Let's get right to the heart of the matter: will AI replace radiologists?
The short answer is a definitive no. The real story unfolding in clinics and hospitals isn't one of replacement, but of powerful partnership. AI is stepping in not as a competitor, but as an incredibly capable assistant, giving radiologists the tools to perform their work faster and with greater accuracy than ever before.
AI in Radiology: A Partner, Not a Replacement
The future is all about augmentation. It’s about combining the best of human intuition with the best of machine precision.

For a while, the idea of artificial intelligence taking over complex human jobs created a lot of noise. Because radiology is so deeply rooted in digital imaging and pattern recognition, it naturally became a focal point for this anxiety.
But what's actually happening on the ground is far more inspiring. We're witnessing a powerful synergy between human intellect and machine intelligence. Think of AI as a tireless assistant, one that can sift through mountains of data to spot the faintest patterns or handle routine tasks automatically. This frees up radiologists to pour their expertise into what really matters: solving complex diagnostic puzzles and making critical decisions for their patients.
From Prediction to Partnership
Back in 2016, a now-famous prediction claimed that radiologists would be obsolete within five years. Well, here we are, and the field is stronger than ever. The prediction completely missed the mark.
Instead of a takeover, we've seen an evolution. AI has become an essential collaborative tool that supercharges the radiologist’s workflow. In fact, surveys show that 85% of radiologists are optimistic about AI's ability to improve patient outcomes by taking on repetitive tasks and helping manage the ever-growing demand for imaging services worldwide. The conversation has shifted from "us vs. them" to "how can we work together?"
This shift isn't unique to medicine. It's a key part of the broader discussion around AI's potential to transform job roles across all industries.
The true value of AI isn't in its ability to work alone, but in its capacity to elevate the skills of the human expert. It's about creating a diagnostic team where technology provides data and the radiologist provides wisdom.
For years, the conversation was dominated by fears of obsolescence. Let's look at how the narrative has completely flipped.
AI's Role in Radiology: A Shift from Replacement to Augmentation
| Area of Concern | Initial Fear (Replacement) | Current Reality (Augmentation) |
|---|---|---|
| Diagnostic Authority | AI would make final diagnoses, rendering radiologists unnecessary. | AI acts as a "second reader," flagging potential issues for human review. |
| Workflow Efficiency | AI would automate the entire reading process from start to finish. | AI automates tedious tasks like measurements, freeing up radiologists for complex analysis. |
| Job Security | The profession of radiology would shrink or disappear entirely. | The demand for radiologists is growing, with AI helping to manage the increasing workload. |
| Skill Relevance | Traditional radiological skills would become outdated. | Radiologists' core skills are enhanced, now including the ability to manage and interpret AI outputs. |
This table shows a clear trend: AI isn't pushing radiologists out; it's elevating their practice and making them more effective than ever before.
This partnership is where we come in. At PYCAD, we specialize in building the digital infrastructure that makes this human-AI collaboration seamless. We develop custom web DICOM viewers and integrate them into medical imaging web platforms, ensuring that AI-driven insights are presented clearly and intuitively, right where the radiologist needs them.
You can see how we put these principles into practice by exploring our portfolio page.
The Reality of AI in Medical Imaging Today
If you really want to understand where AI fits into medicine right now, don’t picture a robotic doctor. Instead, think of it as a brilliant but incredibly specialized apprentice. It can perform specific, repetitive tasks with superhuman speed, but it doesn't have the deep, holistic wisdom of a veteran radiologist who has spent a career honing their craft. Getting this distinction right is key to seeing past the hype and understanding what AI can actually do in a clinic today.
The AI we have now is essentially a master of pattern recognition. We train these algorithms on massive libraries of images, teaching them to spot very specific, known abnormalities. An AI tool can, for example, sift through thousands of chest CT scans and flag potential lung nodules faster and more consistently than any human. It’s built for that kind of narrow, well-defined job, and it’s very, very good at it.
But that very strength reveals its biggest weakness. These models are only as smart as the data they learned from. They shine when identifying common conditions that were heavily represented in their training sets. In other words, they’re experts in the expected.
From the Lab to the Clinic
One of the toughest challenges for AI in radiology is bridging the gap between a pristine lab environment and the messy, unpredictable reality of a hospital. In research papers, AI models are often tested on clean, perfectly curated datasets, where they can post accuracy rates that look like they're ready to take over the world.
But clinical practice is anything but clean and standardized.
- Varying Equipment: The images from one MRI or CT machine can look vastly different from another, even if they're the same brand in different hospitals.
- Patient Diversity: Real-world patients bring an incredible mix of ages, body types, and pre-existing conditions—all variables that might be completely new to the algorithm.
- Unexpected Findings: A patient might be getting a scan for a suspected kidney stone, but the radiologist spots an incidental, completely unrelated tumor on the adrenal gland. That requires a totally different kind of thinking.
These real-world curveballs can make an AI's performance plummet. An algorithm that boasts 95% accuracy in a controlled study might suddenly drop to 75% accuracy when it’s put to work in a live hospital setting. This is exactly why the "AI vs. radiologist" debate misses the mark. The technology simply isn't robust enough yet to handle the sheer unpredictability of human health on its own.
The Power of Clinical Context
Even beyond the technical side, today’s AI is missing the single most important piece of the diagnostic puzzle: clinical context. A radiologist doesn't just see pixels on a screen. They are master synthesizers, pulling together information from everywhere to build a complete picture of a person's health.
A radiologist’s interpretation is an intricate blend of visual analysis, patient history, knowledge of disease progression, and collaboration with other physicians. AI can analyze the image, but it cannot yet replicate this deep, contextual understanding.
Think about it: an ambiguous spot on a liver scan means one thing for a patient with a history of cancer and something entirely different for a healthy patient with no relevant medical history. That ability to weigh the evidence, integrate seemingly unrelated facts, and apply years of experience is the true art of medicine. It’s where human judgment turns raw data into a life-saving diagnosis.
This is precisely why seamless workflow integration is so critical. Here at PYCAD, we know that an AI insight is useless if it doesn't fit naturally into this complex diagnostic process. We build custom web DICOM viewers and integrate them directly into medical imaging platforms. Our solutions are designed to present AI findings not as a jarring, separate alert, but as an intuitive layer of information that enhances what the radiologist already sees. You can see how we bring this to life by checking out our portfolio page.
Ultimately, AI today is an incredible tool for detection and quantification. It can measure tumors, segment organs, and flag common issues, freeing up radiologists from tedious, time-consuming work. But it still falters with the rare, the unexpected, and the nuanced cases where nothing can replace human expertise. The reality isn’t replacement; it’s a sophisticated partnership where technology handles the routine, freeing human experts to focus on the challenges that truly demand their skill.
How AI is Being Adopted in Clinical Settings
If you think AI in radiology is some far-off future, think again. It’s here, it’s happening now, and it’s moving at a pace that’s frankly stunning. This isn't a theoretical concept anymore; these are powerful tools being rigorously tested, validated, and cleared for clinical use every single day. The sheer volume of approved algorithms shows that radiology is leading the charge in medical innovation, embracing technology that delivers real, tangible value.
The numbers don't lie. By mid-2025, the U.S. Food and Drug Administration (FDA) had already given the green light to roughly 873 AI algorithms for medical devices. Radiology is completely dominating this space, accounting for a massive 78% of all new AI device approvals in early 2025. That momentum is only accelerating—we saw 115 new radiology AI algorithms cleared in the first half of the year alone, a growth of over 15% from the end of 2024. This wave of regulatory acceptance is the clearest signal yet that the technology is mature and ready for the clinic. If you want to dive deeper into what it takes to get that approval, our guide on the FDA medical device approval process breaks it down.
These tools aren't just sitting in research labs, either. Industry leaders are pushing them into the real world where they can actually make a difference, moving AI from a promising idea to a life-changing reality.
From Algorithm to Action
Getting from a brilliant algorithm to a tool that saves lives is a journey paved with intense regulatory scrutiny. Every single FDA approval is a major milestone, a confirmation that an AI tool is both safe and effective for its specific job. This is the bedrock of trust that allows clinicians and entire healthcare systems to confidently bring these technologies into their daily practice.
Look at a company like Viz.ai for a perfect example of this in action. Their AI system, now active in over 1,600 hospitals across the globe, analyzes brain scans for signs of stroke and automatically alerts specialists in real-time. What’s the result? They’ve slashed patient processing times by an average of a full hour.
It's not just about doing one thing faster. In a stroke case, saving an hour can be the difference between a patient walking out of the hospital and facing a lifetime of disability. That’s the real human impact of clinically-approved AI.
This is what it looks like when validated AI tools stop being just code and start revolutionizing how we deliver care.
Building the Foundation for Integration
With this flood of approved AI tools, we're facing a new, exciting challenge: how do we actually get them to work smoothly within the chaotic daily workflow of a hospital? An FDA-cleared algorithm is a powerful thing, but it’s only valuable if its insights are delivered to a radiologist clearly, intuitively, and at the right moment. Making that happen—that seamless integration—is the next great frontier.
This is exactly the gap we bridge at PYCAD. We specialize in building custom web DICOM viewers and integrating them into medical imaging platforms. Our entire focus is on making sure that AI-generated data, whether it's a heatmap showing a suspicious lesion or a precise volumetric measurement, feels like a natural extension of the radiologist's own workflow. The tech needs to feel like a trusted partner, not another annoying pop-up.
This kind of thoughtful integration is what transforms a bunch of separate AI tools into a single, cohesive system that supports better, faster, and more confident decisions. You can see how we bring this vision to life by checking out the projects on our portfolio page. As more and more tools get the FDA's nod, the need for this kind of expert integration is only going to skyrocket, cementing AI’s place as a truly indispensable part of modern medicine.
Bringing AI Insights into the Clinical Workflow
A brilliant AI algorithm is a powerful engine, but without a steering wheel and a clear dashboard, it’s just noise. For artificial intelligence to truly elevate the field, its insights must flow seamlessly into the radiologist's hands in a way that feels intuitive, not disruptive. This integration is where the abstract promise of AI meets the practical reality of patient care.
This very challenge—embedding complex data into a fast-paced clinical environment—is exactly what we at PYCAD are built to solve. We build custom web DICOM viewers and integrate them into medical imaging web platforms, transforming AI from a separate, clunky tool into an organic extension of the radiologist’s own expertise.
The journey from a promising research model to a trusted clinical tool is a rigorous one. It’s a multi-stage marathon involving validation, regulatory approval, and finally, hospital adoption.
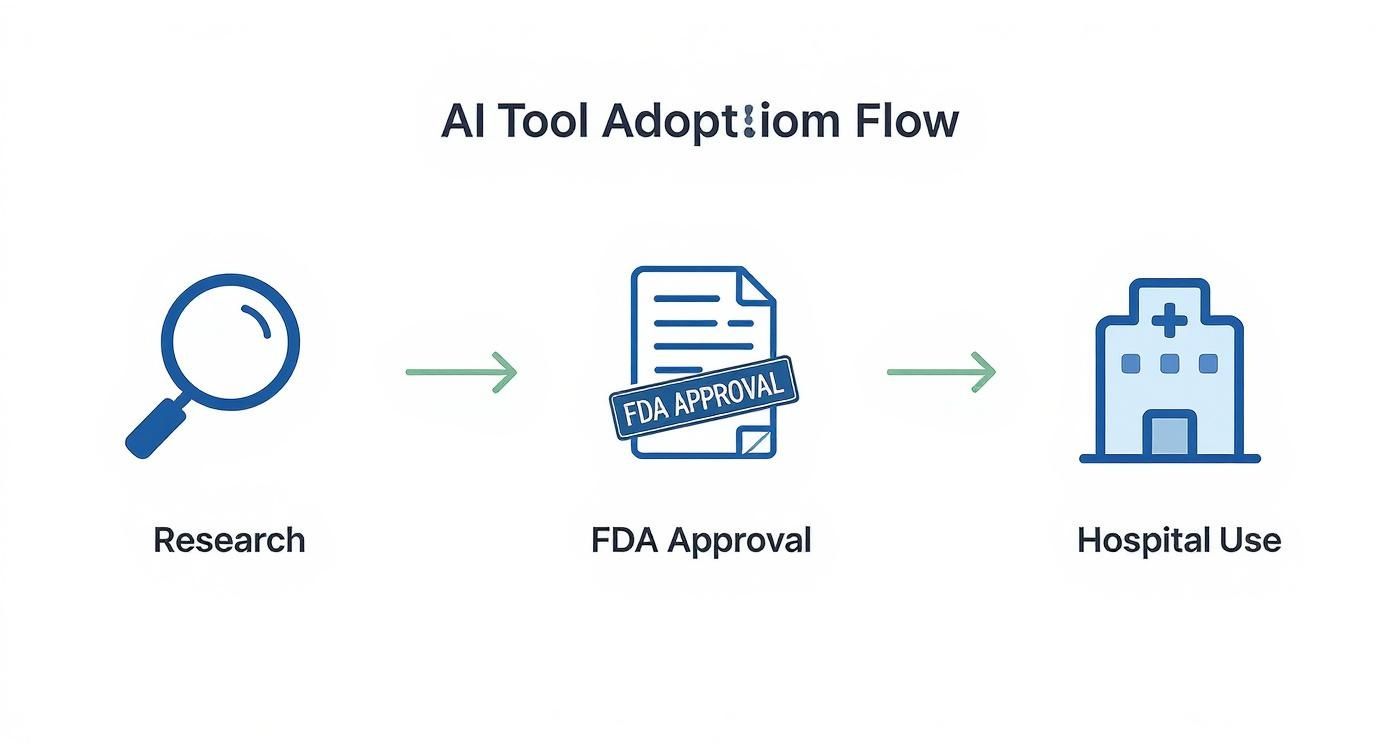
This meticulous process ensures that by the time an AI tool reaches the clinic, it has been thoroughly vetted for both safety and effectiveness.
From Data Points to Diagnostic Clarity
Picture a radiologist examining a CT scan. Instead of toggling between different applications or deciphering a separate report from an AI, they see everything in one unified view. Our custom viewers make this a reality by overlaying AI-generated heatmaps, segmentations, and measurements directly onto the original images.
A potential tumor isn’t just flagged; it’s highlighted with a precise boundary. A critical measurement isn't buried in a table; it’s annotated right on the scan. This approach doesn't just add information—it creates clarity and builds confidence, allowing radiologists to verify and interpret AI findings in a single glance.
The goal isn't just to present AI results. It's to weave them so deeply into the diagnostic fabric that they feel like a natural part of the radiologist's own vision, enhancing their ability without interrupting their focus.
This level of deep integration is essential for turning raw computational power into actionable medical wisdom. It’s what prevents "alert fatigue" and ensures the most critical information always rises to the top.
Creating an Intelligent Diagnostic Cockpit
The modern reading room is evolving. It's becoming less of a simple workstation and more of an intelligent diagnostic cockpit. In this environment, the radiologist is the expert pilot, and various systems—including AI—provide the critical data needed to navigate complex cases safely and efficiently.
A key piece of this puzzle involves tools like Clinical Decision Support Systems (CDSS), which act as intelligent co-pilots. These systems help synthesize patient data, AI findings, and clinical guidelines to support better, faster decision-making.
This holistic approach means getting several key components to work in perfect harmony:
- Picture Archiving and Communication System (PACS): The central vault for all medical images.
- Radiology Information System (RIS): The system that manages patient data and scheduling.
- AI Algorithms: The specialized engines that analyze images for specific findings.
- The DICOM Viewer: The critical interface that brings it all together for the radiologist.
When these elements are perfectly synchronized, the workflow becomes fluid and incredibly powerful. For those interested in the nuts and bolts of making this happen, diving into https://pycad.co/radiology-workflow-optimization/ offers deeper insights into making this integration a success.
Ultimately, when you see this collaborative model in action, the question of "will AI replace radiologists?" starts to feel irrelevant. The technology isn’t taking over; it’s providing a more advanced set of instruments. It’s the radiologist’s skill, experience, and critical judgment that remain firmly in the pilot's seat, guiding the diagnostic journey from start to finish. The future is a partnership, and building the perfect interface for that partnership is the key to unlocking its true potential.
Why Radiologist Demand Is Still Growing
https://www.youtube.com/embed/rZRUpJx4Kug
It seems like a paradox, doesn't it? With all the talk about artificial intelligence, you’d think the need for human radiologists would be shrinking. But what’s actually happening in hospitals and clinics tells a much more interesting story: the demand for skilled radiologists is stronger than ever.
This isn't just a gut feeling. The numbers paint a clear picture of a profession that's expanding, not contracting. Job openings for radiologists are on the rise, and residency programs are growing to keep up. There are a couple of big reasons for this. First, the global demand for medical imaging is exploding. And second, today's AI tools are more like specialized assistants than all-knowing replacements.
So, the conversation is shifting. It's not about replacement anymore; it's about powerful collaboration. AI is becoming an essential partner, helping a stretched workforce handle a tidal wave of complex cases and deliver the best possible patient care.
The Reality of AI Performance in the Clinic
A major reason we still need human experts at the helm is the gap between how AI performs in a perfect lab versus a chaotic, real-world hospital. In a research paper, an AI model might look flawless, but its accuracy can take a hit when it confronts the messy reality of day-to-day clinical work.
Think about it—hospitals are anything but standardized. Scans come from different machines with different settings, patient populations vary wildly, and unusual findings are part of the daily grind. It's not uncommon to see an AI model's performance drop by as much as 20 percentage points when it moves from the training ground to a live clinical environment.
On top of that, most AI tools today are highly specialized. They're fantastic at spotting specific, common diseases, which make up about 60% of imaging models. But what about the other 40%? The vast territory of rare conditions, subtle abnormalities, and complex, multi-faceted cases remains the domain of the human radiologist. This is exactly why U.S. radiology residency programs offered a record-breaking 1,208 positions in 2025—to fill a very real, and growing, need.
More Imaging Means More Need for Expertise
There's another powerful force at play here. As imaging technology gets better and more affordable, we're simply doing more of it. Scans that were once only for emergencies are becoming a routine part of proactive healthcare.
This explosion in imaging creates a mountain of data, and every single pixel needs an expert eye. An AI can flag a thousand potential issues in a heartbeat, but it takes a radiologist to add the critical context. They're the ones who can distinguish a harmless cyst from a dangerous tumor and connect the dots with a patient's full medical history.
AI is helping to generate more data than ever before, which ironically increases the value of the radiologist's ability to provide wisdom, context, and a definitive diagnosis.
At PYCAD, we're right in the middle of this evolution. We build custom web DICOM viewers and integrate them into medical imaging web platforms, turning that flood of data into clear, actionable insights. Our goal is to empower radiologists, not sideline them. By making AI-driven information intuitive and easy to access, we help them confidently navigate higher caseloads. You can see our solutions in action by visiting our portfolio page.
The evidence is clear. The field isn't being automated into obsolescence; it's being supercharged. Radiologists are becoming the conductors of a sophisticated orchestra of data, with AI as their most powerful instrument. To dig deeper into how this is changing the game, take a look at our guide on the benefits of AI in radiology.
Building the Collaborative Future of Radiology
The whole "human versus machine" debate is yesterday's news. We're stepping into a far more exciting era, one focused on building the ultimate diagnostic team. The future of medical imaging isn't a showdown; it's a synergistic partnership.
Think of the radiologist as the expert pilot, with AI serving as an incredibly advanced co-pilot, navigating massive amounts of complex data with skill and speed.

This completely reframes the conversation. We're moving beyond asking "will AI replace radiologists?" and onto a much more constructive question: "How can we best prepare for this collaborative future?" The answer involves a new way of thinking and a new set of skills, transforming the radiologist from a solo image interpreter into a clinical data strategist.
Cultivating the Skills for Tomorrow
To really thrive in this new environment, the radiologists of tomorrow will need to become masters of a new domain, one that bridges the gap between deep medical knowledge and powerful technology. This isn't about becoming a programmer; it's about becoming the indispensable leader of a tech-enabled diagnostic process.
So, what does this new toolkit look like?
- AI Model Validation: Radiologists will need the savvy to critically assess an AI model's performance. They'll have to understand its strengths and, just as importantly, its blind spots within their own specific patient populations.
- Data Literacy: A solid grasp of the data used to train algorithms is non-negotiable. This is the key to correctly interpreting AI outputs and spotting potential biases before they cause problems.
- Workflow Integration Expertise: Knowing how to weave AI tools into the day-to-day clinical workflow is what will separate good from great. This is where efficiency gains and better patient outcomes are truly born.
This shift empowers radiologists to not just use AI, but to command it. It ensures that technology always serves the ultimate mission: providing outstanding patient care.
The most effective radiologists of tomorrow will be those who can blend their deep medical knowledge with a sophisticated understanding of AI, acting as the final arbiters of a powerful human-machine partnership.
This is the very vision that drives us at PYCAD. We are completely dedicated to building the tools that make this collaboration a reality. We build custom web DICOM viewers and integrate them into medical imaging web platforms, creating the kind of intuitive interfaces this new standard of care demands.
Our work is a call to action for everyone in healthcare. Let's focus our collective energy on building systems that truly empower our clinicians and amplify their invaluable expertise. By doing that, we can build a future where technology and humanity work in perfect concert to achieve better outcomes for every single patient.
You can see some of the innovative solutions we’ve brought to life on our portfolio page.
Common Questions, Expert Answers
As we navigate this new frontier where AI meets radiology, a lot of questions come to the surface. Let's tackle some of the most common ones to give you a clearer picture of what this partnership really looks like.
Which Areas of Radiology Will Feel the Biggest Impact from AI?
Right now, AI is making its biggest waves in high-volume, standardized imaging. We're talking about mammography, chest X-rays, and specific CT scans—like those used to spot a stroke or detect lung nodules.
These are the areas where we have massive, well-organized datasets, which are exactly what deep learning models need to learn effectively. But don't mistake this for a takeover. The final word, especially when dealing with unusual or complex cases, will always belong to the experienced human radiologist.
How Does a DICOM Viewer Fit into an AI-Powered Workflow?
Think of the DICOM viewer as the radiologist's cockpit. It’s where they interact with every medical image. When you introduce AI, this viewer becomes even more crucial. A modern, web-based DICOM viewer doesn't just show images; it overlays AI-generated insights—like heatmaps highlighting suspicious areas or precise segmentations—right on top of the original scans.
This is where the magic happens. The viewer turns abstract AI data into tangible, visual evidence, letting radiologists instantly confirm, question, or act on the findings without ever breaking their diagnostic rhythm.
This is exactly what we do at PYCAD. We specialize in building custom web DICOM viewers and integrating them seamlessly into medical imaging platforms, making sure the entire experience is intuitive and truly supports the radiologist's expertise.
How Can a Healthcare Organization Get Ready for AI?
Jumping into AI isn't just about buying new software; it's about preparing your entire ecosystem. To do it right, you need a solid, multi-step plan.
- Set Clear, Achievable Goals: First, decide what you want AI to accomplish. Is it about faster turnaround times for critical stroke cases? Or better detection rates for early-stage cancer? Be specific.
- Take Stock of Your Infrastructure: Next, look at your current IT setup. Can your PACS and network handle the increased data flow from AI algorithms? You have to make sure the foundation is strong enough to build on.
- Design for Real-World Workflows: It’s vital to bring your radiologists and technologists into the conversation from day one. Any new tool has to feel like a natural extension of their daily routine, not a clunky add-on.
- Create a Robust Validation Process: Finally, you need a system to test, validate, and continuously monitor how any AI model performs with your own patient population. This isn't a "set it and forget it" technology; it requires ongoing vigilance to ensure it remains safe and effective.
At PYCAD, our passion is building the platforms that make this collaborative future possible. We partner with medical device companies and healthcare IT teams to craft the seamless, intuitive workflows that allow AI to truly amplify clinical skill. To see how we turn these ideas into reality, feel free to explore our work on our portfolio page.






