It’s easy to get tangled in acronyms, but the core difference between an EMR and an EHR is actually quite simple. An Electronic Medical Record (EMR) is the digital equivalent of a patient's paper chart from a single medical practice. Think of it as a detailed snapshot.
On the other hand, an Electronic Health Record (EHR) tells the whole story. It's a comprehensive, shareable history of a patient’s health that moves with them from one provider to the next—from their primary care doctor to a specialist to the hospital. If an EMR is a single chapter, the EHR is the patient’s complete health biography.
Decoding EMR and EHR
Grasping the distinction between these two systems is foundational to building a modern, connected healthcare infrastructure. Though people often use the terms interchangeably, their purpose, design, and impact are worlds apart. An EMR is built for internal efficiency—it helps a clinic track patient data, manage appointments, and handle billing. It turns paper records into digital files but essentially keeps that information siloed.
An EHR, however, is built for a much bigger purpose: collaboration. Its entire design revolves around creating a single, continuous view of a patient's health that authorized clinicians can securely access, no matter where they are. This means specialists, hospitals, labs, and imaging facilities all see the same up-to-date information, paving the way for truly coordinated care.
EMR vs EHR Key Differences at a Glance
To really nail down the differences, it helps to see them side-by-side. This table breaks down the essential attributes that set EMR and EHR systems apart, focusing on their scope, connectivity, and ultimate goal in patient care.
| Attribute | Electronic Medical Record (EMR) | Electronic Health Record (EHR) |
|---|---|---|
| Data Scope | Patient information from a single clinic or practice. | Comprehensive patient data from multiple healthcare providers. |
| Interoperability | Limited; not designed to share information outside the practice. | High; designed for seamless data sharing across different systems. |
| Patient Journey | A snapshot of care from one specific location. | A complete, longitudinal view of a patient’s entire health history. |
| Primary Goal | Digitize internal records for diagnosis and treatment within one office. | Enable coordinated, patient-centered care across the whole health ecosystem. |
Looking at it this way, the strategic value of each system becomes clear. While an EMR solves an internal documentation problem, an EHR tackles the much larger challenge of creating a connected and informed healthcare network for every patient.
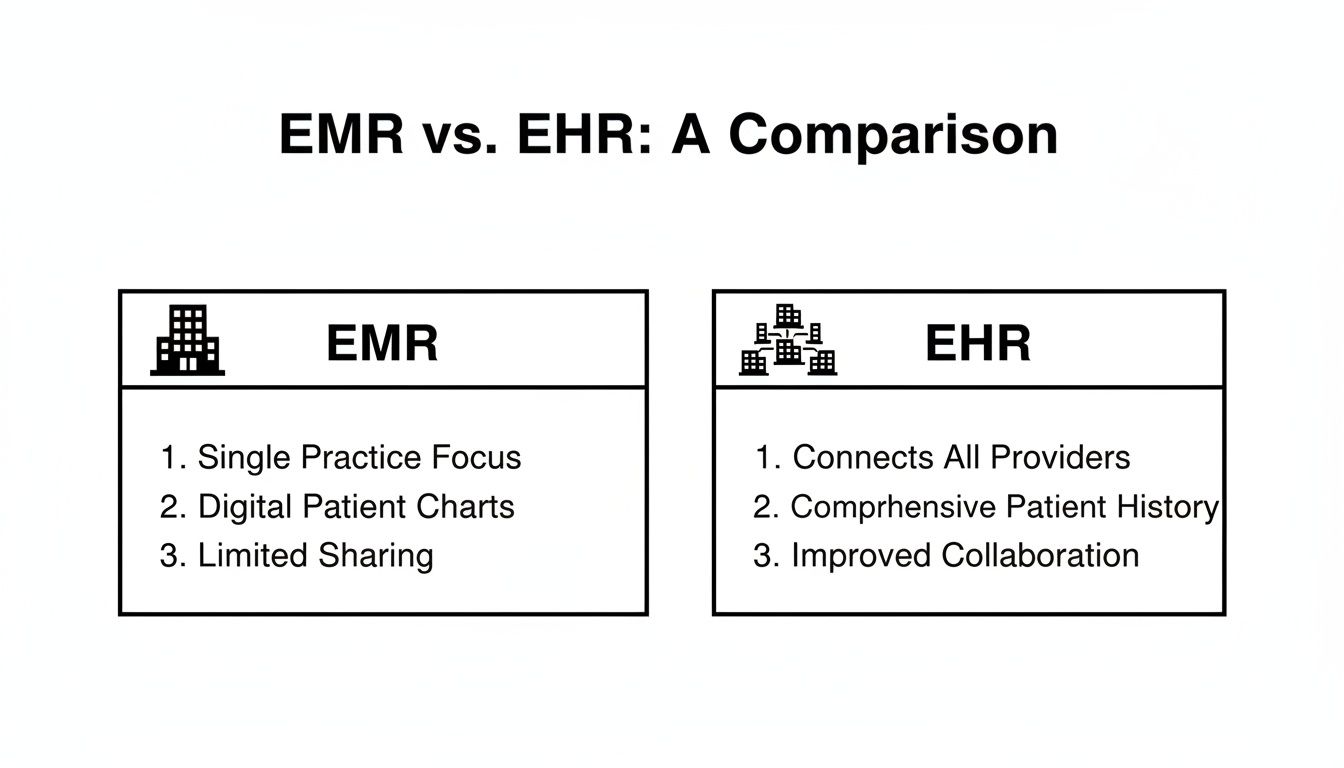
This visual really drives the point home. It shows how an EHR’s networked model supports a far more holistic and collaborative approach to patient care compared to the isolated structure of an EMR.
At PYCAD, this distinction is critical. We build custom web DICOM viewers and integrate them into medical imaging web platforms, and that work depends on the interoperable foundation an EHR provides. You can see how we bring these concepts to life by exploring our past projects.
Comparing Technical and Functional Capabilities
To really get to the heart of the EMR vs. EHR debate, we have to look under the hood at their technical architecture. The core difference isn't just a matter of semantics; it’s about their fundamental design philosophies. This split in their DNA—specifically in data scope and the ability to communicate—shapes everything from daily clinical workflows to long-term patient health.
Think of an EMR as a digital fortress. It's engineered as a closed-loop system, designed to meticulously document and manage information within a single practice.
An EHR, on the other hand, is built to be an open ecosystem. Its purpose goes far beyond simple storage. It's designed from the ground up to share information intelligently and securely across the entire healthcare landscape. That single architectural choice is what truly sets them apart.
Data Scope and Patient History
The most obvious technical split is in the breadth of data each system is designed to handle. An EMR’s perspective is inherently narrow, almost episodic. It contains only the information gathered within the walls of a single clinic, capturing diagnoses, treatment plans, and test results from one provider. What you get is a series of disconnected snapshots of a patient's health.
In stark contrast, an EHR is all about creating a longitudinal patient record. It’s built to pull together data from every touchpoint—primary care physicians, specialists, hospitals, labs, and pharmacies—to construct a single, continuous health story. This panoramic view is absolutely essential for understanding a patient’s full history and making truly informed decisions.
An EMR is like a diary kept in one location, documenting isolated events. An EHR is like a shared, cloud-synced biography, collaboratively written and accessible to all authorized contributors, providing a complete and dynamic life story.
The real-world implications here are huge. Imagine a patient with a chronic condition who sees multiple specialists. Each specialist’s EMR offers only a sliver of the full picture. But an EHR provides a unified, coherent timeline that every provider can access, which helps eliminate redundant tests and dramatically improves care coordination.
Interoperability and Communication Standards
This is where the technical chasm between the two systems becomes a canyon. Interoperability—the ability for different IT systems to seamlessly exchange and actually use information—is the defining feature of an EHR. These systems are built on a foundation of universal communication standards.
You'll often hear about a couple of key standards:
- Health Level Seven (HL7): This is a long-standing set of international standards for moving clinical and administrative data between different software applications.
- Fast Healthcare Interoperability Resources (FHIR): A more modern standard that uses APIs to make data exchange quicker and more efficient, especially for web and mobile platforms.
EMRs, by their very nature, were not built for this. They often function as digital islands. Getting records out of an EMR usually means falling back on manual processes like printing, faxing, or exporting data into a clunky, non-standard format. If you want to dive deeper into the weeds on this, the challenges around https://pycad.co/interoperability-of-electronic-health-records/ are complex but critical to understand.
EHRs, however, use standards like HL7 and FHIR to ensure that a lab result from a hospital can flow directly and securely into a patient’s record at a clinic across town. It just works.
When you're evaluating how solid these systems are, you also have to consider the quality assurance behind them. For example, robust test automation in healthcare is non-negotiable for ensuring these complex systems perform reliably.
This commitment to open, fluid data exchange is precisely why we at PYCAD build on EHR-based platforms. When we build custom web DICOM viewers and integrate them into medical imaging platforms, we depend on that seamless flow of information. An EHR’s architecture is the only foundation that can support this level of advanced integration, and you can see real examples of this work on our portfolio page.
Weaving Medical Imaging and AI into Your Clinical Fabric
When we get right down to it, the whole EMR vs. EHR debate really comes alive when you start talking about the future. Your choice of a records system isn't just about storing data; it's about what you can do with that data. It directly shapes your ability to plug in powerful tools like medical imaging viewers and artificial intelligence, and this is where an EHR’s design truly shines.
EHRs are built with connection in mind. They often come equipped with robust APIs that serve as secure, managed gateways for other systems to talk to them. This open architecture is exactly what you need to build a truly intelligent, interconnected healthcare platform. A closed-off EMR, by contrast, can feel like a brick wall, making this kind of deep integration a frustrating, uphill battle.
The Bedrock of Advanced Integration
At PYCAD, we live this reality every day. We build custom web DICOM viewers and integrate them into medical imaging web platforms, and this entire process hinges on the smooth, reliable data flow that an EHR provides. A well-designed EHR ecosystem lets specialized tools, like our DICOM viewers, pull the right patient data at the right time, presenting imaging studies with the full clinical story wrapped around them.
Think about the impact on a radiologist's workflow. Instead of juggling separate applications, they can view a CT scan directly inside the patient's EHR, instantly seeing their complete history, recent lab results, and current medications. This holistic view is absolutely essential for a precise diagnosis. It's a world away from the old-school approach of viewing images in a vacuum, which is often the reality with legacy EMRs. You can see some of these integrated platforms in action on our portfolio page.
The choice between an EMR and an EHR isn't just about digital records. It's a fundamental decision: do you want a digital filing cabinet, or do you want an intelligent, dynamic hub for patient care?
An EHR's role as the central source of truth is also mission-critical for building out effective clinical decision support systems. These systems need a deep, rich well of data to draw from if they're going to give clinicians genuinely helpful alerts and guidance when it matters most.
Igniting AI and Sharper Clinical Decisions
Artificial intelligence is no longer a sci-fi concept; it's becoming a real-world partner in diagnostics and treatment planning. But here’s the catch: for AI algorithms to deliver on their promise, they need a ton of high-quality, diverse data. They thrive on the kind of comprehensive, longitudinal patient stories that are meticulously stored in an EHR. The narrow, episodic snapshot from an EMR just doesn't cut it for training or deploying sophisticated AI models.
This practical difference has massive technical and commercial implications. The numbers back this up, too. Market analysis consistently shows that facilities using interoperable EHRs have far higher rates of successful system-to-system data exchange. With the EHR market expected to blow past $30 billion annually and cloud-based systems becoming the norm, the runway for deploying integrated DICOM viewers and AI tools is getting longer and clearer. If you're curious about the market dynamics, you can discover more insights about EHR industry statistics.
As you plan your own journey into these advanced technologies, it pays to look at the bigger picture across healthcare. Innovations in parallel fields can offer a fascinating preview of what’s to come, like the trends explored in an article about the future of physical therapy with AI-driven diagnostics and telehealth. It all points to the same conclusion: the future belongs to interconnected, data-rich ecosystems, a future that an EHR is uniquely built to support.
Choosing the Right System for Your Needs
Theory is one thing, but putting it into practice is a whole different ballgame. Deciding between an EMR and an EHR isn’t just a technical choice—it comes down to your daily operations, your vision for growth, and your fundamental approach to patient care. You have to look past the definitions and get real about your own clinical needs.

Think about a small, independent dental practice. The main goal is keeping track of internal charts, logging patient visits, and handling billing—all within its own walls. For this kind of setup, a straightforward EMR is usually the perfect fit. It's cost-effective, digitizes the old paper charts, and makes the office run smoother, meeting all the core needs of a practice that isn't constantly sending patients to outside specialists.
Now, shift your perspective to a large regional hospital network. This system connects primary care offices, dozens of specialty departments, and multiple imaging centers. Here, the entire mission revolves around seamless care coordination. A patient might see their family doctor, get a referral to a cardiologist, and then head to a radiologist—all within the same network. Their information has to follow them, instantly and securely, at every step.
The Deciding Factor: Collaboration
In the hospital network scenario, an EMR would create frustrating and even dangerous information silos. An EHR, on the other hand, is the absolute bedrock of the whole operation. It’s what allows the cardiologist to instantly see the primary physician’s notes and ensures the radiologist's report is available to everyone on the care team, all inside one unified patient file. That’s the real power of interoperability in motion.
So, the EMR vs. EHR question really boils down to your operational scope. Are you an island, or are you part of a larger healthcare archipelago?
The decision isn't just about technology; it’s a strategic choice about the kind of care you want to deliver. An EMR supports efficient, isolated encounters, while an EHR empowers a collaborative, continuous care journey.
This is exactly why our work at PYCAD is so intertwined with the power of modern EHRs. We build custom web DICOM viewers and integrate them into medical imaging web platforms—a job that depends on the kind of open, shareable architecture that an EHR offers. Seeing how these systems work together is key, and you can see real examples of our integration work on our portfolio page.
Beyond Practice Size
Even for smaller, independent clinics, thinking about the future is critical. If a specialty practice has plans to build strong referral relationships with local hospitals or get involved in value-based care initiatives, starting with an EHR is a smart, forward-thinking move. It lays the foundation for future collaboration and makes sure the practice is ready to connect with the wider healthcare world when the time is right.
In the end, your decision should be driven by a clear vision for your patient data. Do you just need a digital filing cabinet for your own use, or do you need a living platform built for sharing, teamwork, and innovation? Answering that question will light the way forward for your organization.
A Practical Checklist for Your Platform Decision
Choosing the right platform is a long-term commitment. It’s about more than just ticking off features on a list; it’s about asking the deep, strategic questions that will define your future. To really grasp the difference between an EMR and an EHR for your organization, you need a solid framework for your evaluation.
This checklist is designed to steer those crucial conversations with vendors and your own team, making sure your choice is one that fuels tomorrow’s breakthroughs, not just gets you through today.
It all starts with an honest look at your collaborative world. Are you a standalone clinic, or are you constantly sharing patient information with hospitals, labs, and specialists across the street or across the country? That one question alone often points you in the right direction, cutting to the core difference between an inward-facing EMR and a connected, network-minded EHR.
Probing for Future-Readiness
Once you know your collaboration needs, it's time to dig into a system's technical horsepower. Don't just ask vendors if they support interoperability—ask them how. A truly forward-thinking platform is built on modern standards that don't just tolerate third-party integrations, they welcome them.
Here are the questions that really matter:
- API and Integration Capabilities: How robust and well-documented is your API? How easily can we plug in specialized tools, like our diagnostic software or a new patient engagement app?
- Commitment to Standards: What’s your roadmap for FHIR (Fast Healthcare Interoperability Resources)? How do you prove your platform will keep up as data standards evolve?
- Scalability and Data Handling: As our data and patient volumes grow, how does your system scale with us? What’s the plan for managing massive datasets and complex workflows? Getting this wrong is painful, so it helps to review established data migration best practices to see what’s involved.
The most important question isn't "What features does it have?" but rather, "What future does it enable?" A system with a locked-down architecture limits your potential, while one built on open standards invites limitless innovation.
This kind of deep inquiry is absolutely critical. For example, at PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms. That kind of work is only possible when an EHR provides the necessary API hooks and lives by modern interoperability standards. An old-school EMR just can’t play at that level. You can see what this looks like in practice on our portfolio page.
By pushing past the glossy feature sheets and focusing on foundational principles—true interoperability, scalability, and a vendor's real commitment to progress—you set your organization up to make a decision that will pay dividends for years to come.
Building Your Future-Ready Health Platform

The direction of healthcare is undeniable: the future belongs to systems that are connected, collaborative, and intelligent. The conversation has moved beyond the simple what is difference between emr and ehr and is now focused on how to architect a health platform ready for whatever comes next.
This journey almost always starts with a foundational choice: selecting the right EHR. An EHR’s native ability to share information creates the essential groundwork for a connected care ecosystem, acting as the central nervous system for all patient data.
Elevating Your EHR into an Intelligent Hub
But an EHR on its own is just the beginning. The real magic happens when you partner with specialists who can unlock its full potential. A standard system becomes extraordinary when you layer in purpose-built tools that simplify complex workflows and deliver much deeper clinical insights.
True advancement in healthcare technology isn't just about adopting a system; it's about transforming that system into a powerful, intelligent, and deeply integrated platform that serves clinicians and patients on a higher level.
At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms. This is our specialty—turning standard EHRs into dynamic, visually rich environments. Our work closes the gap between static patient records and critical diagnostic imaging, creating a unified clinical experience that's far more powerful.
We invite you to see what’s possible. Take a look at the advanced solutions we’ve delivered for our clients by exploring our work on our portfolio page.
Frequently Asked Questions
Diving into digital health records always brings up a few common questions. Let's clear up some of the most frequent points of confusion I hear from professionals trying to navigate the EMR vs. EHR landscape.
Can an EMR System Be Upgraded to an EHR?
The short answer is yes, but it’s rarely a simple software update. Think of it less as an upgrade and more as a complete system migration. Shifting from a siloed EMR to a connected EHR means moving your data to an entirely new platform designed from the ground up for interoperability. It's a strategic overhaul, not just a patch.
Which Is Better for a Small Solo Practice?
This really comes down to your long-term vision. An EMR can feel like the right fit for a small, standalone practice—it’s often more affordable and handles internal record-keeping just fine.
However, if you ever plan to collaborate with other specialists, join a larger network, or simply give your patients a more connected care experience, starting with an EHR is the smarter, forward-thinking investment.
Do Patients Have Access to Their EHR or EMR?
Patients don't get direct access to the backend system that clinicians use. Instead, their window into their health data is typically through a patient portal, which is a feature powered by the clinic's EHR.
The EHR is the comprehensive, authoritative source of truth for providers. The portal is a secure, curated view of that information designed specifically for the patient. Full system access is—and should be—strictly limited to authorized medical staff.
At the end of the day, the real difference between an EMR and an EHR boils down to one word: connectivity. An EMR is like a digital file cabinet for a single clinic. An EHR is a living, breathing health story that can securely travel with a patient wherever they receive care, paving the way for truly collaborative medicine.
Grasping this core distinction is the first step in choosing the right path for your organization. At PYCAD, we build custom web DICOM viewers and integrate them into medical imaging web platforms, a specialty that relies heavily on the solid, interoperable foundation that a modern EHR provides. You can see how these integrated systems come to life on our portfolio page.
The team at PYCAD can help you transform your healthcare platform. We build secure, advanced web DICOM viewers and integrate them with CRM and AI solutions to create powerful, unified systems.