Cutting healthcare costs isn't just about trimming budgets. If you want real, sustainable savings, you have to dig deeper. It's about being smarter with your financial planning, finding ways to make your operations more efficient, and embracing technology to build a system that delivers better value.
Taking a Hard Look at Healthcare Spending
Let's be honest: the old-school approach to cost management doesn't work anymore. You can't just make small tweaks or across-the-board cuts and expect to solve the problem. The truth is, healthcare spending is a tangled web of issues, from drug pricing and administrative bloat to the fundamental ways we deliver and pay for care. Simply put, we need a modern, all-encompassing strategy.
This guide will walk you through the core areas where you can make a meaningful impact. We're going to focus on four key strategies:
- Rethinking the Payment Model: Shifting from a "fee-for-service" system that pays for volume to a "value-based care" model that rewards better patient outcomes.
- Smarter Pharmacy Management: Getting a handle on pharmaceutical spending through better formulary design, embracing biosimilars, and carefully reviewing claims.
- Using Technology to Boost Efficiency: Tapping into tools like AI and automation to cut down on administrative work, smooth out workflows, and lower your operational overhead.
- Bringing Everyone to the Table: Getting providers and patients involved in making cost-conscious decisions by providing clear information and education.
Global Spending Gaps Put It All in Perspective
The challenge of controlling healthcare costs looks very different depending on where you are in the world. National economic strength plays a huge role. Take global public healthcare spending as a share of GDP, for instance. In 2022, only high-income countries managed to average above the 5% GDP benchmark for public health investment, coming in at 5.8%.
Compare that to spending in upper-middle (4%), lower-middle (2.4%), and low-income countries (1.2%), and you see a massive gap. This really highlights how different economic realities create unique hurdles for funding and cost control.
Tackling healthcare spending isn’t about doing less; it’s about doing things smarter. Lasting change comes from eliminating waste and focusing resources on what truly improves patient health.
When it comes to empowering individuals, tools like a healthcare procedure cost calculator are invaluable. They offer a clear look at potential charges, helping people make more informed financial decisions about their care.
For organizations that need a quick summary, the table below outlines the core strategies we'll be discussing. It’s a great way to see the main action items and their expected results at a glance.
Key Strategies for Reducing Healthcare Costs at a Glance
| Strategy Area | Primary Action | Expected Outcome |
|---|---|---|
| Financial Models | Transition to value-based payment | Improved patient outcomes at a lower total cost |
| Pharmacy Costs | Accelerate biosimilar adoption | Significant reduction in drug expenditures |
| Operations | Implement AI-driven automation | Decreased administrative waste and higher efficiency |
| Patient Engagement | Promote price transparency tools | Empowered patients making cost-effective choices |
These four areas represent the biggest opportunities for healthcare organizations to drive down costs while simultaneously improving the quality of care.
Moving from Volume to Value-Based Care

For decades, the American healthcare system has run on a fee-for-service engine. It’s a straightforward model: a provider performs a service, and they get paid for that service. More tests, more procedures, more appointments—it all translates to more revenue. The problem? This model rewards quantity over quality, often leading to higher costs without necessarily improving patient health.
This structure creates a cycle of reactive care, where the financial incentives are geared toward treating sickness rather than preventing it. To make a real dent in healthcare spending, we need to rewire the financial DNA of our system.
The answer for many is value-based care (VBC). This approach turns the old model on its head by tying reimbursement to patient health outcomes, not the number of services rendered.
The Core Principle of Value-Based Care
At its core, value-based care is about paying for positive results. It aligns the financial goals of providers with the wellness goals of their patients. When doctors and hospitals are rewarded for keeping people healthy, the entire focus of care delivery begins to shift.
This transition naturally encourages a more proactive mindset. It makes investing in preventive care, chronic disease management, and patient education a sound financial decision, because these are the very things that prevent expensive emergency room visits and hospital stays down the road. A hospital, for example, might launch a comprehensive diabetes management program to help patients avoid the severe complications that lead to costly interventions.
This isn't just a philosophical shift; the financial implications are massive. Moving toward value-based care could save the U.S. healthcare system nearly $1 trillion by 2025. By focusing on proactive care and better patient engagement, the model helps root out redundant tests and unnecessary procedures that bloat budgets. You can dig deeper into these financial projections and how VBC is set to reshape healthcare spending. Learn more about the potential savings from value-based care on cprcare.com.
Under a value-based model, a primary care physician's success is measured not by the number of office visits, but by the percentage of their diabetic patients who have their A1c levels under control. This is the new currency in healthcare.
Making this work requires building a completely new kind of infrastructure—one that's built on data, collaboration, and a patient-first mentality.
Building the Infrastructure for Success
Switching to value-based care is more than just a policy change; it requires a serious investment in technology, data analytics, and integrated care teams. Organizations need to build a foundation that can effectively track patient outcomes, manage the health of entire populations, and ensure seamless communication across different care settings.
A huge piece of this puzzle is predictive analytics. Health systems can finally use their vast amounts of data to identify high-risk patients before they become high-cost. For instance, an analytics tool might flag a patient with multiple chronic conditions who shows a high probability of hospital readmission. A care coordinator can then step in, making sure that patient has the right support, medications, and follow-up care to stay healthy at home.
A Real-World Scenario in Surgical Scheduling
Think about how this applies to a complex process like surgery scheduling. A hospital could analyze its historical data to forecast surgical demand, pinpoint bottlenecks in operating room availability, and allocate staff and resources more effectively. This doesn't just improve operational efficiency—it cuts costs tied to last-minute cancellations, staff overtime, and underutilized resources.
This level of coordination is simply impossible without the right tools. To succeed, organizations need:
- Electronic Health Records (EHRs) that actually talk to each other, sharing data across specialists and facilities.
- Population health management platforms to get a bird's-eye view of health trends across large patient groups.
- Telehealth capabilities to improve access to care, particularly for those in rural or underserved areas, while lowering overhead.
Overcoming Hurdles in the Transition
The road to value-based care has its bumps. One of the biggest is the significant upfront investment needed to upgrade technology, retrain staff, and redesign entire workflows.
Another major challenge is risk. In many VBC models, providers share financial risk with payers. If patient outcomes don't improve or if costs run higher than projected, the provider could face financial penalties. This demands a sophisticated approach to risk management and the ability to accurately forecast and manage costs for an entire patient population.
Despite these obstacles, the long-term payoff is undeniable. Health systems that have successfully navigated this transition report not only substantial cost savings but also higher patient satisfaction and better clinical outcomes. They get there by focusing on coordinating care, standardizing best practices, and truly empowering patients to become active partners in their own health. The journey takes commitment, but the destination—a sustainable, effective, and more affordable healthcare system—is well worth the effort.
Taking a Strategic Bite Out of Pharmaceutical Expenses
Pharmaceutical spending is a massive—and frankly, often frustrating—piece of the healthcare cost puzzle. For anyone involved, from health systems to patients, the constantly rising price tags on medications can feel like a runaway train.
But it's not an unsolvable problem. With a focused and strategic approach, you can get a real handle on this spending and unlock significant savings that are better used for direct patient care.
One of the most powerful tools in our modern cost-control arsenal is the biosimilar. If you're not familiar, think of a biosimilar as a high-quality, clinically equivalent version of a complex biologic drug. Biologics, often used for tough conditions like cancer or autoimmune diseases, are incredibly effective but come with astronomical prices.
Once the original patent on a biologic drug expires, biosimilars can enter the scene. They are rigorously tested to ensure they have no clinically meaningful differences from the original in safety or effectiveness. What they bring to the table is something that's been sorely needed: competition.
The Real-World Impact of Biosimilar Adoption
When a biosimilar becomes available, it immediately puts downward pressure on the brand-name drug's price while offering a much more affordable alternative. This isn't just theory; we're seeing it happen with blockbuster drugs like Humira and Stelara. As their biosimilar counterparts hit the market, they create immediate and substantial savings opportunities.
Adopting biosimilars isn't just a small tweak; it's a critical strategy for reining in drug spending. These alternatives are almost identical to the original biologics but can cost 80% or more less. Take Humira, for example. The uptake for its biosimilars jumped from a mere 3% to 28% in a very short time, thanks in large part to proactive health plans. You can explore the research on biosimilar adoption from pwc.com to see the full story.
The simple truth is that every time a provider prescribes a biosimilar instead of its more expensive brand-name counterpart, they are actively helping to reduce healthcare costs without compromising patient care.
To capture these savings, you need a solid game plan. It's not enough for biosimilars to simply exist on a shelf; health systems and payers have to actively encourage their use.
How to Accelerate Biosimilar Uptake
Getting providers and patients comfortable with biosimilars requires a coordinated effort. It's a mix of smart policy, clear education, and good communication.
Here are a few tactics that I've seen work time and again:
- Smart Formulary Management: Give biosimilars a preferred spot on your formulary. This usually means lower co-pays or fewer administrative hurdles (like prior authorizations) compared to the brand-name biologic. Make it the easy choice.
- Provider Education and Incentives: Many clinicians are just hesitant due to a lack of familiarity. Launch targeted education campaigns with the clinical data that proves biosimilar safety and efficacy. Some organizations even offer financial incentives to departments that hit biosimilar adoption targets.
- Clear Patient Communication: Patients need to hear, clearly and simply, that a biosimilar is not a "lesser" drug. Explain that it’s a clinically equivalent, more affordable option that will provide the exact same health benefit. This empowers them to be part of the solution.
To show just how dramatic the savings can be, let’s look at a quick comparison. The table below shows the potential financial shift when a biosimilar enters the market for a high-cost biologic.
Biosimilar Adoption Impact Analysis
| Biologic Drug | Annual Sales Example | Biosimilar Price Reduction | Impact on Total Costs |
|---|---|---|---|
| Humira | $18 Billion | 50-85% | Potential annual savings of billions for the health system. |
| Remicade | $5 Billion | 35-70% | Significant reduction in infusion therapy costs. |
| Neulasta | $3 Billion | 30-65% | Lowers supportive care costs for cancer patients. |
| Herceptin | $6 Billion | 40-75% | Makes a key breast cancer treatment more accessible. |
As you can see, the numbers are compelling. Actively promoting these alternatives is one of the most direct ways to lower pharmaceutical expenditures across the board.
Bolstering Your Pharmacy Cost Controls
Beyond biosimilars, you need other defenses against unnecessary spending. This is where smart utilization management and airtight review processes come in. It’s all about making sure the right drug gets to the right patient at the right time—and for the right reason.
Utilization Management Techniques
- Prior Authorization: This is a crucial checkpoint. Requiring pre-approval for certain expensive drugs ensures they are truly medically necessary and align with clinical best practices.
- Step Therapy: This is a common-sense approach. It simply means having a patient try a more affordable, but still clinically effective, drug first before "stepping up" to a pricier alternative.
- Quantity Limits: Placing limits on how much of a drug a patient can get within a specific timeframe is a simple way to prevent waste, stockpiling, and potential overuse.
Technology plays a huge role in making healthcare more efficient, and this applies to pharmacy management as well.
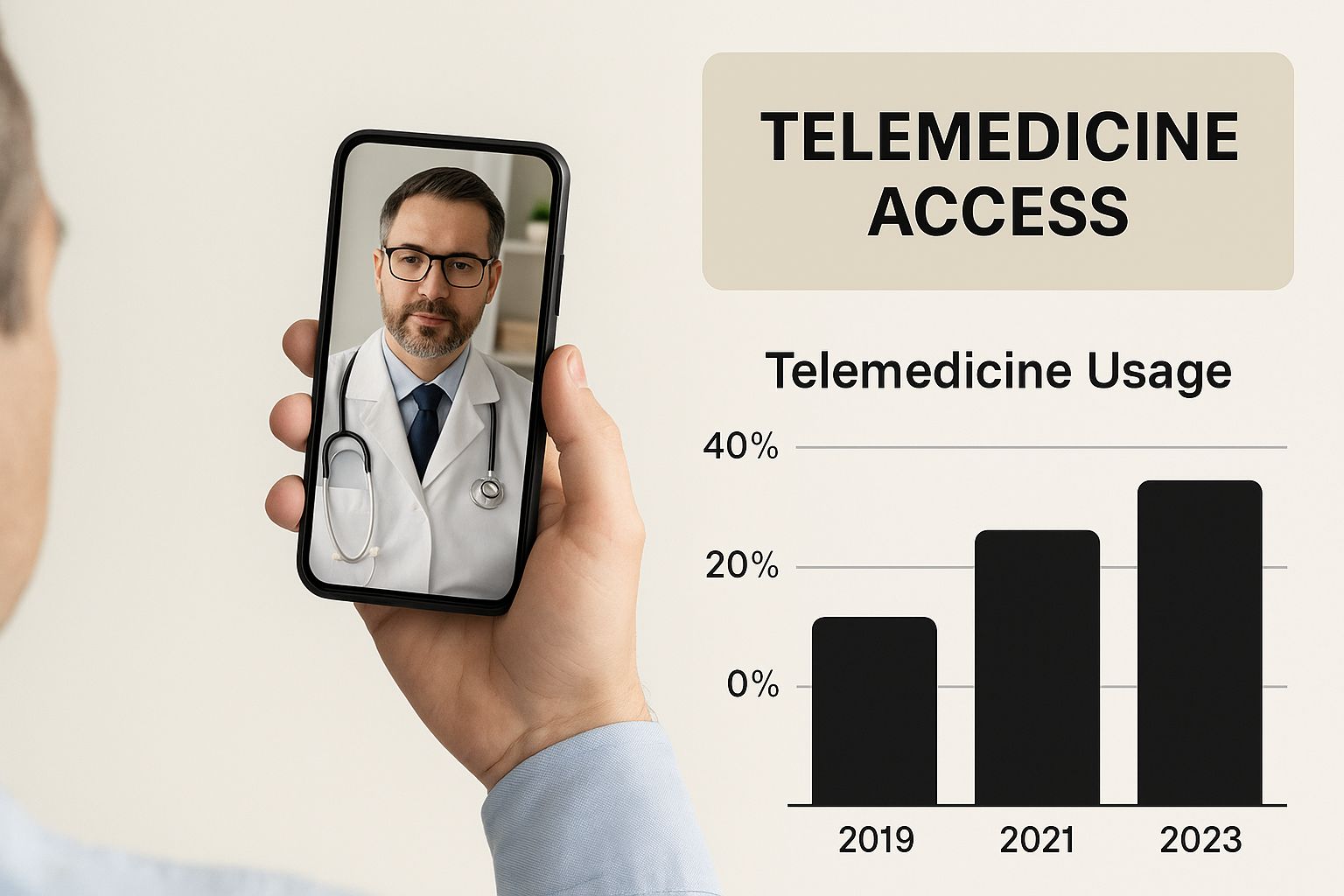
As the image shows, digital tools are becoming central to how care is delivered, creating new pathways for more efficient patient-provider interactions and resource management.
The Role of AI in Pharmacy Claims and Fraud Detection
Finally, let's talk about putting technology to work. Artificial intelligence can give your review process a massive upgrade. Manually reviewing claims is slow work and, let's face it, prone to human error. AI algorithms, on the other hand, can scan thousands of claims in seconds.
These systems are trained to spot red flags that might point to fraud, waste, or abuse. For instance, an AI could flag a pattern where a single pharmacy is dispensing an unusually high volume of a specific expensive drug, triggering an audit. It can also catch simple billing errors or duplicate claims that would have otherwise slipped through, saving millions over time.
By combining a smart biosimilar strategy with robust management and advanced technology, you can build a formidable defense against rising pharmaceutical costs.
Using Technology to Boost Operational Efficiency
In healthcare, technology is far more than just the latest buzzword. It’s a powerful tool that can cut through administrative red tape and seriously drive down operational costs. While telehealth often grabs the headlines, other innovations are quietly making healthcare more efficient and affordable. The real goal here is to let technology handle the mundane tasks, freeing up your expert staff to focus on what they do best: patient care.
Administrative waste is one of the biggest, yet quietest, drains on any healthcare budget. Think about all the time spent on medical coding, processing claims, and chasing down prior authorizations. These tasks are necessary, but they're also repetitive and ripe for human error. This is exactly where automation can make a world of difference.
When you automate routine administrative work, you're not just cutting labor costs. You’re freeing up thousands of hours that can be funneled back into patient-facing activities. This simple shift can boost both the quality of care and the morale of your team.
The business process automation benefits aren't just about speed, either. They bring a level of accuracy and operational insight that's incredibly valuable in the complex world of healthcare.
Automating the Administrative Backbone
Picture a billing department where an AI-powered system automatically vets every claim before it goes out the door. It instantly flags potential coding errors, cross-references them with the latest regulations, and confirms all the right documents are attached. This one change can slash claim denials—a huge source of lost revenue and frustrating rework.
A perfect real-world example is the prior authorization nightmare. Instead of your staff spending hours on hold with insurance companies, an automated system can manage the initial submission and tracking. It pulls clinical data directly from the EHR, fills out the forms, and submits them electronically. Your team only steps in for tricky cases or appeals, freeing them from a massive administrative headache. This directly cuts healthcare costs by reducing labor expenses and speeding up the entire revenue cycle.
This kind of automation brings a new level of predictability and efficiency to your financial operations, a crucial piece of any cost-reduction strategy.
Predictive Analytics for Smarter Operations
Going beyond administrative work, AI and machine learning are giving us incredible foresight into clinical operations. Health systems are now using these tools to predict patient flow, manage hospital bed capacity, and build smarter staffing schedules.
Imagine your emergency department on a chaotic Friday night. A predictive analytics platform can analyze historical admission data, check local event schedules, and even monitor public health trends to forecast patient surges with surprising accuracy. This allows hospital leaders to adjust staffing on the fly, ensuring enough doctors and nurses are on hand without the wasteful overstaffing that happens on quieter nights.
Optimizing Bed Management
One of the most powerful applications we're seeing is in bed management. An AI model can predict when a patient is likely to be discharged, which helps coordinate housekeeping and get rooms ready for incoming patients much faster. This reduces wait times for admitted patients and ensures every available bed is used effectively—a key driver of hospital efficiency and financial health.
Here’s a quick look at how these tools are making an impact across different areas:
- Surgical Scheduling: AI can juggle surgeon preferences, equipment availability, and patient data to create optimized OR schedules that minimize downtime and maximize the number of procedures.
- Supply Chain Management: Predictive analytics can forecast the demand for medical supplies, helping you avoid both stockouts of critical items and wasteful over-ordering.
- Staffing and Rostering: Machine learning can generate fair and efficient staff schedules that meet patient demand while respecting employee preferences, which helps cut down on burnout and costly overtime.
The Tangible Return on Investment
Yes, implementing this technology requires an upfront investment. But from what I've seen, the return is often fast and significant. One large hospital network that rolled out an AI-powered patient flow system reported a 15% reduction in patient wait times and a 10% increase in patient throughput within the first year alone. Those operational gains translated directly into millions of dollars in cost savings and new revenue.
The benefits aren't just on the balance sheet, though. When nurses and administrative staff are freed from tedious paperwork and constant operational firefighting, they report much higher job satisfaction and lower burnout rates. This leads to a more stable, engaged workforce, which is truly priceless when it comes to delivering high-quality patient care. By investing in technology that makes your team's day-to-day work smoother, you're also investing in your most important asset: your people.
Create a Culture of Cost-Consciousness

Lasting cost control isn't just about implementing new software or sending out top-down memos. It's about building a mindset where every single person on your team—from the scheduling desk to the operating room—gets how their daily actions impact the bottom line. This is the human side of the equation, and frankly, it's where the real magic happens.
When financial stewardship becomes part of your organization's DNA, efficiency stops being an abstract goal. It turns into a shared responsibility, something that's baked right into daily decisions and clinical workflows.
Give Your Team the "Why"
This kind of cultural shift always starts with education. Your team needs to understand the reasons behind any cost-saving initiatives. This isn't about micromanaging supply closets; it’s about connecting individual actions to the bigger picture of patient affordability and the long-term health of the organization.
For example, you could hold a quick training session showing how standardizing a specific brand of surgical gloves saves the facility $50,000 a year. Then, you show them that this exact amount is being reinvested into a new patient monitoring system everyone has been asking for. Suddenly, staff see their small changes funding real, meaningful improvements, and they become partners in the process.
Standardize Clinical Pathways to Cut Down on Waste
If I had to point to one of the biggest money drains in healthcare, it’s unwarranted variation in care. When you have five different physicians treating the same exact condition in five completely different ways, you inevitably end up with a mix of unnecessary tests, procedures, and prescriptions. It’s costly and inconsistent.
The most direct solution here is to develop and implement standardized clinical pathways. These are evidence-based roadmaps that outline the most effective and efficient course of treatment for common conditions. They don't strip clinicians of their professional judgment, but they do provide a clear, proven framework that cuts out the waste.
By standardizing pathways for conditions like community-acquired pneumonia or joint replacements, a health system can significantly reduce average length of stay and supply costs per case, directly improving the bottom line while ensuring consistent, high-quality care.
This approach ensures every patient receives care that's rooted in best practices. As a natural result, costs go down because you're focusing resources exactly where they'll have the most impact.
Get Smarter With Your Supplier Contracts
Your supply chain is a goldmine for potential savings, yet it's often overlooked. Too many facilities get stuck in a rut of passive purchasing, just reordering from the same suppliers year after year without ever questioning the terms.
It’s time to get proactive. Equip your procurement team with hard data on your purchasing volume and current market prices. When you can walk into a negotiation and show a vendor that your hospital system buys 10,000 units of a particular catheter every year, you gain immense leverage to secure better pricing. It’s that simple.
Don't shy away from group purchasing organizations (GPOs) or consolidating your vendors to boost your buying power. I’ve seen facilities save a fortune with a simple change, like switching from three different vendors for cleaning supplies to a single, high-volume contract. The savings can be immediate and substantial.
Bring Patients into the Conversation
Finally, let’s talk about your most underused asset in cost control: the patient. An informed, engaged patient is one of your greatest allies in this effort. The foundation for this is price transparency. Giving patients clear, upfront estimates for procedures allows them to make decisions that work for them financially.
Beyond just pricing, focus on creating a true partnership with patients.
- Boost Health Literacy: Take the time to educate patients about their conditions and treatments in plain, simple language. A patient who truly understands their medication regimen is far more likely to stick with it, preventing expensive complications down the road.
- Embrace Shared Decision-Making: When it's clinically appropriate, talk openly about the costs and benefits of different treatment options. A patient might happily choose a highly effective generic drug over a pricey brand-name one if they understand it won't compromise their outcome.
- Champion Preventive Care: Get loud about annual check-ups, screenings, and lifestyle management. Every chronic condition you help a patient prevent represents a massive long-term cost avoided—for both them and the system.
When you empower your team, standardize your key processes, negotiate like you mean it, and truly partner with your patients, you create a powerful, self-sustaining culture of cost-consciousness. This is the foundation that makes every other strategy work.
Answering Your Top Questions About Healthcare Cost Reduction
Even with the best plan in hand, real-world questions always pop up. Let's tackle some of the most common hurdles you might face when trying to trim your healthcare organization's budget. Think of this as a quick, practical Q&A session based on years of experience in the field.
As a Smaller Clinic, Where Do I Even Begin?
If you're running a smaller practice or hospital, you don't have the luxury of a massive budget for a complete overhaul. That's okay. The key is to start with the low-hanging fruit.
Take a hard look at your administrative tasks. Are you drowning in paperwork for things like patient scheduling or billing? Moving those processes to a basic practice management system can be a game-changer, freeing up your staff's time and cutting down on expensive manual errors.
Another great starting point is your supply cabinet. Dig into your purchasing history for medical supplies and pharmaceuticals. You’ll likely spot opportunities to save by buying in bulk or simply renegotiating with your current vendors. These foundational steps create momentum and build a solid base for bigger projects down the road.
How Can We Cut Costs Without Sacrificing Patient Care?
This is the million-dollar question, and it’s the most important one to get right. Let's be clear: the goal isn't to slash services. It's to surgically remove waste and inefficiency. To do this, you need to adopt a value-based mindset, where every dollar spent is weighed against its impact on patient outcomes.
Before you change a single thing, use your data. Model how a potential cut could affect key quality metrics, from readmission rates to patient satisfaction scores. And whatever you do, bring your clinical team into the conversation from day one. Their on-the-ground experience is priceless.
For instance, standardizing the clinical pathways for common conditions like pneumonia or hip replacements is a perfect example. It ensures every patient gets top-tier, evidence-based care while naturally weeding out redundant tests and procedures. The focus shifts to smarter spending, not just less spending.
When you ground every cost-saving initiative in solid clinical evidence, you'll find that financial stability and patient well-being improve together.
What Is the Patient's Role in All of This?
Patients aren't just bystanders; they can be powerful allies in this effort. Their involvement often starts with something simple: preventive care. Regular check-ups, staying on top of vaccinations, and actively managing chronic conditions can head off far more complex and costly health issues down the line.
They can also become savvier healthcare shoppers. When a procedure isn't an emergency, price transparency tools can help them compare costs between different facilities. We should also encourage them to ask about generic or biosimilar drug options. A single question to their doctor about a brand-name prescription could easily save hundreds of dollars.
Finally, patient adherence is huge. When patients stick to their treatment plans and keep the lines of communication open with their providers, they reduce the risk of expensive complications and readmissions. An empowered patient is a partner in creating a more affordable and effective healthcare system for everyone.
At PYCAD, we see firsthand how technology can make healthcare more efficient. Our AI-driven medical imaging tools help organizations improve diagnostic accuracy while optimizing workflows. It's all part of building a smarter, more sustainable approach to cost management. See how we're pushing the boundaries of medical imaging at our official PYCAD website.






