Electronic Health Records (EHRs) are one of the biggest leaps forward healthcare has ever seen. They offer the incredible promise of having a patient’s entire medical history right at your fingertips, but they also bring some serious hurdles to the table—cost, security, and big changes to how clinicians work.
They're not just a new piece of tech; they're the digital backbone of modern medicine. They point to a future where care is safer and more efficient, but getting there requires a clear-eyed look at the whole picture.
The Digital Heartbeat Of Modern Medicine

Think about it: a world where every single piece of a patient's story—lab results, allergies, complex imaging studies, handwritten notes from years ago—is all there, instantly. That’s the real vision driving the move to EHRs. They’re so much more than digital filing cabinets; they're the central nervous system of how we deliver care today.
The switch from stacks of manila folders to intelligent, connected records is a game-changer. It’s not just about swapping paper for screens. It’s about building a smarter, safer, and more connected environment for everyone involved, from the front desk to the operating room.
From Paper Chaos To Digital Clarity
Not long ago, a patient's medical history was a messy puzzle. Bits and pieces were scattered across different clinics, often incomplete, and physically stuck in one location. This kind of fragmentation wasn’t just inconvenient—it could be dangerous, leading to missed information, repeated tests, and slower diagnoses.
EHRs are designed to pull all those threads together into a single, clear story. This gives clinicians the full context they need to make better, faster decisions right when it matters most. Of course, getting to that point of clarity means tackling some very real challenges, which we’ll get into.
At its core, an EHR system is meant to be the single source of truth for a patient's health journey. It ensures every provider, whether it's a family doctor or a specialist surgeon, is on the same page with the most current and complete information.
This move toward unified data is especially vital in highly specialized areas like medical imaging. A lot of off-the-shelf EHRs, for example, really stumble when it comes to handling and displaying complex DICOM files from MRIs or CT scans. This is a problem we solve every day at PYCAD. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, making the whole process feel effortless. Our solutions let doctors view and analyze critical images right inside the patient’s record, getting rid of those frustrating workflow bottlenecks. You can see what this looks like in action over on our portfolio page.
Ultimately, getting a firm grip on the pros and cons of EHRs is the first step toward a future where technology truly serves patients and providers. This guide will walk you through both sides of the coin, giving you a balanced view of this essential evolution in medicine.
The Upside: What EHRs Bring to the Table

To really get to the heart of the EHR debate, we have to start with their most powerful promise: turning fragmented patient care into a single, continuous story. When done right, an EHR isn’t just software; it becomes a clinician's most trusted partner, bringing much-needed clarity to the front lines of medicine.
The most obvious win is having a patient's complete narrative right at your fingertips. Gone are the days of chasing down misplaced charts or waiting on a fax from another hospital. In just a few clicks, a doctor can see everything—allergies, medications, past surgeries, chronic conditions—all laid out in one place.
This is more than just convenient; it's a lifesaver in an emergency, where every second is critical. It empowers clinicians to make split-second decisions with the full picture, drastically cutting the risk of preventable medical errors.
Tearing Down the Silos for Better Teamwork
EHRs do more than just help individual doctors; they build bridges between entire care teams. Think about a patient with a complex condition seeing a cardiologist, a kidney specialist, and their family doctor. Without a shared digital record, these professionals are often working in the dark, leading to duplicate tests or even conflicting treatment plans.
An EHR changes all of that. It creates a common ground where every member of the care team can see updates, lab results, and notes in real time. This ensures everyone is on the same page, leading to a much more unified and effective way of managing patient health.
This connected approach saves time and money, but more importantly, it elevates the quality of care. It's the digital equivalent of having the entire care team in the same room, mapping out the best path forward for their patient.
Your Digital Co-Pilot for Patient Safety
One of the most profound benefits of an EHR is its role as a tireless guardian of patient safety. These systems aren't just for storing information; they actively help prevent harm.
At their best, EHRs act as a built-in safety net. They're programmed to flag potential drug interactions, send allergy alerts, and pop up with reminders for routine health screenings. Think of it as an ever-watchful co-pilot, helping clinicians catch potential problems before they happen.
These automated checks add a vital layer of protection. For instance, if a doctor prescribes a medication that clashes with a patient's known allergy, the EHR will sound the alarm instantly. It's a simple feature that prevents thousands of dangerous medication errors every year. You can dive deeper into these intelligent safeguards in our guide on clinical decision support systems: https://pycad.co/what-is-clinical-decision-support-system/
This shift isn't just a trend; it's a fundamental change in how healthcare operates. By 2025, over 95% of U.S. hospitals had fully adopted EHRs, a huge leap from just 80.5% in 2015. The global EHR market, valued at USD 32.97 billion in 2024, is expected to soar to USD 50.78 billion by 2033, fueled by a worldwide push for better healthcare data.
Making the Entire Operation Run Smoother
The impact of EHRs goes far beyond the examination room. A huge reason for their adoption is the drive toward transitioning to paperless operations, which brings a ton of efficiency gains.
EHRs streamline countless administrative chores that used to eat up so much time:
- Smarter Billing: The system can automatically generate billing codes from documented services, cutting down on errors and speeding up payments.
- Easier Reporting: Pulling data for public health agencies or quality-of-care reports becomes incredibly simple when all the information is already structured and accessible.
- Better Scheduling: Integrated calendars and scheduling tools help clinics manage appointments, reduce no-shows, and keep the day flowing smoothly.
All this automation frees up doctors, nurses, and staff to focus on what truly matters: the patient. It's something we're passionate about at PYCAD. By developing custom web DICOM viewers and embedding them directly into medical platforms, we help specialists analyze critical images without ever leaving the EHR. This kind of seamless integration is what unlocks the true power of a digital health system.
To see the benefits of EHR implementation at a glance, we've broken them down in the table below.
Key Advantages Of EHR Implementation
| Benefit Category | Specific Advantage | Impact On Healthcare Delivery |
|---|---|---|
| Clinical Quality | Instant access to comprehensive patient history. | Empowers clinicians to make faster, more informed decisions, especially in emergencies. |
| Patient Safety | Automated alerts for allergies and drug interactions. | Acts as a digital safety net, significantly reducing the risk of preventable medical errors. |
| Care Coordination | Real-time, shared access to patient data for all providers. | Breaks down communication silos, leading to more cohesive and effective team-based care. |
| Operational Efficiency | Automation of billing, coding, and scheduling tasks. | Frees up staff from administrative burdens to focus more time and energy on direct patient care. |
| Data & Analytics | Structured data collection for population health insights. | Enables proactive health management, research, and identification of public health trends. |
As you can see, the advantages ripple out from the individual patient to the entire healthcare organization, creating a more connected, safer, and efficient system for everyone.
Navigating The Hurdles And Hidden Costs
Let's be honest: bringing an EHR system into a healthcare setting isn't a simple flip of a switch. It's a massive undertaking, and like any major project, it comes with its fair share of challenges. While the potential rewards are huge, ignoring the real-world obstacles is a surefire way to end up with a frustrated team and a system that falls short of its promise.
The first hurdle is usually the most obvious one: the money. The price tag on the EHR software itself is just the tip of the iceberg. To get a true picture of the investment, you have to look at the entire ecosystem of costs that comes with it.
Peeling Back The Layers Of Financial Investment
Think of it like buying a house. The list price is just the starting point. You still have to account for closing costs, inspections, moving expenses, and future maintenance. It's the same with an EHR, and getting blindsided by these "hidden" costs can blow a hole in even the most carefully planned budget.
You absolutely have to plan for a whole range of related expenses:
- Hardware Upgrades: Can your current network, servers, and computers even run the new system effectively? More often than not, the answer is no. This means a significant upfront investment in new infrastructure is on the table.
- Implementation and Customization: Getting an EHR running isn't a plug-and-play operation. It's a complex process of migrating old data, customizing workflows to match how you actually work, and connecting it to all your other software. All of that requires paying for professional services.
- Ongoing Maintenance and Support: Don't forget the recurring costs. Annual license renewals, software updates, and technical support contracts are expenses that will be in your budget year after year.
These financial realities are a critical part of the "cons" side of the EHR equation. If you fail to budget for the whole picture, you'll end up with an underfunded system that no one can use to its full potential.
The Human Element And The Risk Of Burnout
Beyond the balance sheet, there’s a far more personal—and arguably more critical—challenge: the toll an EHR can take on your clinical staff. A clunky, poorly implemented system can quickly become a major source of daily frustration, feeding into the already serious problem of physician burnout. The very tool meant to make care better can sometimes feel like a wall between a doctor and their patient.
This burnout usually comes from a few key pain points:
- Clunky User Interfaces: Let’s face it, many EHRs aren't exactly known for being user-friendly. Forcing a busy clinician to navigate confusing menus and click through endless screens just to chart a simple visit is a massive time-waster.
- "Death by a Thousand Clicks": The documentation burden can be staggering. Clinicians often find themselves spending more time satisfying the EHR's data entry requirements than they do talking with their patients.
- Alert Fatigue: The system is constantly pinging you with alerts. While well-intentioned, the constant stream of low-priority or irrelevant pop-ups can numb clinicians to the point where they might accidentally ignore a genuinely critical warning.
The goal should always be to make technology serve the clinician, not the other way around. When an EHR forces a doctor to bend to its will, it breaks the natural rhythm of patient care and adds a layer of mental exhaustion that directly contributes to burnout.
At PYCAD, we see this struggle all the time, especially in highly specialized fields like medical imaging. That’s why we at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms our clients already use. By making crucial imaging data instantly accessible within the main workflow, we eliminate the need to juggle multiple programs, cutting down on friction and giving specialists their most valuable asset back: time. You can see how we make this happen on our portfolio page.
Overcoming Technical Pitfalls And The Learning Curve
Finally, you have to be ready for the technical growing pains that come with such a huge operational shift. The move from paper charts to digital—or even from an old EHR to a new one—is almost never a perfectly smooth ride. It takes patience, a solid plan, and a great support system.
The learning curve is usually the first mountain to climb. Everyone, from your top surgeons to your front-desk staff, needs thorough and continuous training to get comfortable with the new system. This isn't a one-and-done workshop; it's a process of ongoing support as the software gets updated and your workflows evolve.
Then there’s the ever-present risk of system downtime. Whether it's for planned maintenance, a software glitch, or a security issue, any time the EHR is offline, your entire operation can grind to a halt. This makes having a reliable system and a rock-solid backup plan completely non-negotiable. A well-thought-out implementation strategy, built with input from the people who will actually be using the system, is what turns a rocky transition into a successful evolution of care.
Solving The Medical Imaging And Interoperability Puzzle
One of the greatest promises of an EHR is a complete, unified patient story. Yet, in practice, that promise often feels just out of reach. We've all seen it: different systems from different vendors simply refuse to talk to each other, creating what can only be described as digital islands.
Each island—the lab, the pharmacy, the specialist's office—holds a critical piece of the patient's record, but there are no bridges connecting them. This isn't just an IT headache; it's a real barrier to quality care. When data is siloed, clinicians are forced to make decisions with an incomplete picture, leading to redundant tests, delayed diagnoses, and dangerous gaps in a patient's medical history.
The dream of a seamless, interconnected system runs headfirst into the hard wall of poor interoperability.
The Medical Imaging Disconnect
Nowhere is this challenge more obvious than with medical imaging. Modern diagnostics depend on massive, complex files from MRIs, CT scans, and X-rays. This data is typically managed in a Picture Archiving and Communication System (PACS) using a universal format called DICOM.
Here's the problem: most standard EHRs aren't built to handle this kind of data. They're designed for text and numbers, not for storing and displaying huge, high-resolution imaging studies.
This technical mismatch creates a deeply frustrating and inefficient workflow. A radiologist might have to leave the patient’s EHR, log into a separate PACS viewer, find the right study, analyze it, then jump back to the EHR to manually type out their findings. This constant app-switching is a massive time drain and a source of friction that pulls focus away from what really matters—the patient.
This disconnect effectively shatters the promise of a unified patient record. The imaging data, often the most critical piece of the diagnostic puzzle, remains isolated. Clinicians are left to piece together the story from multiple, disconnected sources.
This diagram shows some of the most common hurdles, including the technical challenges that drive these workflow headaches.
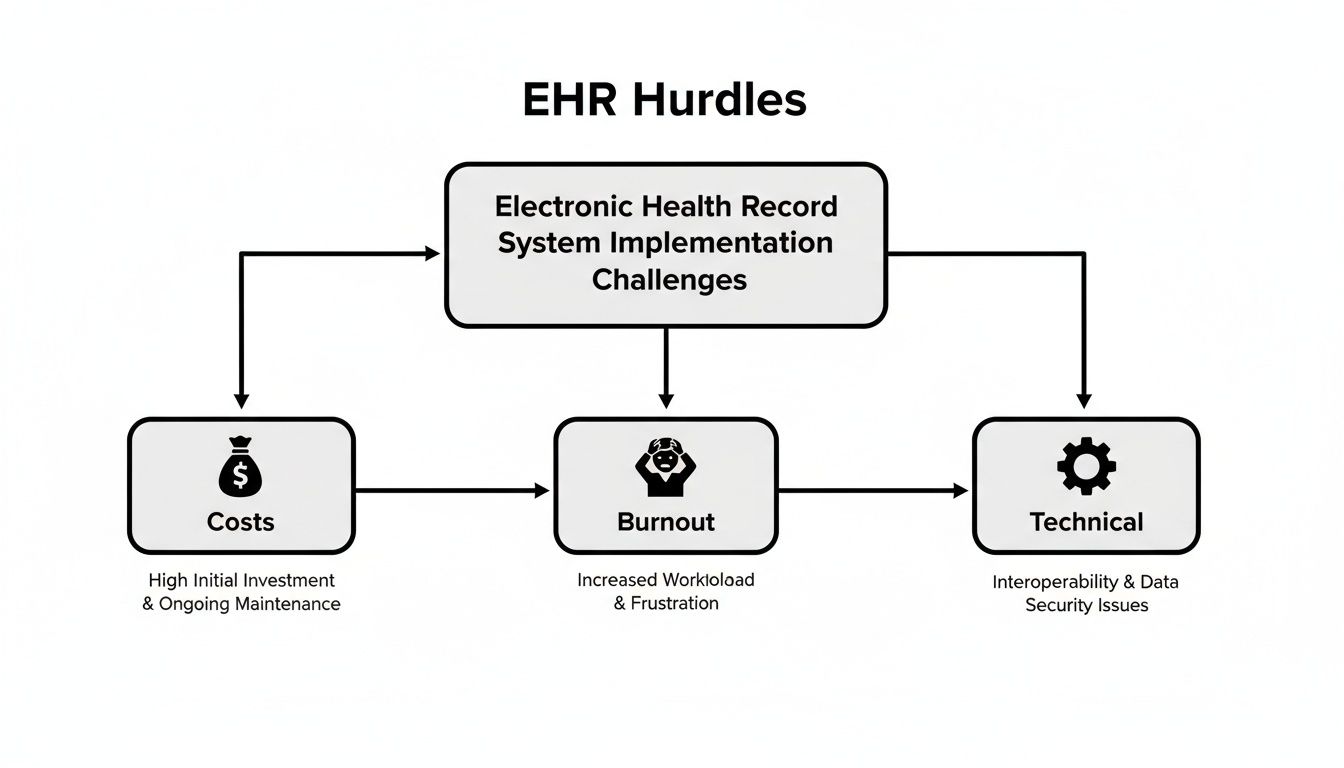
As you can see, alongside financial costs and staff burnout, technical limitations like poor interoperability form a core trio of challenges that every organization must overcome.
Building Bridges, Not Walls
Solving this imaging puzzle is exactly where we at PYCAD come in. We know that one of the biggest "cons" of many EHRs is their inability to speak the language of medical imaging.
So, we build the translator. We at PYCAD, specialize in creating custom web DICOM viewers and integrating them seamlessly into existing EHRs and medical imaging web platforms.
Instead of forcing clinicians to jump between systems, we bring the images directly into their primary workflow. Think of our solutions as a powerful bridge, connecting the isolated island of the PACS directly to the mainland of the EHR.
This integration delivers real, tangible benefits:
- A Truly Unified View: Clinicians can view and analyze a patient’s MRI, CT scan, or ultrasound right alongside their lab results, medications, and clinical notes. Everything is finally in one place.
- A Boost in Efficiency: By eliminating the need to switch applications, we slash the number of clicks and cut down on wasted time, helping specialists work faster and more accurately.
- Smarter Collaboration: When imaging is embedded in the EHR, it becomes much easier for specialists to collaborate with primary care physicians and other team members, ensuring everyone is looking at the same information.
Our mission is to tear down the digital walls that stand in the way of great patient care. Technology should adapt to the clinician's workflow, not the other way around. By building these essential integrations, we help turn a fragmented collection of data into a true, holistic patient record. You can see real-world examples of our integration work on our portfolio page.
The Future Is Integrated
The conversation around the pros and cons of EHRs is changing. It's no longer just about adopting a digital system; it's about making that system truly work for the people using it.
True interoperability is the key to unlocking the full potential of digital health, turning EHRs from passive data repositories into active, intelligent partners in care. For a deeper look at this topic, you can read our detailed guide on the interoperability of electronic health records.
By tackling specific, high-impact challenges like medical imaging integration, we can solve one of the most persistent problems in healthcare IT. The goal is a fluid, intuitive environment where technology fades into the background, allowing clinicians to focus entirely on their patients. That's the future we’re committed to building.
Balancing Data Security And Patient Privacy

In healthcare today, a patient's health information is one of your most valuable assets—and one of your biggest liabilities. The move to EHRs throws this delicate balance into the spotlight, creating a true double-edged sword for security. Protecting patient trust is everything, so we have to be brutally honest about the good and the bad.
On one hand, modern EHRs offer security features that paper records simply can't compete with. It's like swapping a filing cabinet's simple lock for a high-tech bank vault. You gain a level of control and oversight that was impossible before.
This digital fortress is built on a few powerful ideas.
- Granular Access Controls: You can set up the system so a billing specialist only sees insurance details, while a surgeon can view the entire clinical history. People only see what they absolutely need to see.
- Robust Encryption: Patient data gets scrambled both in storage and during transfer, making it completely unreadable to anyone without the right digital keys.
- Detailed Audit Trails: Every single time someone looks at, changes, or downloads a patient's file, it's logged. This digital footprint creates accountability and helps flag suspicious activity in an instant.
These features alone are a massive leap forward in guarding patient data against everyday internal threats and simple mistakes.
The High Stakes Of Centralized Data
But here's the flip side: centralizing all that data creates a much bigger, more tempting target. While losing a single paper chart is bad, a successful hack on an EHR server could expose the records of thousands—or even millions—of patients all at once. This reality has put a giant bullseye on the back of every healthcare organization.
Security in an EHR environment is not a one-time setup; it is a continuous, vigilant commitment. The threat landscape is always shifting, and protecting sensitive information requires constant adaptation and a proactive defense strategy.
Winning this ongoing battle requires more than just good firewalls and strong passwords. It means actively hunting for new threats, running regular security audits, and building a culture where every single staff member understands their role in protecting patient data. It also means mastering the complex web of regulations that govern patient privacy.
Navigating HIPAA And Beyond
At the heart of it all is the Health Insurance Portability and Accountability Act (HIPAA). This federal law is the bedrock of patient data protection, and the penalties for getting it wrong are steep. When you're dealing with specialized data like medical images, the security standards get even tougher.
To get a better sense of the technical safeguards involved, our guide on HIPAA-compliant data transfer is a great place to start.
Staying compliant isn't a "set it and forget it" task. It demands solid policies, ongoing training, and working with technology partners who truly get what’s at stake. At PYCAD, for example, security is baked into every line of code when we build a custom DICOM viewer or integrate with a new medical imaging web platform. We know that a single vulnerability can shatter the patient trust you've worked so hard to build. You can learn more about our commitment to secure solutions on our portfolio page.
In the end, EHR security is a shared responsibility. It's a blend of the strongest technology and the most diligent human oversight.
Crafting Your Strategic EHR Implementation Plan
Making the switch to an EHR is so much more than a tech upgrade; it’s a fundamental shift in how your organization operates. Moving from a theoretical list of pros and cons to actually getting a system up and running requires a clear, actionable game plan. Think of the challenges not as roadblocks, but as signposts pointing you toward a more connected and efficient future for patient care.
When you plan thoughtfully, those "cons" we talked about become manageable hurdles. The secret to a successful rollout is to approach it like a clinical problem: diagnose your organization's unique needs first, then prescribe the right solution.
Building Your Evaluation Checklist
Your first move should be creating a detailed checklist that bridges the gap between technology and your day-to-day clinical reality. This isn't about chasing the EHR with the longest feature list; it's about finding the one that feels like a natural extension of how your team already delivers care.
Start by getting honest answers to a few key questions:
- Workflow Alignment: Does this system actually map to our clinical workflows, or is it going to force our staff into clunky, frustrating workarounds?
- Integration Capabilities: How smoothly will it talk to our existing lab systems, billing software, and—most importantly—our medical imaging platforms?
- Scalability and Support: Can this system grow with us over the next 5 to 10 years? What kind of training and real-world support can we expect from the vendor when we hit a snag?
Answering these questions will quickly help you separate the systems that just look good in a demo from the ones that will actually work for you.
Planning For Seamless Integration
One of the most common traps is underestimating just how complex data integration can be, especially when it comes to specialized formats like medical images. An EHR that can't properly pull and display DICOM files from your PACS is only giving you half the picture. This is a non-negotiable point when you're thinking about an EHR's long-term value.
This is a problem we've spent a lot of time solving at PYCAD. We at PYCAD, build custom web DICOM viewers and integrate them into medical imaging web platforms, making sure those critical diagnostic images are right there inside the main patient record. That’s the kind of deep, specialized integration that elevates an EHR from good to indispensable.
A truly successful EHR implementation is measured not by the software itself, but by its seamless disappearance into the background of excellent patient care. The technology should empower clinicians, not distract them.
Ultimately, your strategic plan is a roadmap to empowerment. It’s about acknowledging the real-world challenges of cost and workflow disruption while keeping your eyes fixed on the incredible potential for better patient safety and efficiency. To see what this kind of seamless integration looks like in action, take a look at some of our work on our portfolio page. By choosing the right partners and planning with care, you can navigate the complexities and truly unlock the promise of a modern, digitally-driven practice.
Common Questions We Hear About EHR Systems
When you're deep in the process of evaluating EHRs, it's easy to get lost in the details. The same critical questions about cost, workflow, and patient safety tend to surface time and again. Let's tackle them head-on, turning those abstract pros and cons into a clear path forward.
What Is The Single Biggest Advantage Of An EHR System?
If you have to boil it down to one thing, it's this: a massive leap forward in patient safety and quality of care. Nothing else comes close.
Think about it. With an EHR, you have instant access to a patient’s entire story—their history, allergies, current medications. This isn't just about convenience; it's about life-saving intelligence. Decision support tools can flag a dangerous drug interaction before a prescription is even sent, preventing a medical error in real-time. That direct impact is the whole point.
How Can We Mitigate High Costs And Physician Burnout?
These are, without a doubt, the two biggest hurdles. But they are manageable if you're strategic.
To get a handle on costs, look seriously at cloud-based EHRs. They often shift the financial burden from a huge upfront investment to a more predictable operating expense.
For burnout, the key is to put your clinical team at the center of the decision. Prioritize systems with clean, intuitive interfaces. Involve your staff from day one in the selection process. Then, don't skimp on training and take the time to customize workflows. Your goal is to make the technology feel like an extension of their skills, not a barrier to them.
Our EHR Struggles With Medical Images. What Are Our Options?
This is an incredibly common frustration. Most EHRs are simply not built to handle the complexity of DICOM files from MRIs, CT scans, and other imaging.
The best way forward is to work with a specialist who can bridge that gap. At PYCAD, this is exactly what we do. We build custom web DICOM viewers and integrate them seamlessly into medical imaging web platforms and existing EHRs.
The result is a single, unified environment. A doctor can pull up a patient’s record and view their MRI or CT scan right there, without ever leaving the screen. It eliminates the clunky process of switching between systems and dramatically speeds up the diagnostic workflow.
This kind of targeted integration turns one of the biggest weaknesses of an EHR into one of its most powerful strengths.
At PYCAD, our passion is solving these very integration puzzles. We believe technology should empower clinicians, not get in their way. See how we build these powerful, unified systems by exploring our work on our portfolio page.






