equipment and staff are ready and waiting.
-
The Worklist and the Scan (RIS to PACS): On the day of the exam, the technologist sees the patient on their worklist. Here's where the integration really shines. The RIS sends a DICOM Modality Worklist straight to the imaging machine. This automatically fills in all the patient details, which means no more manual typing and a massive reduction in the risk of human error.
-
The Image and the Update (PACS to RIS): Once the scan is complete, the images are sent directly to the PACS for secure, long-term storage. The PACS then sends a quick message back to the RIS, updating the patient's status to "exam complete." Just like that, everyone in the loop knows the images are ready for the radiologist to review.
This seamless operation is a perfect example of why effective system integration is so crucial. It’s about making separate technologies work together to create a workflow that’s far more powerful than the sum of its parts.
To get a clearer picture of their distinct roles, let's break down their core functions side-by-side.
PACS vs RIS A Functional Comparison
This table highlights how each system contributes its unique strengths to the overall radiology workflow.
| Function | PACS (Picture Archiving & Communication System) | RIS (Radiology Information System) |
|---|---|---|
| Primary Role | Manages, stores, and displays medical images. | Manages patient data and radiology workflow. |
| Core Data | Visual data (DICOM images like X-rays, CTs, MRIs). | Text-based data (patient demographics, scheduling, reports). |
| Key Users | Radiologists, technologists, referring physicians. | Schedulers, administrative staff, billing departments. |
| Main Features | Image viewing tools, secure archiving, distribution. | Patient registration, scheduling, billing, reporting. |
| Workflow Focus | Image acquisition, interpretation, and diagnosis. | Patient management from order entry to final report. |
While PACS handles the "pictures," RIS handles the "paperwork." Together, they ensure the right images get to the right specialist with all the correct patient information attached.
The Common Language of Radiology
For this intricate dance to work, both systems need to speak the same language. This is where universal interoperability standards come in. Without them, the entire process would grind to a halt.
Two main standards make this communication possible:
-
DICOM (Digital Imaging and Communications in Medicine): This is the universal language for all medical images. It's the standard that ensures an MRI taken on one brand of machine can be viewed and stored by software from a completely different company. DICOM is what allows the PACS "orchestra" to be so versatile.
-
HL7/FHIR (Health Level Seven / Fast Healthcare Interoperability Resources): These standards are for the text-based data—the "sheet music"—managed by the RIS. HL7 and its modern successor, FHIR, are the rules for exchanging information like patient demographics, orders, and reports between the RIS, EHR, and other hospital systems.
When you combine DICOM for the visuals and HL7/FHIR for the text, you get a workflow where every part is perfectly in sync. If you want to dive deeper into this topic, our guide on how to achieve seamless PACS integration is a great next step.
The industry has certainly taken notice. Recent analysis shows that integrated solutions accounted for over 62% of the revenue share, proving that the market is moving decisively toward unified platforms that boost efficiency and ensure data flows freely.
This is exactly where we at PYCAD live and breathe. We build custom web DICOM viewers and integrate them into medical imaging web platforms, giving radiologists the absolute best tools to interpret the vital visual data delivered by this powerful workflow.
Putting Your System to Work and Looking to the Future
Bringing pacs and ris systems into your clinical environment is a massive strategic move. The very first fork in the road is deciding where these critical systems will live: on your own servers right down the hall, or in the cloud. Each path presents a different blend of control, cost, and agility, and the best choice is deeply personal to your organization's unique needs and resources.
An on-premise setup gives you direct, hands-on control over every piece of hardware and every byte of data. For organizations with powerhouse IT departments and strict data sovereignty rules, this can be incredibly appealing. But it’s not without its costs—you’re looking at a significant upfront investment in servers and infrastructure, plus the long-term responsibility of maintenance, security, and every single upgrade.
On the other hand, cloud-based systems offer a breathtaking level of flexibility. You can ramp up your storage and computing power on demand, paying only for what you actually use. This approach slashes the initial capital spend and offloads the heavy lifting of hardware management to the cloud provider. The trade-off? You’re trusting a third party with your data’s accessibility and security.
Choosing Your Deployment Model
So, on-premise or cloud? There's no single right answer. It all boils down to a careful look at your organization's priorities. Let’s break it down to help you navigate this decision.
- Security and Control: If absolute, physical control is your top priority, on-premise wins. However, don't underestimate the cloud. Top-tier cloud providers pour millions into cybersecurity measures that often dwarf what a single hospital can realistically manage.
- Scalability and Flexibility: The cloud is the undisputed champion here. Need more storage? It's just a few clicks away. With an on-premise system, expansion means a lengthy and expensive process of buying and installing new hardware.
- Cost Structure: On-premise demands a large upfront capital expenditure (CapEx) plus ongoing operational costs. Cloud models typically run on a subscription basis (OpEx), which makes budgeting more predictable and manageable, especially for smaller practices or clinics.
The workflow diagram below beautifully illustrates the elegant simplicity of how these systems function once they’re up and running—from the moment an order is placed to the final report being delivered.
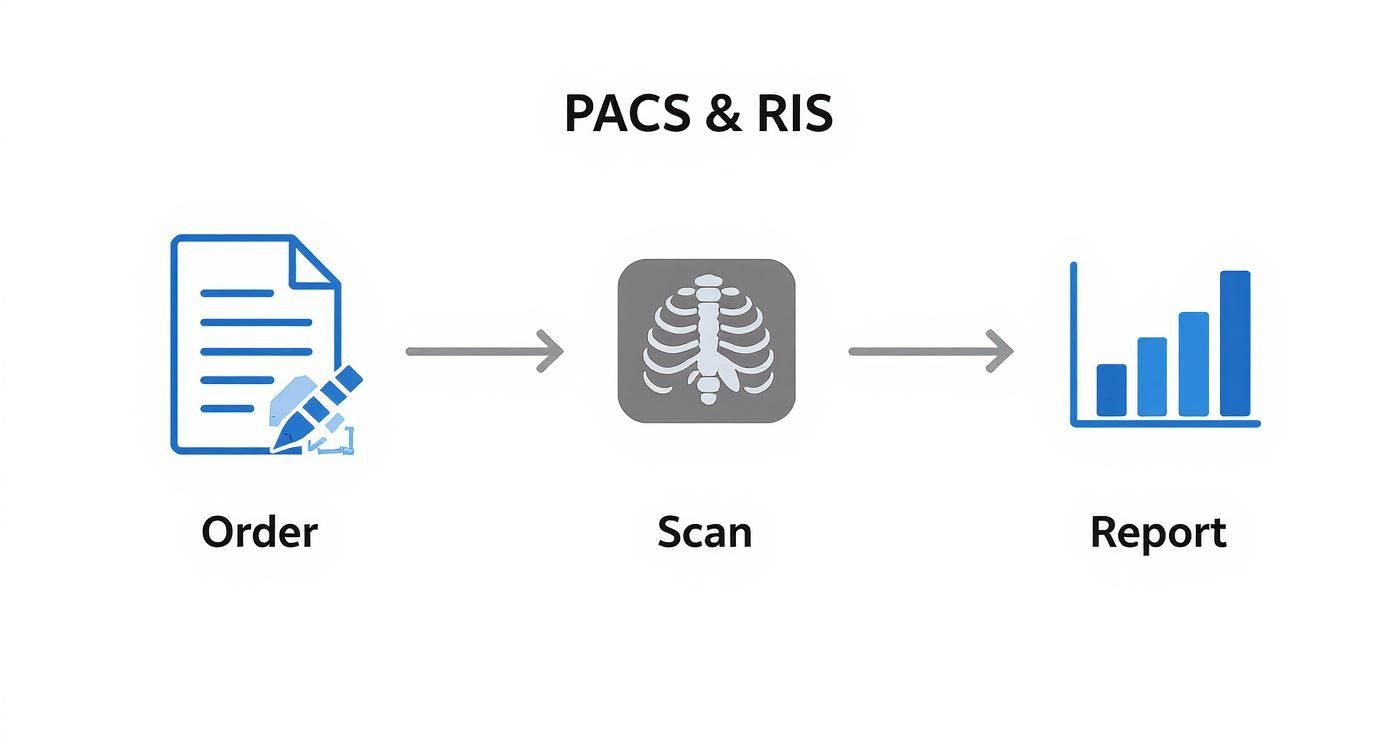
This entire process hinges on that seamless flow of information, a goal that can be achieved whether your data lives in your own server room or in the cloud.
The Future is Intelligent and Interconnected
Looking beyond deployment, the entire landscape of medical imaging is being reshaped by some incredibly powerful forces. These aren't just buzzwords or far-off concepts; they are the new realities defining the next generation of pacs and ris systems.
The relentless march toward digital imaging is fueling this change. The global PACS and RIS market is a testament to this momentum, valued at around USD 5.36 billion and projected to nearly double to USD 10.05 billion by 2035. This isn't just growth; it's a clear signal of the industry's deep commitment to smarter healthcare. You can dive into the numbers and read the full research on the PACS and RIS market to see where things are headed.
The future of radiology isn't just about storing images; it's about making them smarter, more accessible, and completely secure. This means embracing AI, demanding data freedom, and building an unbreakable defense against cyber threats.
Several key trends are paving the way:
- The Rise of Artificial Intelligence (AI): AI is quickly becoming an indispensable partner for radiologists. It can automate tedious tasks, help triage urgent cases by spotting critical findings, and act as a second set of eyes, identifying subtle patterns that might otherwise be missed.
- Vendor Neutral Archives (VNAs): Think of a VNA as a declaration of data independence. It separates your image archive from your PACS viewer, giving you the freedom to switch PACS vendors without the monumental headache of data migration. This puts you, the healthcare provider, firmly back in control of your own data.
- Advanced Cybersecurity: In a connected world, the risk of cyberattacks is very real. The future demands a proactive, multi-layered security strategy, from end-to-end encryption to advanced threat detection, to protect sensitive patient information.
At PYCAD, we’re not just watching this future unfold; we’re actively building it. We specialize in developing custom web DICOM viewers and integrating them into modern medical imaging platforms designed to work hand-in-glove with AI-driven workflows and secure cloud architectures. Take a look at some of the forward-thinking solutions we’ve built on our portfolio page.
Your PACS and RIS Questions, Answered
Diving into medical imaging technology can feel a little overwhelming. With so many terms and systems, it's easy to get lost. Since these platforms are the engine room of any modern radiology department, getting clear on how they work is the first step toward making smart, future-focused decisions. Let's tackle some of the most common questions people have about PACS and RIS systems.
Is a PACS and RIS System Overkill for a Small Clinic?
Not at all. In fact, you could argue that smaller practices feel the positive impact even more dramatically. Think about it: a cloud-based system completely sidesteps the need for a massive, upfront investment in servers and the IT staff needed to maintain them.
For a small clinic, these tools become a force multiplier. You can automate scheduling, simplify the entire billing process, and give consulting specialists instant, secure access to images from anywhere. It’s all about empowering a small team to deliver exceptional care to a large volume of patients without getting bogged down by administrative chaos.
How Is Patient Data Kept Secure?
Security isn't just a feature; it's the absolute foundation of any modern medical system. Both PACS and RIS are engineered from the ground up with multiple layers of defense to meet stringent regulations like HIPAA.
Protecting patient data is non-negotiable. Robust systems use end-to-end encryption, strict access controls, and detailed audit logs to ensure only authorized personnel can view or handle sensitive information.
This layered security model protects data at every stage, whether it's stored on-premise or in the cloud. The goal is to create a digital fortress around patient records and diagnostic images.
What's the Biggest Hurdle During Implementation?
Interestingly, the biggest challenge is rarely the technology itself—it’s the people. While migrating years of patient data from an old system has its complexities, the real make-or-break factor is getting your team trained, comfortable, and genuinely excited about the new workflow.
A smooth transition really comes down to a few key things:
- Great Training: You need to make sure everyone, from the front desk scheduler to the head radiologist, feels confident using the new software.
- Open Communication: Clearly explaining why the change is happening and how it will make everyone's job better is crucial for getting people on board.
- Visible Leadership: Having champions for the project who can guide and support the team through the learning curve makes all the difference.
The investment in getting this right is clearly valued across the industry. North America has long been the leader in the global PACS and RIS market, holding roughly 37% of the market share. The U.S. market alone was valued at nearly USD 590 million and is expected to more than double by 2034. This trend highlights a deep, ongoing commitment to these core technologies. You can discover more insights about the PACS and RIS market to get a clearer picture of the financial landscape.
We at PYCAD build custom web DICOM viewers and integrate them into medical imaging web platforms, giving clinicians the sharpest, most intuitive tools for diagnosis. To see how we're shaping the future of medical imaging, take a look at our work on the PYCAD portfolio page.






