In any modern hospital, the radiology department is a whirlwind of activity. At the center of it all, you'll find two critical systems working in tandem: the Radiology Information System (RIS) and the Picture Archiving and Communication System (PACS). These aren't just pieces of software; they're the digital backbone that turns medical images into life-saving diagnoses.
The Digital Heartbeat of Modern Radiology
Think of a busy air traffic control tower. You have one system managing flight plans, schedules, and communication—the logistics. You have another system showing the real-time location of every plane on a radar screen—the visual data. Radiology runs on a similar principle.
This guide will walk you through what RIS and PACS actually do, not as abstract concepts, but as the essential tools they are in a real-world clinical setting.
The easiest way to think about it is this: RIS is the "brain" of the operation, managing all the patient data, appointments, and reports. PACS, on the other hand, is the vast "visual library" where every single medical image is stored, viewed, and shared.
Distinguishing Core Functions
While they work together, their jobs are completely different. Getting a handle on their distinct roles is the key to understanding how a modern radiology department functions so effectively. One manages the workflow, the other manages the pixels.
-
Radiology Information System (RIS): This is the logistical command center. It handles all the administrative heavy lifting—scheduling patient appointments, tracking their progress through the department, managing billing, and making sure the final diagnostic reports get to the right doctors.
-
Picture Archiving and Communication System (PACS): This system is all about the images. It's a secure, high-capacity archive for every MRI, CT scan, and X-ray. It gives radiologists powerful tools to instantly pull up and analyze these images, comparing them to previous scans to see what’s changed. If you want to go deeper on this, our guide on what PACS is in healthcare is a great next step.
To make the distinction even clearer, let's break it down side-by-side.
RIS vs PACS At a Glance
This table highlights the core responsibilities of each system, showing how they complement each other without overlapping.
| Function | Radiology Information System (RIS) | Picture Archiving and Communication System (PACS) |
|---|---|---|
| Primary Role | Workflow & Data Management | Image Storage & Viewing |
| Patient Data | Manages demographics, scheduling, billing | Links images to patient records |
| Core Tasks | Patient registration, order entry, reporting | Image acquisition, archival, distribution |
| End Users | Administrative staff, technologists, radiologists | Radiologists, referring physicians, specialists |
| Key Output | Final diagnostic reports, billing statements | High-resolution medical images |
Ultimately, the RIS tells the story of the patient's journey, while the PACS provides the visual evidence.
This powerful digital partnership is why clinicians can make faster, more accurate decisions than ever before. It's no surprise that the global RIS market was valued at around USD 1.1 billion and continues to grow. This trend, highlighted by market analysis from Imarc Group, shows just how essential these integrated IT solutions have become in managing the complexities of modern healthcare.
At PYCAD, we live and breathe this stuff. We specialize in building custom web DICOM viewers and integrating them into medical imaging web platforms, constantly pushing what's possible. You can see some of our real-world solutions in the PYCAD portfolio.
Mapping the Digital Patient Journey
To really get a feel for how radiology information systems and PACS work together, let's walk through a common scenario. Picture a patient arriving for a scheduled MRI. What seems like a straightforward appointment is actually a sophisticated digital dance, a workflow honed over years to ensure every scan is fast, accurate, and safe.
This entire process is really just a series of seamless digital handshakes between different systems. It's designed to take manual work—and human error—out of the equation, starting the very moment a doctor orders the scan.
The Order and The Scan
The journey kicks off in the Radiology Information System, or RIS, which you can think of as the air traffic control for the entire imaging department.
-
Placing the Order: A physician's request for an MRI is entered into the RIS. This might happen directly in the radiology department or, more commonly, through an integration with the hospital's main Electronic Health Record (EHR). This isn't just a simple request; it carries all the crucial patient details, clinical history, and the exact type of exam needed.
-
Scheduling and Building the Worklist: The RIS takes that order and helps schedule the appointment. The moment it's booked, the system automatically adds the patient to a technologist's worklist. This is a dynamic queue, telling the MRI tech precisely who's next, what scan to perform, and any special instructions to be aware of.
-
At the Modality: When the patient is ready, the technologist simply selects their name from that worklist, right on the MRI machine's console. All the patient data from the RIS flows over automatically, guaranteeing the images will be tagged to the correct person. This one step is a powerful safeguard against mixing up patient files, a potentially catastrophic error.
Once the scan is done, the digital images are ready for the next leg of their journey.
From Pixels to Diagnosis
The freshly captured images are now sent over to the Picture Archiving and Communication System (PACS). This is the department's high-security digital library. The PACS immediately archives the images and links them to the correct patient record, using the data that originated in the RIS.
This diagram helps visualize how information moves from the RIS to the PACS, all the way through to the final diagnosis.
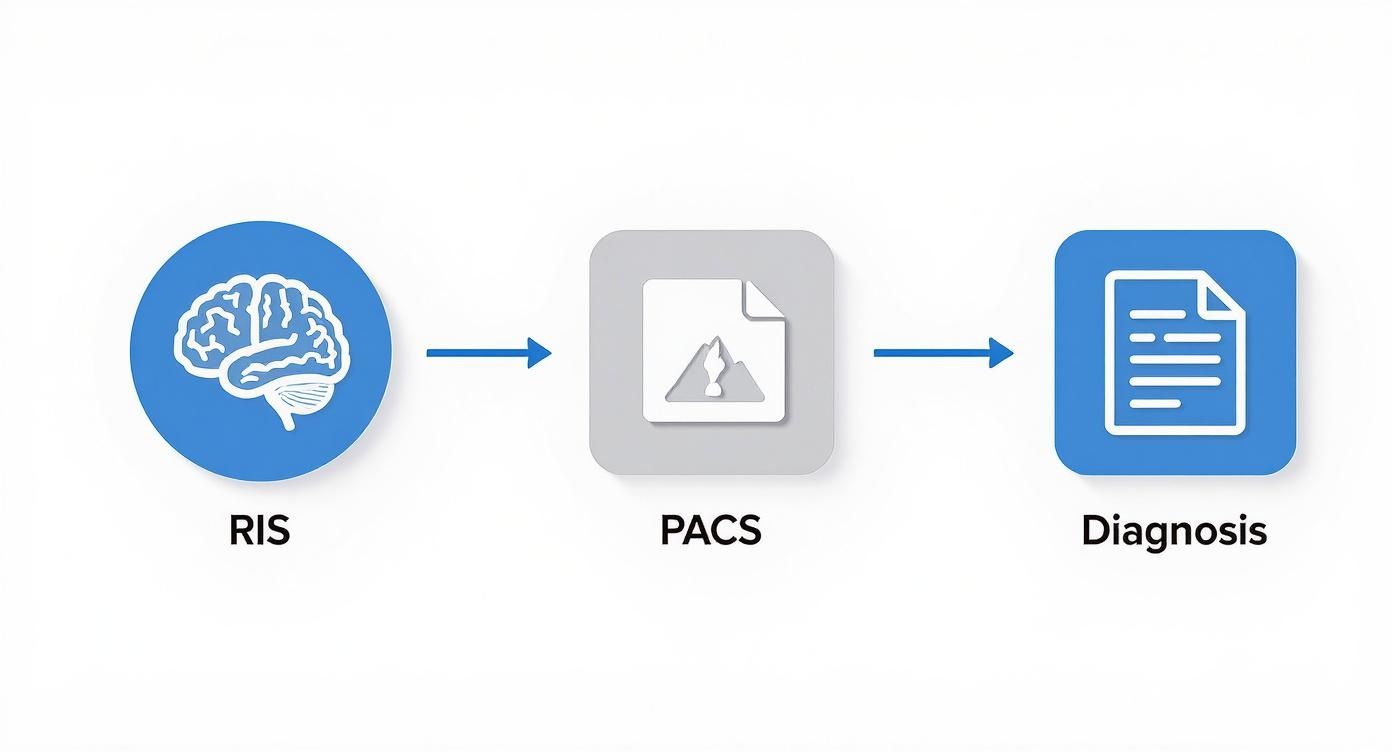
As you can see, it’s a clean, logical handoff. Each system passes the baton to the next, ensuring the patient's record remains complete and accurate from start to finish.
The study then pops up on the radiologist's reading worklist. They can instantly pull up the new MRI from the PACS and, just as importantly, retrieve any prior scans for comparison. This gives them the full story, leading to a much richer diagnosis.
Using a specialized DICOM viewer, the radiologist can now dive in, meticulously analyzing every detail of the images. This is where human expertise and powerful technology meet. Here at PYCAD, this is exactly what we do—we build custom web DICOM viewers and integrate them into medical imaging web platforms, giving clinicians the advanced tools they need for precise interpretation.
Closing the Loop
After finishing their analysis, the radiologist dictates their findings. This report is then transcribed and finalized right inside the RIS, which now acts as the official record for the diagnostic text.
The final, signed report is automatically sent back to the referring physician's EHR and is also permanently linked to the images sitting in the PACS. The patient's record is complete, the billing information is triggered, and the communication loop is closed.
This entire journey, from a simple order to a final report, is a beautiful example of the harmony between RIS and PACS. It’s a workflow that directly leads to faster diagnoses and better patient care. To see how custom development can perfect this flow, feel free to explore some of our work in the PYCAD portfolio.
Speaking the Same Language in Medical Imaging
For a radiology department to function, its core systems—the RIS and the PACS—have to be in constant conversation. But what if they don't speak the same language? Imagine a RIS from one company trying to send an imaging order to a PACS from another. Without a shared vocabulary, that critical information gets lost in translation. The entire system grinds to a halt.
This is why we have universal standards. They act as the essential translators, ensuring that a CT scan taken in a New York hospital looks exactly the same to a specialist viewing it in California. They guarantee that when a patient checks in, their name and medical record number flow seamlessly from the front desk to the RIS and right onto the imaging machine.
Without these common languages, healthcare would be a chaotic mess of disconnected data silos. Let's break down the three foundational standards that make modern medical imaging possible.
DICOM: The Universal Blueprint for Images
At the very core of any PACS is DICOM (Digital Imaging and Communications in Medicine). The simplest way to think about DICOM is as the JPEG or PDF of the medical world, but with superpowers. It’s the global standard for how we transmit, store, retrieve, and view medical images.
When an MRI scanner captures an image, it doesn't just save a picture. It bundles that image into a DICOM file, which is packed with a rich layer of critical metadata. This includes:
- Patient Information: Name, ID, date of birth, and everything needed to link the image to the right person.
- Study Details: The type of scan, when it was performed, and which doctor ordered it.
- Equipment Data: Details about the scanner itself, like the manufacturer and specific settings used.
This metadata is what makes DICOM so powerful. It ensures every image is permanently and accurately tied to the correct patient and clinical context. It's why any DICOM-compliant viewer can open an image from any DICOM-compliant scanner, no matter who made the equipment.
HL7: The Workhorse for Clinical Workflows
If DICOM is all about the images, HL7 (Health Level Seven) is about everything else. HL7 is the messaging standard that lets all the other clinical systems talk to each other. It’s the quiet, behind-the-scenes workhorse that keeps the RIS, the hospital's Electronic Health Record (EHR), and even the billing systems perfectly in sync.
When a doctor orders a scan in the EHR, an HL7 message zips over to the RIS to create the worklist. When a radiologist dictates their findings, another HL7 message delivers that final report straight back into the patient's chart in the EHR.
HL7 messages are the invisible couriers of healthcare, constantly carrying small, vital packets of data around the hospital. They manage admissions, patient transfers, orders, and results, weaving dozens of separate applications into one cohesive system.
This standard is what truly powers efficient workflows. By automating this constant flow of information, HL7 gets rid of tedious manual data entry, slashes the risk of human error, and makes sure the entire care team is working with the same real-time information. To learn more about how these systems connect, our guide on understanding PACS integration is a great next step.
FHIR: The Modern, Flexible Future
The newest player on the scene is FHIR (Fast Healthcare Interoperability Resources), and it's built for the internet age. While HL7 is incredibly powerful, it can be a bit rigid and complex to work with. FHIR was designed from the ground up to be more flexible, faster, and far easier for developers to implement.
Think of FHIR as the next evolution of HL7, built with the same technology that powers modern websites and apps. It breaks down massive, complex medical records into small, logical chunks called "resources"—things like a patient's contact info, a single lab result, or a known allergy.
This modular approach makes it incredibly simple for an application to ask for only the specific piece of data it needs, rather than a whole document. This is already unlocking incredible new tools, from patient-facing apps that pull up lab results on a smartphone to physician portals that seamlessly combine data from multiple hospital systems. FHIR isn't just a new standard; it's the engine that will drive the next generation of healthcare interoperability.
Choosing Your Deployment Model
Deciding how to deploy your radiology information systems and pacs is one of the most foundational choices you'll make. Think of it like this: are you going to build your own private power plant, or will you tap into the city's electrical grid? Each path has real-world consequences for your budget, your control over operations, and your ability to grow.
This decision really comes down to a simple question: where will your data live, and who's responsible for the machines that store it? The answer will shape your IT strategy for years to come, dictating everything from capital expenses to the skills you need on your team.

The Traditional On-Premise Approach
Going with an on-premise model means you own it all. The hardware, the software, the data center—it's all yours, housed within your own facility. It’s the equivalent of owning your home; you have total say over every server, every network cable, and every security protocol.
This gives you an unmatched level of control, which is a huge plus when you're dealing with sensitive patient data. But that control comes with some heavy responsibilities.
- Upfront Investment: You're looking at a significant capital expenditure (CapEx) to buy the servers, storage, and software licenses right out of the gate.
- IT Overhead: It requires a dedicated, skilled IT team on your payroll to manage installation, run constant maintenance, and troubleshoot when things go wrong.
- Physical Space: You need a secure, climate-controlled data center to house everything, which isn't a small ask.
For large, established institutions that already have a robust IT department and prefer to keep a tight grip on their data, the on-premise model is a proven, reliable choice.
Embracing the Flexibility of the Cloud
A cloud-based model is the polar opposite. It’s like leasing a top-floor apartment in a luxury high-rise. You don't own the building, but you get access to world-class amenities, and a professional team handles all the security and maintenance for you.
With a cloud deployment, a specialized vendor hosts your RIS and PACS on their secure, remote servers. Your team accesses everything they need right over the internet. This model has absolutely taken off for some very compelling reasons.
The industry data backs this up. Hospitals and clinics, which make up over 82% of the Radiology Information Systems market, are increasingly choosing web-based systems for their sheer convenience and scalability. It’s a clear shift toward more agile solutions, a trend you can explore in global RIS trends.
The cloud fundamentally changes how you pay for IT. It turns a massive upfront capital investment into a predictable, monthly operational expense (OpEx). This simple shift makes budgeting far easier and gives you much more financial wiggle room.
Finding Balance with a Hybrid Model
Of course, this isn't an all-or-nothing decision. A hybrid model is a pragmatic "best of both worlds" strategy. It beautifully combines the hands-on control of an on-premise system with the amazing flexibility of the cloud.
For instance, a hospital might keep its active PACS storage on-site for the fastest possible image retrieval during patient care. At the same time, they could use a cost-effective cloud service for long-term archiving and disaster recovery. This approach lets you build an infrastructure that perfectly matches your clinical workflows and financial realities.
Here at PYCAD, we live and breathe these modern architectures. We build custom web DICOM viewers and integrate them into medical imaging web platforms, often deploying them in cloud or hybrid setups to deliver the best possible performance and accessibility. You can see how we put these ideas into practice in our PYCAD portfolio.
To help you visualize the trade-offs, here’s a straightforward comparison of the three models.
Comparison of RIS and PACS Deployment Models
This table offers a detailed look at the key differences between on-premise, cloud-based, and hybrid solutions for deploying medical imaging systems.
| Criteria | On-Premise | Cloud-Based | Hybrid |
|---|---|---|---|
| Cost Structure | High upfront capital expense (CapEx) for hardware and software. | Predictable operational expense (OpEx) through subscriptions. | Mix of CapEx and OpEx, tailored to specific needs. |
| Scalability | Limited and requires purchasing new hardware for expansion. | Highly scalable, allowing you to easily adjust storage and computing power. | Flexible scalability, leveraging the cloud for growth while keeping core data on-site. |
| Maintenance | Managed entirely by an in-house IT team, requiring significant expertise. | Handled by the vendor, freeing up internal IT resources. | Shared responsibility between the in-house team and the cloud provider. |
| Accessibility | Access is typically restricted to the internal network. | Securely accessible from any location with an internet connection. | Combines on-site access with flexible remote capabilities. |
Ultimately, choosing the right path forward is a strategic decision. It hinges on your organization’s budget, the strength of your IT resources, and your long-term vision for your radiology information systems and PACS.
Unlocking Advanced System Capabilities
Standard, off-the-shelf radiology information systems and pacs are a great starting point. They get the job done. But let’s be honest—every medical practice has its own unique rhythm, its own distinct set of challenges. This is where we go from good to great, turning a standard setup into a powerhouse of efficiency through custom integration.
Think of it less as a simple software tweak and more as creating a truly unified environment. When you integrate your RIS and PACS with other essential platforms—like your Electronic Health Record (EHR), billing systems, and patient CRM—you’re not just connecting boxes. You’re tearing down the walls between them and creating a single, seamless flow of information.
The result? A patient's journey is smooth and connected, from the moment they book an appointment in the CRM to the day their final bill is processed. It's a strategic move that slashes manual data entry, cuts down on errors, and gives your clinical team back the time they need to focus on what they do best: patient care.
The Evolution of the DICOM Viewer
The image viewer is one place where this customization pays huge dividends. For decades, radiologists were anchored to specific, high-powered workstations loaded with proprietary software. That model worked, but it created bottlenecks, limited access, and made remote collaboration a real headache.
That world is long gone. Modern, web-based DICOM viewers have completely changed the game, built for how healthcare works today. They provide what’s known as zero-footprint access, a fancy way of saying a clinician can pull up high-resolution diagnostic images right in a web browser. No plugins, no special software, no fuss.
This leap forward gives clinicians secure, on-the-go access to the images they need, when they need them. A specialist can review a critical CT scan on a tablet from home just as easily as they could at their workstation in the hospital.
At PYCAD, we don't just use off-the-shelf viewers; we build custom web DICOM viewers and bake them directly into a medical imaging platform. This lets us craft solutions that are perfectly molded to how a client actually works, not how a software vendor thinks they should work.
Building for Tomorrow's Teleradiology Needs
This shift towards flexible, web-based solutions is opening up incredible new opportunities, especially in teleradiology. Picture Archiving and Communication Systems (PACS) have been at the heart of radiology's digital transformation, but it was the creation of standards like DICOM that truly unlocked the interoperable, multi-vendor world we have today. You can learn more about this journey from this in-depth overview by the U.S. Department of Veterans Affairs.
Custom viewers take this potential to the next level by bringing sophisticated tools directly into the browser.
- Advanced Visualization: Powerful features like 3D rendering and multi-planar reconstruction (MPR) are no longer trapped in the reading room.
- Collaborative Features: Imagine specialists from different hospitals consulting on a complex case in real-time, sharing their screen and making annotations together.
- AI Integration: A custom viewer can be built to seamlessly display insights from AI algorithms, overlaying heatmaps or flagging potential anomalies for the radiologist to review.
By embracing custom solutions, healthcare organizations can create an imaging ecosystem that not only solves today's problems but is agile enough to adapt to whatever comes next. To see what this tailored approach looks like in the real world, I invite you to explore some of our work in the PYCAD portfolio.
Navigating Security and Compliance
In healthcare, patient data is more than just information—it’s a sacred trust. When it comes to radiology information systems and pacs, protecting that trust isn't a feature; it's the bedrock of the entire operation. Security and compliance are the silent guardians, ensuring every piece of sensitive data stays confidential, whole, and visible only to those who absolutely need it.

This commitment isn't just about setting a strong password. It’s a deep, multi-layered strategy built to fend off threats and comply with ironclad regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. This law sets the standard for how Protected Health Information (PHI) is handled, demanding uncompromising safeguards.
Building a Fortress Around Patient Data
Think of a truly secure RIS/PACS environment as a fortress, built on three core pillars. These aren’t just technical checkboxes; they are foundational principles that must be woven into the very fabric of your daily operations, from the server room right to the clinician's monitor.
-
Robust Access Controls: This is the principle of least privilege in action. People should only be able to access the specific information they need to perform their jobs, and nothing more. Role-Based Access Control (RBAC) makes this real, ensuring a front-desk scheduler can’t access the same diagnostic tools as a board-certified radiologist.
-
Comprehensive Audit Trails: Every single action within the system must leave a digital footprint. From a login attempt to a viewed image or an edited report, it all gets logged. These audit trails are your system’s black box, providing indisputable accountability and proving invaluable when investigating a potential security incident.
-
End-to-End Data Encryption: Data needs to be unreadable to unauthorized eyes, always. That means it must be encrypted both "at rest" while sitting in the PACS archive and "in transit" as it flies across the network. If you want to dive deeper, our article covering https://pycad.co/hipaa-compliant-data-transfer/ offers a fantastic breakdown.
Protecting patient data isn't just a legal chore; it's an ethical duty. A single breach can shatter patient trust and cause lasting harm, which is why proactive security has to be an institutional imperative.
Practical Measures for a Secure Ecosystem
Putting these principles into practice takes a smart blend of technology and disciplined processes. Evaluating a range of enterprise security software solutions is a crucial step toward building a comprehensive defense for your RIS/PACS environment.
But software alone isn't enough. Secure network configurations and regular, thorough security audits are just as critical. Think of these audits as a routine health check-up for your systems, helping you spot vulnerabilities before they can ever be exploited. This layered approach is the only way to truly protect patients, defend the institution’s reputation, and maintain the integrity of the entire diagnostic journey.
At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms, and we place security at the heart of every architectural decision. You can see examples of how we embed this security-first mindset into our work by viewing the PYCAD portfolio.
A Few Common Questions
Diving into the world of radiology information systems and PACS often sparks a few questions. These systems are the beating heart of modern diagnostic imaging, so getting a handle on how they work—and work together—is key for everyone from hospital IT teams to the clinicians on the floor.
Let's clear up some of the most common points of confusion. Think of this as a quick-start guide to understanding the core technology that powers today's radiology departments.
What’s the Real Difference Between a RIS and an EHR?
It’s easy to get these two mixed up, but their roles are quite distinct. An Electronic Health Record (EHR) is the big picture—it's the complete, digital chronicle of a patient's entire health story, covering everything from primary care visits to surgical notes.
A Radiology Information System (RIS), on the other hand, is a specialist. It’s purpose-built to run the show inside the radiology department. The RIS is all about managing the imaging workflow: scheduling appointments, creating radiologist worklists, and handling the reporting process. Once a report is finalized, the RIS sends that crucial piece of the puzzle over to the EHR to become part of the patient's master file.
Can a Small Clinic Get By with Just a PACS?
Absolutely. A smaller practice can definitely implement a standalone PACS (sometimes called a "mini-PACS") to handle the essentials: storing, pulling up, and viewing medical images. This gives you the digital image library you need to make diagnoses.
But here’s the catch: without a RIS, you’re missing the engine that drives the workflow. All the patient tracking, smart scheduling, and report distribution have to be done by hand. This can quickly become a bottleneck, leading to inefficiencies and even errors as the clinic gets busier. That’s why most practices, even smaller ones, find that an integrated RIS/PACS solution is the only sustainable way to grow. For more on this and other digital health topics, you can always find great articles and discussions on the Salthea Blog for Further Insights.
How Does AI Fit into the Picture?
Artificial intelligence is no longer a futuristic concept; it’s becoming an invaluable partner in the reading room, connecting directly with both the RIS and PACS to make a real impact.
Think of it this way: an AI tool can scan through images stored in the PACS, automatically flagging subtle abnormalities that might be hard to spot. It then communicates with the RIS to bump that study to the top of the radiologist’s worklist for urgent review.
AI doesn't stop there. It can also help the RIS optimize complex scheduling puzzles or even draft preliminary report findings based on what it sees in the images. It’s not about replacing the radiologist, but about giving them a powerful collaborator to improve both speed and diagnostic confidence.
Here at PYCAD, we live and breathe this stuff. We’re passionate about building the next generation of medical imaging platforms. In fact, we build custom web DICOM viewers and integrate them into medical imaging web platforms.
Curious to see what that looks like? Take a look at our work.